Weight Bias Among Healthcare Providers: We have Met the Enemy and it is Us
This activity expired March 1, 2021.
Course Overview
This article reviews up-to-date data related to the issue of weight bias, particularly how it is experienced by individuals and how it might be promulgated by healthcare providers. The abundant literature shows that nearly all types of healthcare professionals evidence weight bias, both implicit and explicit, which impacts patients care, thus presenting a significant barrier to obesity treatment. Tools to help identify bias are discussed along with suggestions to help providers minimize weight bias in words or actions. Finally, the authors provide available resources that measure bias and support efforts to confront weight stigma.
Course Description
This continuing education course is designed to educate, through independent study, integrated healthcare clinicians who care for patients with overweight or obesity, including the metabolic and bariatric surgical patient population.
Course Objectives
Upon completion of this program, the participant should be able to:
- Define weight bias.
- Discuss the prevalence of weight bias in healthcare.
- Discuss how weight bias in healthcare impacts healthcare access.
- Explain the difference between implicit and explicit biases.
- List ways to address biases within clinical practices.
Target Audience: This accredited program is intended for nurses who treat patients with overweight or obesity.
Completion Time: This educational activity is accredited for a total of 1.0 contact hour (Nursing)
Accreditation Summary: This educational program is provided by Matrix Medical Communications. Provider approved by the California Board of Registered Nursing, Provider Number 14887, for 1.0 contact hour.
Provider Contact Information: Emily A. Scullin Matrix Medical Communications, 1595 Paoli Pike, Suite 201, West Chester, PA 19380; Email: [email protected]
Sponsorship and Support: This continuing education activity supported by Medtronic (Minneapolis, Minnesota).
by Paul Davidson, PhD, and Pamela R. Davis, RN, BSN, CBN, MBA
![]() Dr. Davidson is from Brigham and Women’s Hospital Center for Metabolic and Bariatric Surgery, in Boston, Massachusetts, and Harvard Medical School in Boston, Massachusetts. Ms. Davis is with Pam Davis Consulting in San Antonio, Texas.
Dr. Davidson is from Brigham and Women’s Hospital Center for Metabolic and Bariatric Surgery, in Boston, Massachusetts, and Harvard Medical School in Boston, Massachusetts. Ms. Davis is with Pam Davis Consulting in San Antonio, Texas.
Ms. Davis is with Pam Davis Consulting in San Antonio, Texas. She is a Certified Bariatric Nurse and a bariatric surgery patient with 15 years of experience working with individuals affected by obesity. Ms. Davis has authored articles, encyclopedia entries, patient education materials, and practice guidelines for treating individuals affected by obesity.
Funding: This article is part of a continuing education activity supported by Medtronic (Minneapolis, Minnesota).
Disclosures: Dr. Davidson reports no conflicts of interest relevant to the content of this article. Ms. Davis has provided consulting services for Medtronic.
Bariatric Times. 2019;16(3):16–22.
INTEGRATED HEALTH CONTINUING EDUCATION
This department is dedicated to providing peer-reviewed, evidenced-based continuing education activities for multidisciplinary clinicians who care for patients with overweight or obesity and their related comorbidities.
 Department Editor
Department Editor
Tracy Martinez, RN, BSN, CBN
Ms. Martinez is the Department Editor of Integrated Health Continuing Education for Bariatric Times; and Program Director of Wittgrove Bariatric Center in Del Mar, California.
A Message from the Department Editor
Dear Colleagues: I am both pleased yet disappointed to present the latest continuing education module on weight bias and obesity stigma among healthcare providers. I must ask, why are we still struggling with empathy when caring for those with severe obesity?
This article is both educational and provocative because it pushes the reader to look introspectively and honestly to evaluate and reflect on their own potential biases. I thank Pam Davis and Paul Davidson for this wonderful article and also express gratitude to Ted Kyle for his thoughtful and insightful guest editorial message on the topic. Hopefully this will inspire all of us to reflect on our own biases as well as our co-workers’ and clean house where needed.
