Revisional Bariatric Surgery in Gastric Outlet Obstruction: A Minimalist Approach
 by Fady Kamel, Ekua Yorke, and Christopher de Gara, MB, MS, FRCSC
by Fady Kamel, Ekua Yorke, and Christopher de Gara, MB, MS, FRCSC
Christopher de Gara and Ekua Yorke are with the University of Alberta, Edmonton, Alberta, Canada and the Centre for the Advancement of Minimally Invasive Surgery, Edmonton, Alberta, Canada. Fady Kamel is with the University of Alberta, Edmonton, Alberta, Canada.
Funding: No funding was provided.
Disclosures: The authors report no conflicts of interest relevant to the content of this article.
Abstract: Many operative techniques have been developed to address severe obesity. One such technique, called vertical banded gastroplasty, gained popularity in the 1990s. This approach was eventually abandoned due to failure of sustainable weight loss and delayed complications, such as gastric outlet syndrome. Traditionally, these complications have been managed by converting to a Roux-en-y gastric bypass. However, Roux-en-Y gastric bypass is an involved procedure with its own risks and potential complications. This study presents an alternative approach to gastric outlet obstruction following vertical banded gastroplasty.
A retrospective chart review at the Edmonton Bariatric Surgery Revision Clinic, Edmonton, Alberta, Canada, from November 2014 to July 2016, identified six patients with a previous vertical banded gastroplasty and gastric outlet syndrome. All six patients underwent operative intervention. The mesh band was successfully divided in five of six patients without significant postoperative morbidity. There was complete resolution of symptoms in all patients postoperatively.
This case study describes an alternative approach where division of the mesh in a patient with gastric outlet obstruction secondary to vertical banded gastroplasty can provide complete resolution of symptoms.
Keywords: Vertical banded gastroplasty, gastric outlet syndrome, revisional bariatric surgery, bariatric surgery
Bariatric Times. 2017;14(10):22–24.
Introduction
Bariatric surgery is the only established treatment modality for severe obesity with long-term efficacy in sustainable weight loss1 and resolution of comorbidities, such as diabetes, hypertension, and dislipidemia.2 Historically, many techniques have been developed in hopes of finding a safe, successful, and cost-effective approach. Vertical banded gastroplasty (VBG) was first described in 1982 by Mason and gained popularity in the 1990s due to good weight loss outcomes.3 However, long-term, it became evident that there were significant complications from the VBG procedure, such as gastric outlet obstruction, band erosion, severe reflux, and weight recidivism.[4–6]
The VBG was eventually abandoned due to high rates of weight recidivism (up to 61%) in addition to other complications.[7] Unfortunately, patients who received the procedure frequently seek ongoing medical attention because of these long-term complications. Revision surgery for VBGs is estimated to be as high as 56 percent for complications and failure of sustained weight loss[8] with up to 21 percent occurring within three years of the original operation.[7,9] Other late complications of VBG include gastric outlet obstruction (GOO), with a rate between nine and 12 percent9,10 and gastroesophageal reflux disease (GERD), with a rate of 22 percent.11 Revision surgery for reflux and obstruction often requires conversion to a Roux-en-Y gastric bypass (RYGB) or reversal of VBG, which includes a gastrogastrostomy.
This case study presents an alternate approach to treating patients who have undergone VBG and are suffering from obstructive symptoms.
Methods
A retrospective chart review of all patients who had revision VBG surgery from November 2014 to July 2016 at the Royal Alexandra Hospital in Edmonton, Alberta, Canada, was completed. From August 2015 to July 2016, a total of six patients selected for VBG mesh division were identified. A single surgeon performed all of these revisions.
Prior to conversion, all patients underwent a gastroscopy and upper gastrointestinal contrast study as part of the preoperative workup. A multidisciplinary team also reassessed the patients. The operative approach was similar in all patients. All revision surgeries were started laparoscopically, but converted to open if there were significant intra-abdominal adhesions. Ideally, the whole VBG mesh was removed in its entirety. If this wasn’t feasible, then a significant portion of the mesh was resected anteriorly to relieve the obstruction. In all patients, an intraoperative gastroscopy and methylene blue dye test were used to assess for leak prior to completion of the procedure. The gastroscopy also assessed for anatomic resolution of the gastric outlet obstruction.
