Marginal Ulcer Perforation and Concurrent 360-degree Twisted Roux Limb Volvulus following Roux-en-Y Gastric Bypass: A Case Report
 by Brook E. Porter, BS; Lindsey E. Goldstein, MD, FACS, FASCRS; and Jeffrey E. Friedman, MD, FACS, FASMBS
by Brook E. Porter, BS; Lindsey E. Goldstein, MD, FACS, FASCRS; and Jeffrey E. Friedman, MD, FACS, FASMBS
Ms. Porter and Dr. Friedman are with the University of Florida, College of Medicine, Department of Surgery, Division of Metabolic and Bariatric Surgery in Gainesville, Florida. Dr. Goldstein is with the University and Florida and Malcolm Randall VA Medical Center in Gainesville, Florida.
Funding: No funding was provided.
Disclosures: Ms. Porter and Dr. Goldstein reports no conflicts of interest relevant to the content of this article. Dr. Friedman is a consultant for Ethicon, Inc., Somerville, New Jersey.
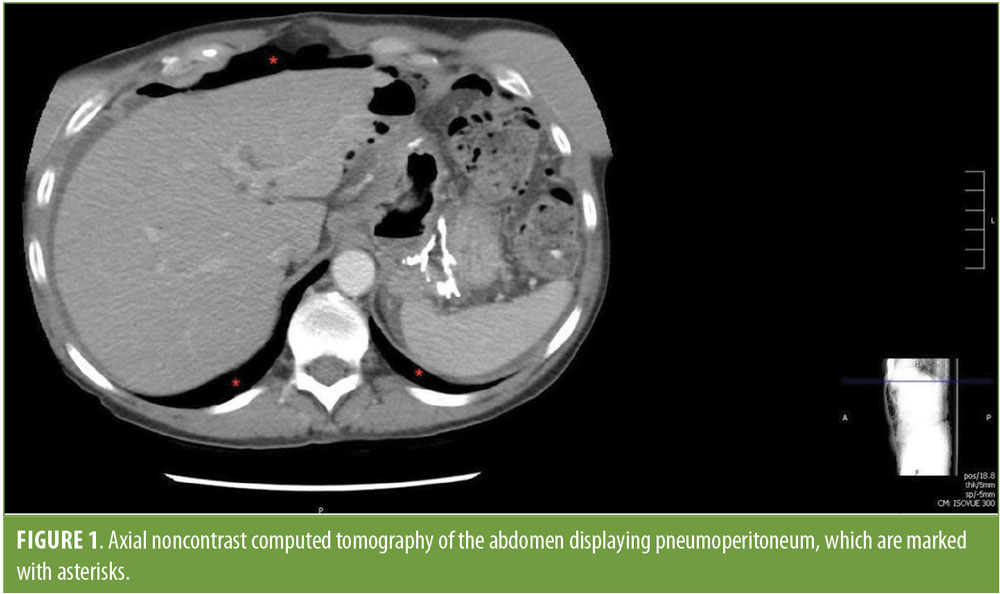
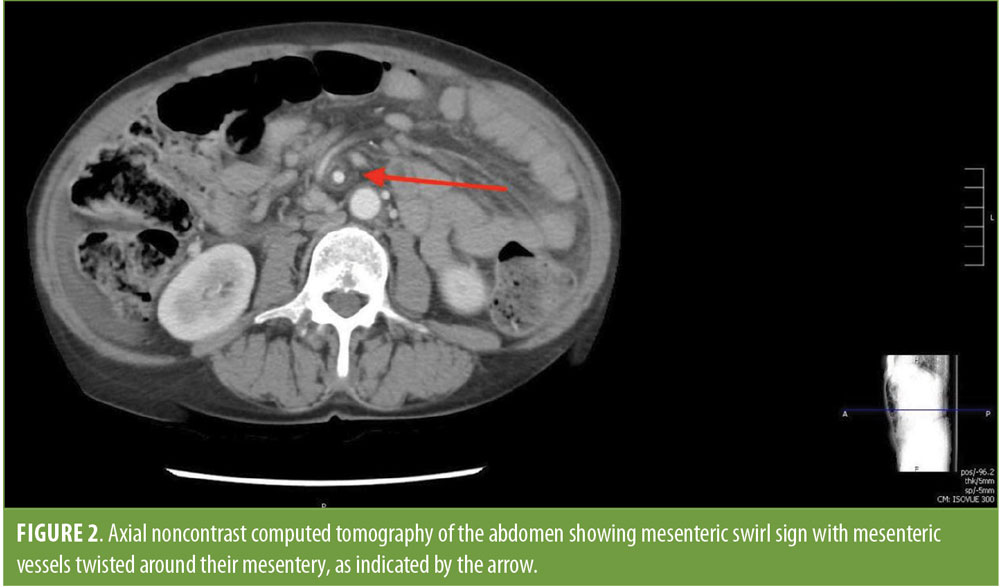
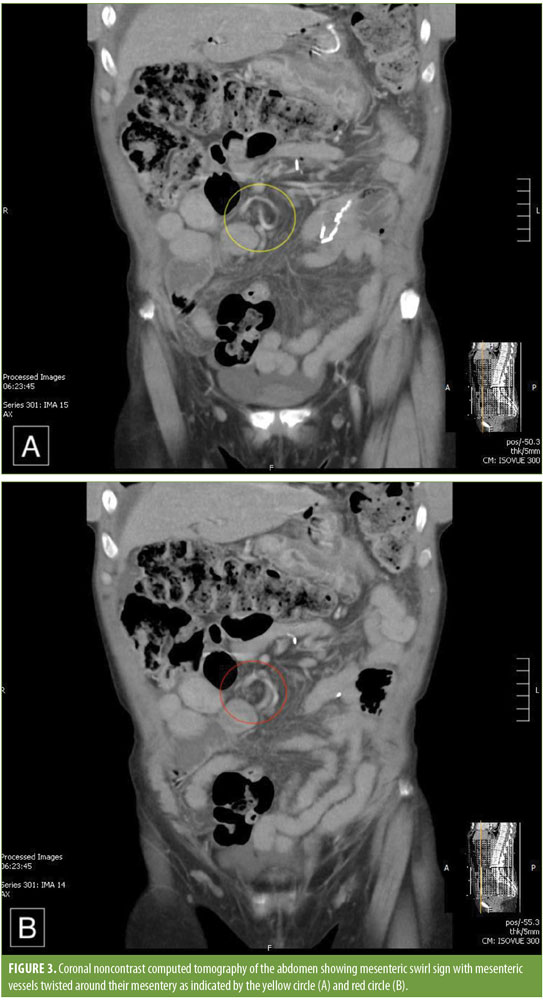
Abstract: Roux-en-Y gastric bypass is a common weight loss operation. A 360-degree twisting of the Roux limb around its mesentery is a technical error at the time of surgery and an uncommon complication of gastric bypass surgery. Patients with a twisted Roux limb often present early in the postoperative period with nausea, vomiting, dysphagia, and abdominal pain. Surgical correction is necessary. Marginal ulcer formation, a well-documented complication of this operation, similarly presents with nausea, vomiting, abdominal pain, and dysphagia, and it is often treated medically. Left untreated, marginal ulcers are at risk of perforation, which is a surgical emergency. We describe a patient who presented five years postoperatively from a gastric bypass with pneumoperitoneum consistent with a perforated ulcer and a mesenteric swirl on computed tomography scan. Upon exploration, the patient had a perforated marginal ulcer at the gastrojejunostomy anastomosis and a 360-degree twist of the Roux limb around its mesentery. It is crucial to run the Roux limb before and after construction to prevent twisting and other defects. This case highlights the importance of noncontrast computed tomography scan in assessing nonspecific gastrointestinal symptoms following Roux-en-Y gastric bypass as complications are not uncommon.
