Percutaneous Decompressive Jejunostomy for Treatment of Biliary Limb Obstruction After Duodenal Switch—Case Report
 by David F. Greenbaum, MD, FACS, and Gaurav Sharma, MD
by David F. Greenbaum, MD, FACS, and Gaurav Sharma, MD
Drs. Greenbaum and Sharma are with the Department of Bariatric Surgery, Virtua Memorial Hospital in Mount Holly, New Jersey.
Funding: No funding was provided.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: Duodenal stump blowout after duodenal switch surgery can be a major complication, if the patient gets small bowel obstruction. We present a case to discuss a less invasive way to prevent this complication in a hostile abdomen. This is a case of 37-year-old female who had conversion of gastric bypass to duodenal switch nine years ago. She presented with small bowel obstruction, for which she underwent exploratory laparotomy and resection of part of her biliary limb. She recovered from that operation and was discharged on post-operative day 5. She returns on post-operative day 8 with acute dilatation of proximal biliary limb. Since her abdomen is hostile at this point, we decided to get her proximal jejunum percutaneously decompressed by interventional radiologists. She recovered well and was discharged with the tube in place.
Keywords: Decompressive jejunostomy tube, duodenal switch, obesity
Bariatric Times. 2019;16(11):17–18.
Percutaneous gastrostomy as a temporary or definitive treatment for acute gastric dilatation in patients after gastric bypass surgery is a well-known treatment.1–4 It is used to decompress a grossly dilated stomach in the same way a nasogastric tube would be used if the stomach were still in continuity with the esophagus. It can relieve a closed loop obstruction and be life saving. It allows a physician to study the cause of the obstruction and facilitate a surgical correction of the problem, if necessary. The tube can then be removed two-to-three weeks later after the problem has resolved.
Patients who have undergone biliopancreatic diversion (BPD) with the duodenal switch (DS) do not have a bypassed stomach. They have a blind duodenal pouch where the duodenum was transected just proximal to the adherence of the pancreas and the entrance of the common bile and pancreatic ducts. The same pathophysiology might occur in this situation if the biliary limb becomes obstructed. A closed loop obstruction with potential life-threatening complications could occur if not treated timely. In this situation, one must decompress this closed loop, and typically, surgery is undertaken. The authors present a case where nonsurgical intervention with percutaneous decompressive jejunostomy was chosen to treat this problem.
Case Presentation