My best to you,
Tracy Martinez RN, BSN, CBN
Abstract
This article reviews up-to-date data related to the issue of weight bias, particularly how it is experienced by individuals and how it might be promulgated by healthcare providers. The abundant literature shows that nearly all types of healthcare professionals evidence weight bias, both implicit and explicit, which impacts patients care, thus presenting a significant barrier to obesity treatment. Tools to help identify bias are discussed along with suggestions to help providers minimize weight bias in words or actions. Finally, the authors provide available resources that measure bias and support efforts to confront weight stigma.
Introduction
Issues of bias and discrimination are an unfortunate reality, and research shows that stigma based on an individual’s weight is more pernicious than one might expect. Weight bias involves a stereotyped, negative view of an individual with overweight or obesity, in which that person might be subjected to discrimination and unfair treatment in a variety of areas. Though it is illegal to discriminate in employment based on sexual identity or orientation, pregnancy, race, national origin, age, religion, or disability, it is still legal to discriminate because of weight. There are few spheres within life in which some form of bias based on obesity does not exist, including education, media, transportation, clothing purchases, and interpersonal relationships.1,2
A large national sample found that over the past several decades, weight bias was found to be nearly as prevalent as racial or age bias.3,4 A recent evaluation found that weight bias now ranks just below race, gender, and age as the fourth most common form of discrimination in the United States.5 As much as clinicians might be surprised to learn, weight bias also turns out to be common among nearly all types of healthcare providers, including professionals treating overweight and obesity.2,6 In evaluating the literature within this area, there is an opportunity to gain insights as to why this might be and how to make changes to decrease this trend. As clinicians in the field of obesity, it is incumbent upon each of us to take a personal stance to acknowledge and minimize our own biases in providing care and to serve as an example to others.
Weight Bias and Stigma
Weight bias is defined as negative attitudes toward, and beliefs about others because of their weight. These negative attitudes are manifested by stereotypes and/or prejudice towards people with overweight and obesity. Those with obesity can also experience weight bias internalization, which occurs when individuals apply negative weight stereotypes to themselves and self-derogate because of their body weight.7 Weight bias can lead to obesity or weight stigma, which is the social sign or label affixed to an individual who is the victim of prejudice. Obesity stigma involves actions against people with obesity that can cause exclusion and marginalization.8