Keywords: Gastric bypass, Roux-en-Y, mesenteric swirl sign, marginal ulcer, volvulus, postoperative complications
Bariatric Times. 2019;16(6):16–17.
Laparoscopic Roux-en-Y gastric bypass (RYGB) is the gold standard in bariatric surgery for weight loss worldwide. Significant complications following RYGB include anastomotic leak, hemorrhage, bowel obstruction, anastomotic stricture, marginal ulcer, fistula, internal hernia, volvulus, dehydration, vitamin deficiencies, anemia, and fatigue.1–5 Of note, marginal ulceration, or ulceration at the gastrojejunal anastomosis, is one of the most common causes of abdominal pain after RYGB, with an incidence rate of 1 to 16 percent.1,5 Predisposing factors to marginal ulcers include technical errors; diabetes mellitus; hypertension; stress; recent surgery; and nonsteroidal anti-inflammatory drug (NSAID), alcohol, and tobacco use.1–2,6 A major complication of marginal ulceration is perforation, which has a 1- to 2-percent incidence rate in the RYGB patient population.6 Perforations present suddenly as immense, sharp, and diffuse pain that is made worse by movement, such as coughing or sneezing. The presence of free intraperitoneal air on computed tomography (CT) can indicate a perforated ulcer, which is a surgical emergency. If left untreated, a perforation can lead to sepsis and death.6 Volvulus also presents with abdominal pain, nausea, and vomiting. This can be difficult to diagnose; however, it can be visualized on CT by a mesenteric swirl sign.7 Intestinal volvulus causes serious morbidity and mortality, since it can lead to abdominal obstruction, ischemia, and infarction; thus, patients with high suspicion should undergo diagnostic laparoscopy to avoid catastrophic consequences.4
We present a patient with a history of RYGB five years prior at an outside facility who required emergent transfer to our facility due to an acute perforation of a marginal ulcer at the gastrojejunostomy. On arrival to the facility, imaging confirmed a mesenteric swirl sign, and a physical exam demonstrated peritonitis. We were initially suspicious that an internal hernia was the cause of both the swirl sign and her peritonitis. However, during laparoscopic exploration, we discovered a 360-degree twisting of the Roux limb, which required revision of her gastrojejunostomy.