A 37-year-old female patient who was nine years after conversion of a gastric bypass to a DS for inadequate weight loss and comorbidity resolution had excellent results, losing about 100 pounds in the follow-up period. She was 5 feet 10 inches tall, and her weight had been stable at about 185 pounds. She was doing well until she presented with acute abdominal pain, which required urgent laparotomy and resection of part of her biliary limb for an adhesive obstruction, which caused necrosis of about two feet of small intestine and irrigation of infected fluid, which was throughout her abdomen. She recovered uneventfully and went home five days later tolerating a regular diet, having brown bowel movements, with a vacuum-assisted closure devise on her open granulating wound.
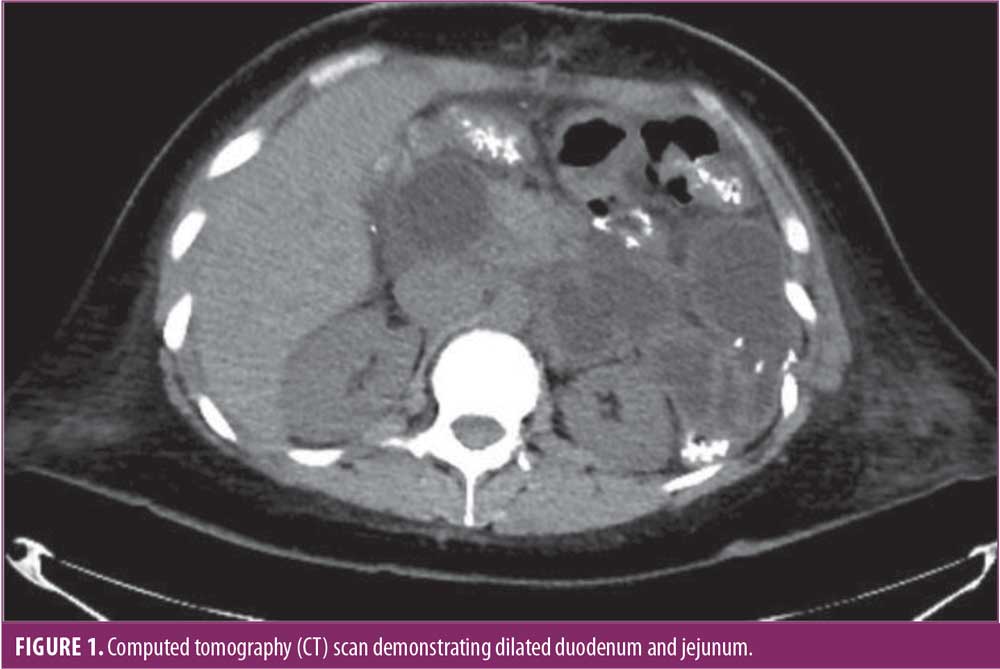
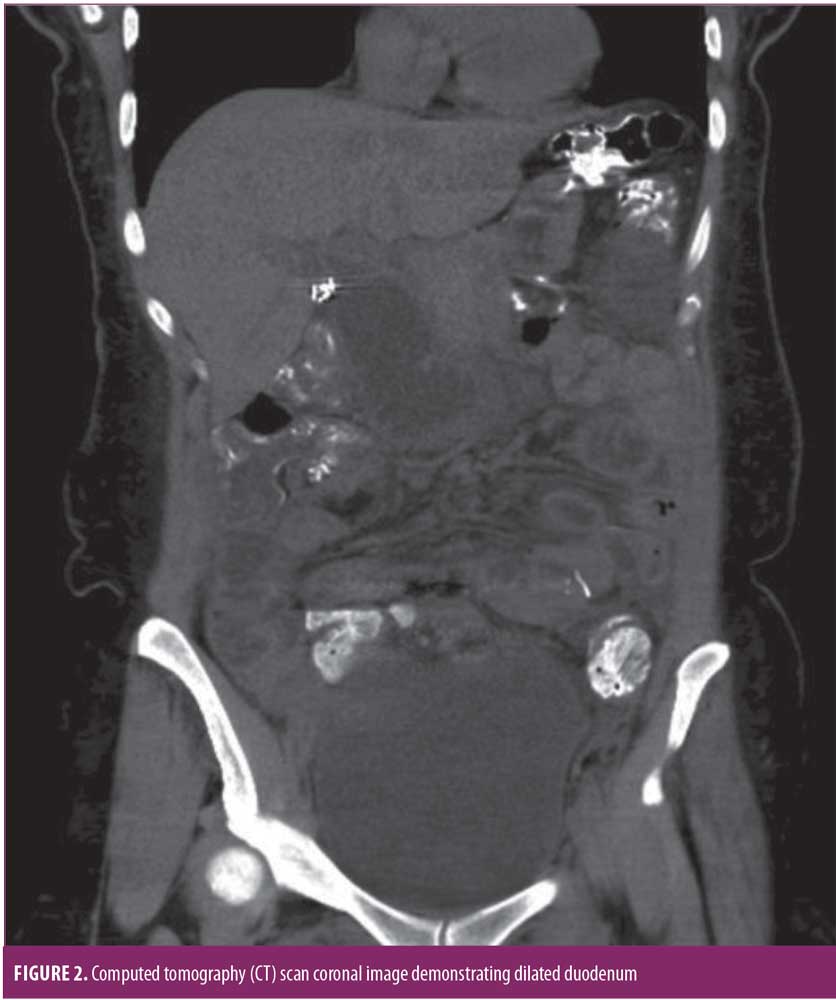
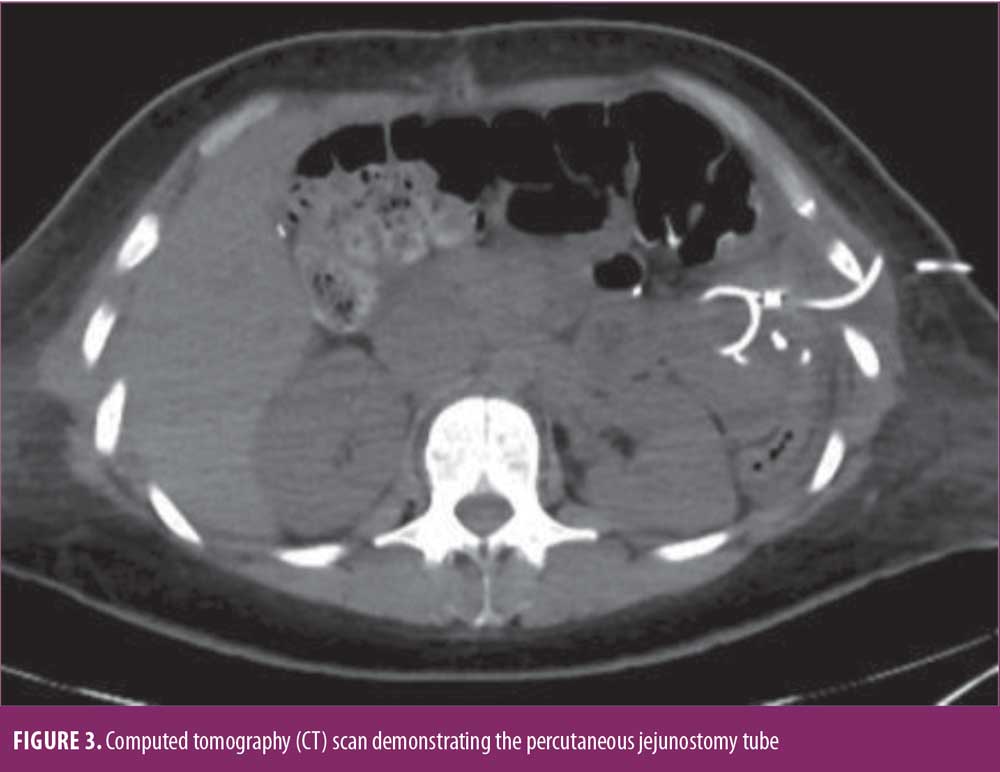
Three days later, she returned to the emergency room with recurrence of her acute abdominal pain. Work-up revealed a very dilated proximal biliary limb with her duodenum and a proximal jejunum measuring over twice its normal diameter. Interesting enough, her liver function tests and lipase were not elevated. Nonetheless her severe pain, along with her abnormal computer tomography (CT) scan findings, allowed us to make the decision to decompress her biliary limb an urgent nature (Figures 1,2). Interventional radiology was consulted, and a percutaneous decompressive jejunostomy was inserted (Figure 3). Her pain resolved, and she was able to tolerate a regular diet. Contrast study through the tube one week later showed the biliary limb to be decompressed and the obstruction resolved (Figure 4). She was discharged with the tube in place, and it was removed three weeks after insertion in the office after she had fully recovered. The patient is doing well in the last 18 months. She did not need any other procedure or surgeries. She was last seen in the office one month prior to submission of the manuscript.

Discussion
An obstructed biliary limb in a patient who has had a gastric bypass presents with a unique circumstance because placing a nasogastric tube will not alleviate this problem. The signs and symptoms of this problem might include severe pain, abdominal distention, tachycardia, hypotension, elevated liver function tests and pancreatic enzymes, and potentially death. Diagnosis is by CT scan or ultrasound. Plain films might commonly miss this diagnosis because the bypassed stomach is usually fluid filled without gas. Percutaneous gastrostomy has become a well-known procedure for patients who present with this problem after gastric bypass.1–4 The benefit of placing this tube is to convert an emergent operation to decompress the acutely distended stomach and correct its cause to an elective operation, if one is needed at all. After the tube is placed, the patient can be resuscitated appropriately, studied through the tube, and then undergo whatever surgery is necessary on an elective basis. Many times, the cause of the gastric dilatation resolves with decompression alone and surgery is averted.