The notion of weight stigma is something that was described in literature more than a century and a half ago. In “Letters on Corpulence, Addressed to the Public” by William Banting in 1864,9 he said:
“Among the parasites that plague us all, I cannot think of any more distressing than being overweight…It seems to me that being overweight is very little understood by doctors, or they would long ago have found the cure for this sad disease. And yes, the general public is not sympathetic either—or they would stop their sneering remarks and judgmental glances at those of us who are overweight.”9
To many, those words could have been written today and seemed just as accurate.
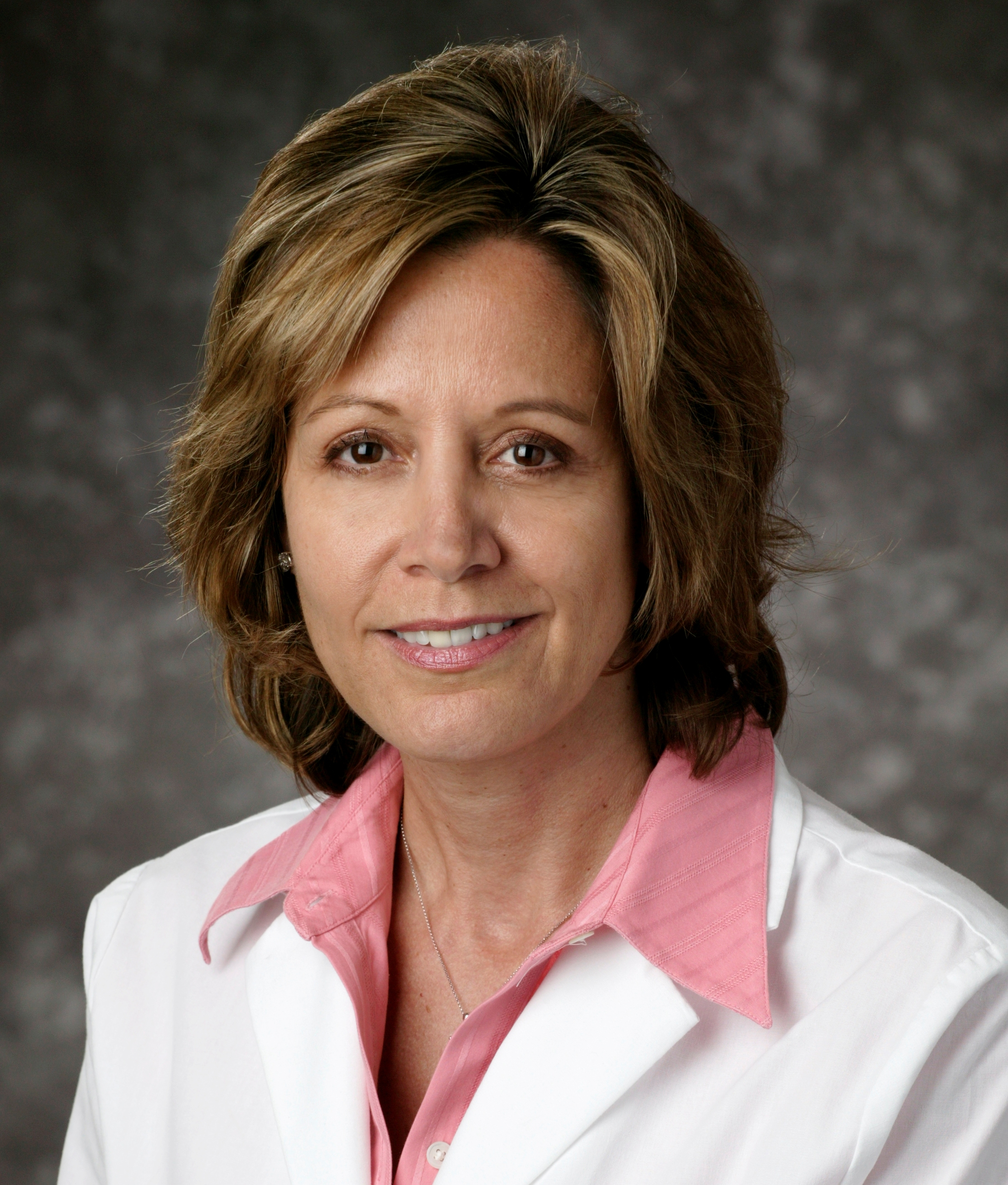
Implicit vs. explicit bias. Forms of bias are categorized as either implicit or explicit. Implicit bias is automatically activated and tends to be more unconscious, influencing individual behavior without clear awareness. The most common way to measure implicit bias is by using an Implicit Association Task (IAT), in which images and words appear on a screen and strength of association is measured by response latency. Project Implicit10 offers different versions of IATs, including “Weight (‘Fat-Thin’ IAT)”. This IAT would conclude the test taker displayed an automatic preference for people without obesity over those with obesity if he or she responded more quickly when “bad” words like “angry” and “horrible” and images of individuals with obesity were assigned to the same response key than the reverse (e.g., bad words and images of people without obesity assigned to same key. Data collected from the Project Implicit Weight IAT reveal a majority automatic preference for “thin” people relative to “fat” people (Figure 1).10
Explicit bias is within conscious awareness and influences outward behavior in an intentional manner. Assessment of explicit bias can be completed using self-report surveys.11
The Presence of Weight Bias and Stigma
Bias toward those who struggle with overweight or obesity might start early in health careers as a study of 206 university health majors demonstrated. In taking an online survey, nearly 93 percent of respondents displayed clear weight bias, particularly as seen through a measure that rated descriptors of those with overweight or obesity. A great majority of students viewed such individuals as “lazy,” “short on will power,” “lacking endurance,” “overeating,” “self-indulgent,” and “weak.”12 An article examining weight bias among exercise students and professionals found that 85 percent of the studies reported obesity stigma among physical therapists, fitness trainers, and those involved in physical education.13 Bias has also been observed among physiotherapists who commonly treat weight-related ailments through hands-on treatments, which include manipulation, massage, exercises, stretching, and electrotherapy. A small but in-depth study of physiotherapy patients found that negative attitudes toward excess weight were notable, graphic images were typically of thin people, furniture was not comfortable for larger individuals, and patients were commonly called out for their weight regardless if it had anything to do with their presenting problems.14