Averages tabulated for data were expressed as medians since the dataset was small and deviated significantly from a mean distribution curve. Categorical variables were summarized as number of cases and percentages.
Results
VBG mesh removal was performed on six patients. All patients were female with a median age of 51 years and median body mass index (BMI) of 38.7kg/m2 at the time of the revision procedure. All patients had esophagogastroscopy and stomach and duodenum fluoroscopy prior to operative intervention. The revision procedure was performed a median of 18 years following the initial VBG procedure. These results are summarized in Tables 1 and 2.
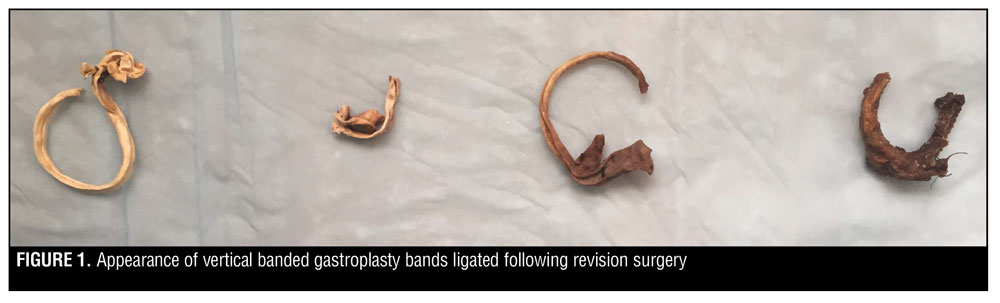
Operative findings. The revision procedure began the same for all patients. Veress needle insufflation followed by laparoscopic trocar placement under direct vision was performed. The patient was then placed in reverse Trendelenburg and the left side elevated. Adhesions were taken down using sharp dissection, electrocautery, and blunt dissection. Table 3 summarizes each patient’s intraoperative findings with regard to the band. Figure 1 shows the appearance of VBG bands ligated following the revision surgery. In all patients, an intraoperative gastroscopy was then performed. It confirmed band release by passing easily into the distal stomach and duodenum. A leak test with insufflation and methylene blue did not identify a perforation in any of the six patients intraoperatively.
Postoperative follow-up. All six patients were followed up for at least 30 days postoperatively. There was resolution of gastric outlet symptoms in all six patients on the first postoperative day. This was maintained at the 30-day follow up for all patients.
Discussion
While VBG is no longer a bariatric procedure offered to patients, it was once popular in the 1990s, and those patients are now presenting with late complications of the procedure. Gastric obstruction is one such complication. When refractory to nonsurgical management, the most common approaches described in the literature are conversion to a RYGB procedure[4,6] or reversal of the VBG, which involves a gastrogastrostomy.[6,12] While both procedures have been shown to resolve symptoms, they do have disadvantages. Conversion to RYGB is a technically challenging procedure, which sometimes has to be converted to an open surgery because of extensive adhesions; it can have complication rates up to 21 percent.[7] These complications include anastomotic leaks, intra-abdominal abscess, port-site infection, intestinal obstruction, and intraluminal hemorrhage.[7,13] A reversal with a gastrogastrostomy creates a connection between the proximal and distal stomach that creates a bypass of the stricture and can lead to significant weight gain postoperatively.[6,12]
Gavert et al5 described an alternative approach where they removed the VBG band and placed an adjustable band in the same procedure. Lim et al recently reported a case series using endoscopic stenting to treat gastric outlet obstruction. However, in their series, four of 13 patients required further operative intervention, and they describe one case where the operative time was 212 minutes. Therefore, this is another involved option with a high complication rate requiring further intervention.3,4 While these procedures are offered to patients, they do come with significant risks, and patients might be hesitant to accept them.5
We present a safe, alternative approach to gastric outlet obstruction and reflux following a VBG procedure. Five of our six patients had at least partial release of the VBG mesh. All patients had complete resolution of outlet obstruction symptoms. This case series demonstrates that simply releasing the mesh can lead to complete resolution of outlet obstruction following VBG. In one patient, the band could not be identified, but she still had complete resolution of symptoms postoperatively suggesting that her symptoms were due to the extensive adhesions intra-abdominally, and not necessarily due to the mesh specifically. Additionally, there was no significant weight gain postoperatively when the patient remained adherent to dietary recommendations. The main benefit of this approach is that it is a less involved procedure than those described previously in the literature and can be accomplished laparoscopically. Additionally, it avoids the described complications that can result from converting to RYGB or reversal with a gastrogastrostomy. Our described approach minimizes operative time and provides the patient with an alternative, safer procedure than previously described options in the literature. The procedure also provides patients with complete clinical resolution of symptoms early in the postoperative period.