After a DS, acute gastric dilatation does not occur because there is no gastric remnant. Nonetheless, there is still the potential for the blind duodenal loop, which can become obstructed, causing the same set of signs and symptoms and potential mortality if not treated timely. Here, a CT scan is necessary to make the diagnosis. The treatment options are for the most part the same—one needs to decompress the obstructed part of the gastrointestinal tract urgently and then correct the cause. To my knowledge, percutaneous decompressive jejunostomy has not been discussed in this setting, yet percutaneous jejunostomy has been done for a variety of reasons.5,6
In this case, reoperative surgery eight days post laparotomy where adhesions and inflammation could cause a hostile environment might not be the best option. Percutaneous drainage, if possible, would seem prudent. The obstruction here resolved without the need for further surgery, but if necessary, elective surgery could be done in the future.
Conclusion
Duodenal stump blowout from bowel obstruction can be a disastrous complication after DS surgery. Decompressing proximal jejunum percutaneously and providing bowel rest can prevent a major operation in a patient.
References
- Jones K. Biliopancreatic limb obstruction in gastric bypass patient at or proximal to Jejunojejunostomy: a potentially deadly, catastrophic event. Obes Surg. 6;485–493.
- Almulaifi A, Kong-Han Ser, Wei-Jei Lee. Acute gastric remnant dilatation, a rare early complication of lapaorscopic mini-gastric bypass. Asian J Endosc Surg. 2014;7:185–187.
- Bibyan M, Khanolwai RG, Parmar AK, Reddy PK. Percutaneous drainage of gastric remnant dilatation after laparoscopic Roux-en-Y gastric bypass. Asian J Endosc Surg. 2012;5:78–80.
- Petsas T, Kraniotis P, Spyropoulos C. The role of CT-guided percutaneous gastrostomy in patients with clinically severe obesity presenting with complications after bariatric surgery. Surg Laparosc Endosc Percutan Tech. 2010;20(5):299–305.
- Yang ZQ, Shin JH, Song HY, et al. Fluoroscopically guided percutaneous jejunostomy: outcomes in 25 consecutive patients. Clin Rad. 2007;62: 1061–1065
- Sparrow P, David E, Pugash R. Direct percutaneous jejunostomy—an underutilized interventional technique?. Cardiovasc Intervent Radiol. 2008;31:336–341.
Category: Case Report, Past Articles