Dietitians and nutritionists have played a seminal role in developing interventions to help individuals with overweight or obesity. In working with issues of nutrition and weight as a core component of training and practice, efforts have been made to determine whether weight bias might exist among clinicians in the nutrition field. One article revealed both implicit and explicit weight stigma toward heavier patients. Factors such as overeating, inactivity, lack of willpower, and unhealthy food choice were considered central to putting on weight, while factors such as genetics, illness, or metabolic issues, were not viewed to be highly relevant.15 Another review showed that a majority of studies involving nutritional professionals evidenced weight bias toward patients with obesity.13
Researchers investigated attitudes of undergraduate dietetics students toward individuals with obesity and tested whether a patient’s body weight influenced students’ treatment decisions and health evaluations. Results revealed that a majority of students felt that patients with obesity were less likely to follow treatment recommendations compared to normal-weight patients. Though both patients of normal weight and patients with higher body mass indices (BMIs) were rated to be as motivated and potentially successful in dietary counseling, the clients with obesity were judged to have poorer dietary habits and overall health though there was no evidence of this in the case studies.16 A recent Brazilian study had nutrition students analyze case scenarios in which patient details, including dietary intake, calories consumed, and life habits, were the same except for whether they were told the patient was normal weight or had obesity. Dietary assessments by the students were more critical of female patients who they believed had obesity even though there was no difference in habits from the normal weight patient vignettes. Male patients believed to have obesity were judged to be less likely to follow dietary recommendations.17
Women with obesity seeking gynecologic cancer screening were interviewed about factors related to their care and how this might discourage them from pursuing treatment. With increased BMI, it became apparent that several issues stood out, including improperly sized equipment, receiving unsolicited advice about weight, being treated negatively, feeling embarrassed about being weighed, and being treated disrespectfully.18
