Raising the Standard: ASMBS Annual Meeting at ObesityWeek 2018: Getting to the Heart of the Matter
 by Dominick Gadaleta, MD, FACS, FASMBS, and Anthony T. Petrick, MD, FACS, FASMBS
by Dominick Gadaleta, MD, FACS, FASMBS, and Anthony T. Petrick, MD, FACS, FASMBS
Dr. Gadaleta is Associate Chair, Chief of General Surgery, MBS Director, North Shore University Hospital, Northwell Health, Manhasset, New York.
Dr. Petrick is Quality Director, Geisinger Surgical Institute; Director of Bariatric and Foregut Surgery, Geisinger Health System, Danville, Pennsylvania.
Bariatric Times. 2019;16(1):8–9.
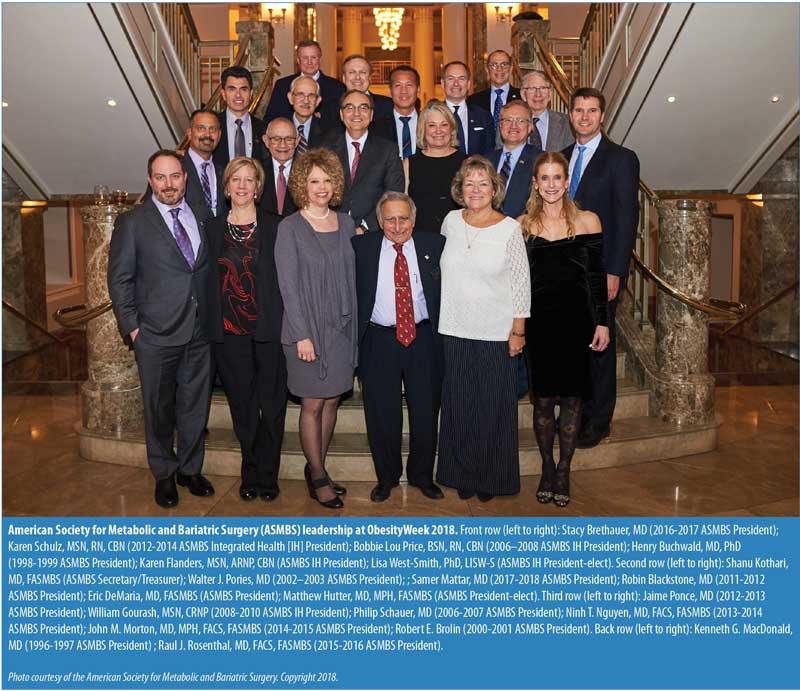
The 35th annual meeting of the American Society for Metabolic and Bariatric Surgery (ASMBS) was held at ObesityWeek 2018 for the first time in Nashville, Tennessee, this year . This unique, international event focuses on the basic science, clinical application, surgical intervention, and prevention of obesity. The ASMBS and The Obesity Society (TOS) again joined resources and presented an outstanding scientific and educational conference covering cutting-edge basic science, clinical research, and public policy impacting the quality of life for the millions who suffer from obesity.
The combined ObesityWeek Keynote Address was given by Steven Nissen, MD, the Chairman of the Department of Cardiovascular Medicine at the Cleveland Clinic and Professor of Medicine at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University. His talk, “The Intersection Between Obesity and Heart Disease,” connected the a meeting which focused on the theme, “Getting to the Heart of the Matter.”
The ASMBS Integrated Health Keynote Address was given by Randy Seeley, PhD, the Henry K. Ransom Endowed Professor of Surgery at the University of Michigan School of Medicine, and the Director of the National Institutes of Health (NIH)-funded Michigan Nutrition Obesity Research Center (MNORC). This address was followed by the ASMBS Integrated Health Presidential Address, which was provided by Karen Flanders, MSN, APRN, CBN. Both speakers and presentations were well-attended and well-received.
This year’s ASMBS Mason Lecture was given by Harvey J. Sugerman, MD, Emeritus Professor of Surgery, Virginia Commonwealth University. Dr. Sugerman described the mental and physical struggles that helped define him as he worked his way through medical school at Thomas Jefferson University, his residency training as a Lieutenant Colonel time in the United States Army, his time as a practitioner in private practice, and ultimately his 28 years at the Medical College of Virginia, which culminated in his becoming the David Hume Professor of Surgery, Chairman of the General and Trauma Surgery Division and Interim Chair of the Department of Surgery. This courageous and heartfelt address will likely have a lasting impact on all who attended.
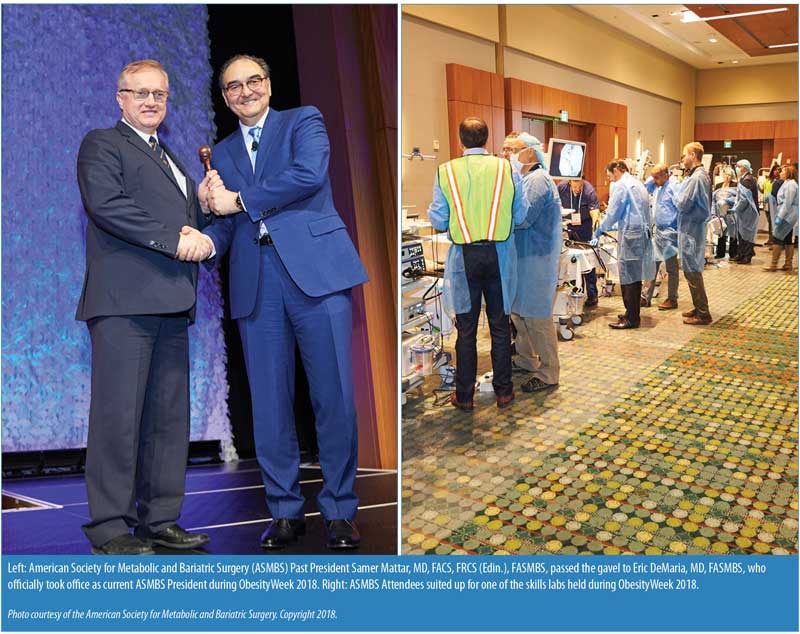
ASMBS Past President Samer Mattar, MD, FACS, FRCS (Edin.), FASMBS, passed the gavel to Eric DeMaria, MD, FASMBS, who officially took office as current President of the ASMBS. Both addressed the audience, highlighting the past year’s accomplishments as well as initiatives for 2019. Next year’s ObesityWeek will focus on the obesity-related comorbidity type 2 diabetes mellitus (T2DM), and Dr. DeMaria shared that he is planning for a term that aligns with that theme.