Case Presentation
A 61-year-old woman with a history of peptic ulcer disease and hypertension presented to an outside emergency department complaining of worsening abdominal pain, nausea, vomiting, and shortness of breath. The patient had undergone RYGB surgery for morbid obesity at an outside hospital in 2012. Her preoperative body mass index (BMI) was 45kg/m2. The operation was reportedly uneventful. She was readmitted several times postoperatively with nausea, vomiting, and abdominal pain. Her surgeon was unable to find the source of her symptoms during these readmissions, so she became frustrated and stopped seeing him. Over the next several years, the patient became increasingly frustrated and depressed due to her chronic symptoms, so she started self-medicating with alcohol and tobacco to alleviate her pain. Consequently, she underwent multiple upper endoscopies through a gastroenterologist at a different hospital and was diagnosed with a marginal ulcer. She was started on an antacid (sucralfate) and a proton pump inhibitor (PPI) to treat her marginal ulcer. Despite this, her nausea, vomiting, and abdominal pain did not subside. On the morning of her presentation to our emergency department, she awoke with severe abdominal pain and shortness of breath. A noninfused CT scan of the abdomen performed at the transferring emergency department revealed pneumoperitoneum, suggesting marginal ulcer perforation (Figure 1). Additionally, the scan showed a mesenteric swirl sign, which we were concerned was a volvulus versus internal hernia (Figure 2). The patient was emergently transferred to the emergency department, where her abdominal exam was positive for generalized tenderness, rebound, guarding, and peritoneal signs. Following evaluation, she was emergently taken to the operating room for diagnostic laparoscopy. Laparoscopy revealed a perforated marginal ulcer of the anterolateral gastrojejunostomy. The gastrojejunostomy was densely adherent to the remnant stomach. Once the adhesions were lysed, it appeared that the marginal ulceration had perforated posteriorly as well; however, the remnant stomach sealed the posterior aspect of the ulcer. Overall, greater than 50 percent of the gastrojejunostomy had perforated, and the entire anastomosis was affected by the ulcer. The Roux limb was then run prior to reconstruction to evaluate the mesenteric swirl seen on CT and to rule out a volvulus or internal hernia of the small bowel. It initially appeared that the patient had an internal hernia through the Petersen’s defect because the defect was widely open with bowel through it. When the small bowel was run in its entirety, it became apparent that the Roux limb had been reconstructed incorrectly during her initial operation and was twisted around its mesentery. To confirm this diagnosis, the procedure was converted from laparoscopic to an open procedure, reaffirming that the Roux limb had been incorrectly reconstructed at the time of her initial RYGB five years prior. The stomach and Roux limb were divided proximal and distal to the anastomosis, resecting the perforated marginal ulcer. The Roux limb was detorsed, and the gastrojejunostomy was reconstructed. A feeding gastrostomy tube was placed in the remnant stomach. The patient tolerated the procedure well and was discharged without any complications four days later in good condition. She has done well since surgery and has quit drinking and smoking with consequent resolution of her nausea, vomiting, and abdominal pain.
Discussion
This case is unusual because the patient presented with two well-described complications of RYGB, perforated marginal ulcer and a concurrent twisted Roux limb. Most perforated ulcers occur within 18 months of RYGB, and rarely do they occur after 24 months.1,2 While there are few reported cases of twisted Roux limbs from improper reconstruction during RYGB in the literature, comparable surgical complications, such as internal hernias and improper Roux-en-O reconstruction, are considered early complications, often arising within two weeks of the initial RYGB surgery.8 Hence, the time frame of five years before presentation with the twisted Roux limb and the marginal ulcer is atypical.
Marginal ulcers following RYGB are not uncommon, with an incidence of 1 to 16 percent.5,6 The patient was at an increased risk of developing a marginal ulcer following RYGB due to her hypertension, recent surgery, and, most notably, technical error. Frustrated that her surgeon could not find the source of her nausea, vomiting, and pain caused by the twisted Roux limb from her initial surgery, the patient self-medicated with alcohol and tobacco use, which further increased her risk of ulceration. Ironically, when her ulcer perforated, this ultimately led to her definitive diagnosis of a twisted Roux limb, which was likely responsible for her chronic symptoms.