Numerous studies have been conducted with nurses, nurse practitioners (NPs), and nursing students, and among these health providers, there is clear evidence of weight bias. Among nursing students, weight bias was evident on an online IAT measure, especially when the presumed patient was a woman.19 In validating a new instrument to measure attitudes about obesity, NPs were surveyed in a study that showed a clear negative slant. The results of the study showed beliefs about those with obesity were not as positive as those of individuals of normal weight, as they were seen to be less successful, did not make desirable marriage partners, were untidy, and less healthy. The effect was more powerful in judging women rather than men, so a gender bias seemed to be overlaid as well.20 Most recently, a review article by Goad et al explored the association between BMI and self-esteem in nurses, alongside their attitudes toward patients who have obesity. They found the literature to be conflicting with many methodological issues.21 In contrast to the Western findings, a study of 297 nurses in China found slightly positive beliefs about individuals with obesity and a pervasive sense that weight was primarily out of a person’s control.22
There is evidence that therapists who specialize in the treatment of eating disorders also hold onto biased views regarding obesity. While therapists surveyed expressed positive views about treating those with weight issues, they rated their colleagues as saying disparaging remarks about patients with obesity, and many felt that other providers felt negatively or might have been uncomfortable treating those who had obesity. Though these providers felt competent to treat the disease of obesity, they also expressed less hopeful outcomes, doubted levels of motivation among their patients, and felt they were less likely to be compliant with their treatment plan.23 When marriage and family therapy trainees were examined in a study, they were found to express explicit bias, particularly if they had their own weight issues.24
Though the available literature is quite limited, one review article detailed weight bias among pharmacy students and practicing pharmacists. Those individuals make recommendations regarding pharmacologic and nonpharmacologic treatment of illness, and it was determined that both groups demonstrate both implicit and explicit weight bias, however, the practicing pharmacists displayed this to a lesser degree.25
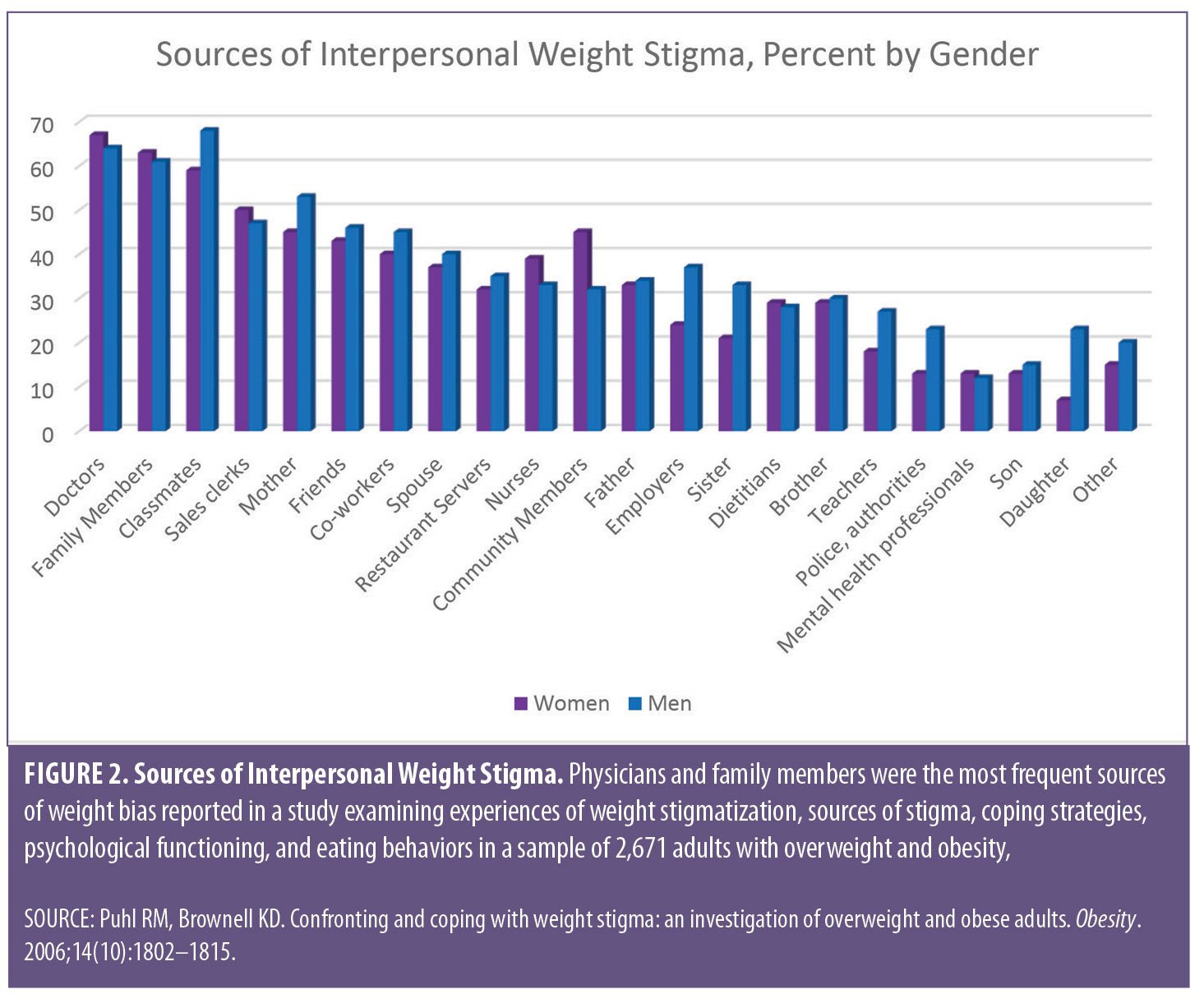 A large study with over 2,500 participants asked men and women to rate whether they had experienced weight stigma from each of 20 categories that included family members, employers, dietitians, nurses, and doctors. Results showed that doctors, family members, and classmates were the most common sources of perceived bias (Figure 2).26 Of note, the experience of bias wasn’t impacted by BMI and was noted at a range of overweight, the only exception being family members who were even more critical as BMI rose.