Postoperatively, these patients were then enrolled in an intensive program at the Bariatric Revision Clinic to help them remain within an acceptable weight range and continue healthy eating habits. If these patients fail intensive nonsurgical management postoperatively, meaning they were adherent with the multidisciplinary team’s recommendations but still did not achieve sustainable weight loss, then revision surgery to RYGB is still an option.
A limitation of this case series is that it is smal, and although there has only been short-term follow-up, the results are encouraging. It is recommended that all patients with VBG and gastric outlet obstruction have a complete workup, including a thorough history and physical exam, contrast studies, esophagogastroduodenoscopy, and motility studies. After ruling out functional problems, these patients should be considered for a VBG release procedure if they are deemed to be appropriate candidates.
Conclusion
This case series supports an alternative surgical approach to managing gastric outlet obstruction after a VBG. The approach is technically less challenging, relatively quick, and safe. It is a low-risk option for patients with significant comorbidities who would not be candidates for a prolonged surgery, such as RYGB.
References
- Douketis JD, Feightner JW, Attia J, Feldman WF. Periodic health examination update: detection, prevention and treatment of obesity. Can Med Assoc J. 1999;160(4):513–525.
- Sjostrom L. Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS Study. Int J Obesity. 2008;32:S93–S97.
- Mason EE. Vertical banded gastroplasty for obesity. Arch of Surg. 1982;117:701–706.
- Bloomberg RD, Urbach DR. Laparoscopic Roux-en-Y gastric bypass for severe gastroesophageal reflux after vertical banded gastroplasty. Obes Surg. 2002;12:408–411.
- Gavert N, Szold A, Abu-Abeid S. Laparoscopic revisional surgery for life-threatening stenosis following vertical banded gastroplasty, together with placement of an adjustable gastric band. Obes Surg. 2003;13:399–403.
- Tevis S, Garren MJ, Gould JC. Revisional surgery for failed vertical-banded gastroplasty. Obes Surg. 2011;21:1220–1224.
- Brethauer SA, Kothari S, Sudan R, et al. Systematic Review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis. 2014;10(5):952–972.
- van Gemert WG, van Wersch MD, Greve JWM, Soeters PB. Revisional surgery after failed vertical banded gastroplasty: restoration of vertical banded gastroplasty or conversion to gastric bypass. Obes Surg. 1998;8:21–28.
- Marsk R, Jonas E, Gartzios H, et al. High revision rates after laparoscopic vertical banded gastroplasty. Surg Obes Relat Dis. 2009;5:84–98.
- van Dielen FMH, Soeters PB, de Brauw LM, Greve JWM. Laparoscopic adjustable gastric banding versus open vertical banded gastroplasty: a prospective randomized trial. Obes Surg. 2005;15:1292–1298.
- Rebecchi F, Rocchietto S, Giaccone C, et al. Gastroesophageal reflux disease and esophageal motility in morbidly obese patients submitted laparoscopic adjustable silicone gastric banding or laparascopic vertical banded gastroplasty. Surg Endosc. 2011;25(3):795–803.
- Thoreson R, Cullen JJ. Indications and results of reversal of vertical banded gastroplasty. J Gastrointest Surg. 2008;12:2032–2036.
- Suter M, Ralea S, Millo P, Alle JL. Laparoscopic Roux-en-Y after failed vertical banded gastroplasty: a multicenter experience with 203 patients. Obes Surg. 2012;22:1554–1561.
- Lim CH, Amateau SK, Ikramuddin S et al. Endoscopic management of vertical banded gastroplasty stricture: Feasability, safety, and efficacy. Obes Surg. 2016;26:2802–08
Category: Case Study, Past Articles