This year, the ASMBS had 18 preconference courses on Sunday and Monday for all attendees, providing sessions for both novice and seasoned members. These full- and half-day courses were designed to improve skills, help begin a new program or take an existing program to the next level. The course on the high-risk patient, directed by Keith Kim, MD, and Vinni Bajwa, MD, had presentations on the evaluation and safe surgical management of patients with severe and end-stage cardiac, renal, and hepatic disease before and after transplant, as well as patients with severe immune deficiency or hypercoagulable state. The afternoon focused on the surgically complex patient, and presenters provided insight and strategies to manage patients with severe reflux, prior foregut or trauma surgery, and complicated abdominal wall hernias. The enhanced recovery after surgery (ERAS) course, directed by Scott Monte, PharmD, featured presentations by Anthony Petrick, MD; Stacy Brethauer, MD; and Brandon Williams, MD, among others. The half-day course was an excellent review of best practice, and it served as guide to anyone considering incorporating ERAS into their surgical program.
In Top Paper Session I—Heart, moderated by Shanu Kothari, MD; Joel Brockmeyer, MD; Carlos A Schiavon, MD; and more, asked the question: Does the Roux-en-Y gastric bypass (RYGB) common limb length influence hypertension (HTN) remission, weight loss and cardiometabolic parameters? Using data from the Gastric Bypass to Treat Obese Patients with Steady Hypertension (GATEWAY) trial, they analyzed 45 patients who underwent RYGB with 150cm alimentary limb and 100cm biliopancreatic limb. Overall, 51 percent had complete resolution of HTN on no medication; however they found no difference in HTN remission, weight loss, glycemic/A1c, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, and triglyceride levels regardless of length of resultant common limb at one year. During the same session, we also learned that bariatric surgery reduces the incidence of atrial fibrillation1 and decreases the rate of mortality due to congestive heart failure.2
The Top Paper Session II, moderated by Richard Peterson, MD, featured several interesting presentations. Laurent Biertho, MD, from Quebec, Canada, presented their analysis of nonrevisional RYGB and sleeve gastrectomy (SG) from Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) 2015 database. Comparing 123,164 patients under age 65 to 7,501 patients 65 years or older, the researchers found that older patients undergoing bariatric surgery are at higher risk for adverse events, including mortality, regardless of procedure. However, the effect of age on leak rate is only seen in RYGB procedures.3 Dr. Brethauer presented six-month data from a study that evaluated the implementation of new enhanced recovery goals for the MBSAQIP national quality improvement project Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY). Using data from 36 participating centers, 2016 cases prior to implementation were compared to the first six months of ENERGY. Average length of stay (LOS) decreased from 2.24 to 1.76 days (p<0.001), and LOS longer than four days decreased from 8.2 to 4.4 percent (p<0.001) without increased bleeding, reoperation, or readmission rates. There was a significant association between increased adherence to the protocol and decreased odds of estimated LOS (p<0.001). Additionally, participating centers reported that 27 percent of their patients did not require postoperative opioids.4
This article highlights just a small sample of the outstanding posters, videos, and papers presented at the meeting this year. ObesityWeek also offered numerous social and networking opportunities. Congratulations to the Program Committee for organizing an outstanding event and to the ASMBS Foundation for another successful LEAD Awards ceremony. Planning is underway for next year’s annual meeting, which will be held at ObesityWeek 2019 in Las Vegas, Nevada, November 3–7, 2019.
Next month: Decreasing Readmissions through Opportunities Provided (D.R.O.P.), the first national Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) quality improvement project.
References
- Lynch KT, Mehaffey JH, Hawkins RB, et al. Bariatric surgery reduces the incidence of atrial fibrillation: A propensity score matched analysis. Surg Obes Relat Dis. 2018 Nov 24. pii: S1550-7289(18)31132-8. [Epub ahead of print]
- Aleassa EM, Khorgami Z, Tu C, et al. Bariatric surgery decreases mortality of congestive heart failure: A nationwide study. Surg Obes Relat Dis. 2018;14(Suppl 11):S4.
- Biertho L, Nadeau M, Pelletier M, et al. Metabolic surgery versus best medical management for type 2 diabetes: Interim analysis of the REMISSION prospective controlled trial. Surg Obes Relat Dis. 2018;14(Suppl 11):S6.
- Brethauer SA, Petrick A, Grieco A, et al. Employing new enhanced recovery goals for bariatric surgery (ENERGY): A metabolic and bariatric surgery accreditation and quality improvement (MBSAQIP) national quality improvement project. Surg Obes Relat Dis. 2018;14(Suppl 11):S6.
Category: Past Articles, Raising the Standard