The patient presented to the emergency department with abdominal pain, nausea, and vomiting, which are consistent, yet nonspecific, symptoms of both a perforated ulcer and an obstructed Roux limb. She had a pre-existing diagnosis of marginal ulcer from a remote upper endoscopy. The positive peritoneal signs on physical exam, coupled with her history, further supported the diagnosis of a perforated ulcer. Endoscopy is a common method to diagnose marginal ulcers; however, this method would not necessarily detect a twisted Roux limb.9 Thus, it could have been easy to overlook the concurrent twisted Roux limb if it had not been for the preoperative CT scan. While the patient was readmitted several times after her initial surgery in 2012, her symptoms of nausea and pain were nonspecific to a twisted Roux limb, volvulus, or internal herniation. Without imaging, this posed a challenge to diagnose. The best predictor of internal hernia is the mesenteric swirl sign, which has a sensitivity of 61 to 100 percent and a specificity of 80 to 90 percent.10–15
Conclusion
Mistakes happen, but they are rarely reported. The present report demonstrates the importance of running the Roux limb prior to and after construction of the gastrojejunostomy during RYGB surgery to rule out twisting, internal hernias, and other preventable complications. Owns et al3 demonstrates that true twisting of the Roux limb from the initial RYGB only can be corrected by recreating the gastrojejunostomy because taking down the jejunojejeunostomy only can untwist the intestine but not the mesenteric blood supply.3 Additionally, noncontrast CT scan is a valuable tool to assess vague or nonspecific chronic abdominal pain following RYGB surgery because complications are not uncommon.
References
- Moon RC, Teixeira AF, Goldbach M, Jawad MA. Management and treatment outcomes of marginal ulcers after Roux-en-Y gastric bypass at a single high volume center. Surg Obes Relat Dis. 2014;10(2):229–234.
- Kalaiselvan R, Exarchos G, Hamza N, Ammori BJ. Incidence of perforated gastrojejunal anastomotic ulcers after laparoscopic gastric bypass for morbid obesity and role of laparoscopy in their management. Surg Obes Relat Dis. 2012;8(4):423–428.
- Owens M, Shukla H, Sczenpaniak J, Mahdavi A. Variations on bowel obstruction after gastric bypass and management of the twisted Roux limb. Surg Obes Relat Dis. 2013;9(6):1020–1021.
- Aman MW, Steele KE, Magnuson TH, et al. Intestinal complications after Roux-en-Y gastric bypass. Bariatric Times. 2015;12(4):14–18.
- Fringeli Y, Worreth M, Langer I. Gastrojejunal anastomosis complications and their management after laparoscopic Roux-en-Y gastric bypass. J Obes. 2015;2015:1–6.
- Coblijn UK, Goucham AB, Lagarde SM, et al. Development of ulcer disease after Roux-en-Y gastric bypass, indicence, risk factors, and patient presentation: a systematic review. Obes Surg. 2014;24(2):299–309.
- Fernandez-Moure J, Sherman V. Swirl sign—intestinal volvulus after Roux-en-Y gastric bypass. N Engl J Med. 2017;376(3):e3.
- Griffith PS, Birch DW, Sharma AM, Karmali S. Managing complications associated with laparoscopic Roux-en-Y gastric bypass for morbid obesity. Can J Surg. 2012;55(5):329–336.
- Widjaja D, Balar B. Shifting from normal to abnormal: transformation of clinical presentation of post-laparoscopic Roux-en-Y gastric bypass surgery complications. Can J Gastroenterol Hepatol. 2013;27(2):69–71.
- Goudsmedt F, Deylgat B, Coenegrachts, et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass: a correlation between radiological and operative findings. Obes Surg. 2015;25(4):622–627.
- Iannuccilli JD, Grand D, Murphy BL, et al. Sensitivity and specificity of eight CT signs in the preoperative diagnosis of internal mesenteric hernia following Roux-en-Y gastric bypass surgery. Clin Radiol. 2009;64(4):373–380.
- Lockhart ME, Tessler FN, Canon CL, et al. Internal hernia after gastric bypass: sensitivity and specificity of seven CT signs with surgical correlation and controls. AJR Am J Roentgenol. 2007;188:745–750.
- Corsino C, Harper H, Sieg V. “Swirl sign:”a case of abdominal pain after Roux-en-Y gastric bypass surgery. Clinic Pract Cases Emerg Med. 2018;2:270–271.
- Jamal M, Court O, Barkun J. Swirl sign. J Am Coll Surg. 2009;209:789.
- Qureshi UA, Fansur M, Qureshi SS. Swirl sign —ACT angiogram alarm sign or congenital transmesenteric hernias. J Coll Physicians Surg Pak. 2018;28:S13–15.
Category: Case Report, Past Articles