A large study with over 2,500 participants asked men and women to rate whether they had experienced weight stigma from each of 20 categories that included family members, employers, dietitians, nurses, and doctors. Results showed that doctors, family members, and classmates were the most common sources of perceived bias (Figure 2).26 Of note, the experience of bias wasn’t impacted by BMI and was noted at a range of overweight, the only exception being family members who were even more critical as BMI rose.
Research has demonstrated that physicians are perceived to spend less time with their patients with obesity than patients with normal weight.6 Levels of patient-centered communication have been found to be less with patients deemed to be less likely to follow through, and patients with obesity have been stereotyped in that manner by primary care providers (PCPs). Some studies show evidence that patients with obesity perceive they are respected less by their PCPs, and they receive less time being educated about how to improve their health.27 Studies show that health professionals who harbor weight bias are more likely to believe that weight is caused primarily by behavior rather than biology, feel more negatively about treating those with obesity, and expect outcomes to be less positive than those who don’t hold such biases.23 While strong negative weight bias was seen in an evaluation of healthcare providers, it was noted that those beliefs were still less than what has been noted in the general public.28 In an evaluation of 259 women with obesity who reported generally positive and respectful care by PCPs, there were still elements of bias that crept into the relationship. Most did not feel they could rely on their physician for help with weight loss, and nearly half said that their provider never suggested a means to control weight. A majority also felt the doctors simply did not appreciate how challenging it was to have obesity.29
Though it might seem unexpected, there is strong evidence that even individuals dedicated to treating overweight and obesity commonly exhibit weight bias and stigma. A seminal study conducted in 200130 polled 389 clinicians and researchers who were attending an obesity treatment conference using a self-report questionnaire to assess explicit attitudes and an IAT to measure weight bias. Overall, the obesity health professionals scored in a direction consistent with negative explicit and implicit views of obesity, and they held stereotypes of individuals with the condition as being lazy, stupid, and worthless. On a more hopeful note, the more professionals worked with individuals with obesity, the more positively they viewed such patients.30 A similar study was conducted at the same conference in 2013, and it was observed that over the ensuing time, implicit bias decreased while explicit weight bias increased; the more exposure a provider had to treating patients with weight issues, the less explicit anti-fat bias they endorsed.31 While one might expect that views might be different within the realm of bariatric surgery, surveys and interviews of postoperative patients in one of the only studies of its kind, revealed weight bias. Unfortunately, those who experienced such stigma from providers and who internalized the bias demonstrated a decreased capacity to follow the recommended diet. When queried, their providers attributed their lack of adherence to compliance issues, not recognizing the role they played in the issue.32
Weight Bias as a Barrier to Obesity Treatment
For individuals with obesity, there is an irony in the fact that those who might seek help are often discouraged from doing so because of weight bias among healthcare providers. The longer someone avoids treatment out of fear of the way they are judged, the greater the likelihood of symptoms progressing to medical conditions in which care is both more involved and expensive.30 Research in the field of weight-related bias and stigma makes it clear there are a multitude of negative impacts on patients who are subjected to such treatment. From an emotional standpoint, weight bias has been shown to be correlated with increased rates of depression and anxiety and decreased self-esteem, particularly when that bias has been internalized.26 Many studies have also linked internalized weight bias to poorer body image and dissatisfaction with appearance. Of particular interest in addressing concerns with overweight and obesity, weight bias internalization has been related to increased levels of binge eating, dietary restraint, emotional eating, weight cycling, and more symptoms of food addiction.7 Individuals who have perceived such bias and felt judged negatively by providers have been found to be less likely to attempt or succeed at weight loss.27 Another impact of experiencing weight stigma has proven to be a decreased desire to exercise and be physically active, which further reduces one’s chances of weight loss.
Research also shows that patients with obesity are aware when weight bias occurs in the healthcare setting. Patients with obesity perceive that weight bias leads to less time spent by healthcare professionals and less willingness to perform screening procedures.33 Patients who deal with weight stigma tend to feel a greater sense of shame and then place less value on their healthcare.27 Further, an evaluation of PCPs and their patients found less emotional rapport was built with patients who presented with overweight or obesity. The weakened emotional connection was feared to lead to a diminution of following provider recommendations and decreasing the power of behavioral suggestions.34
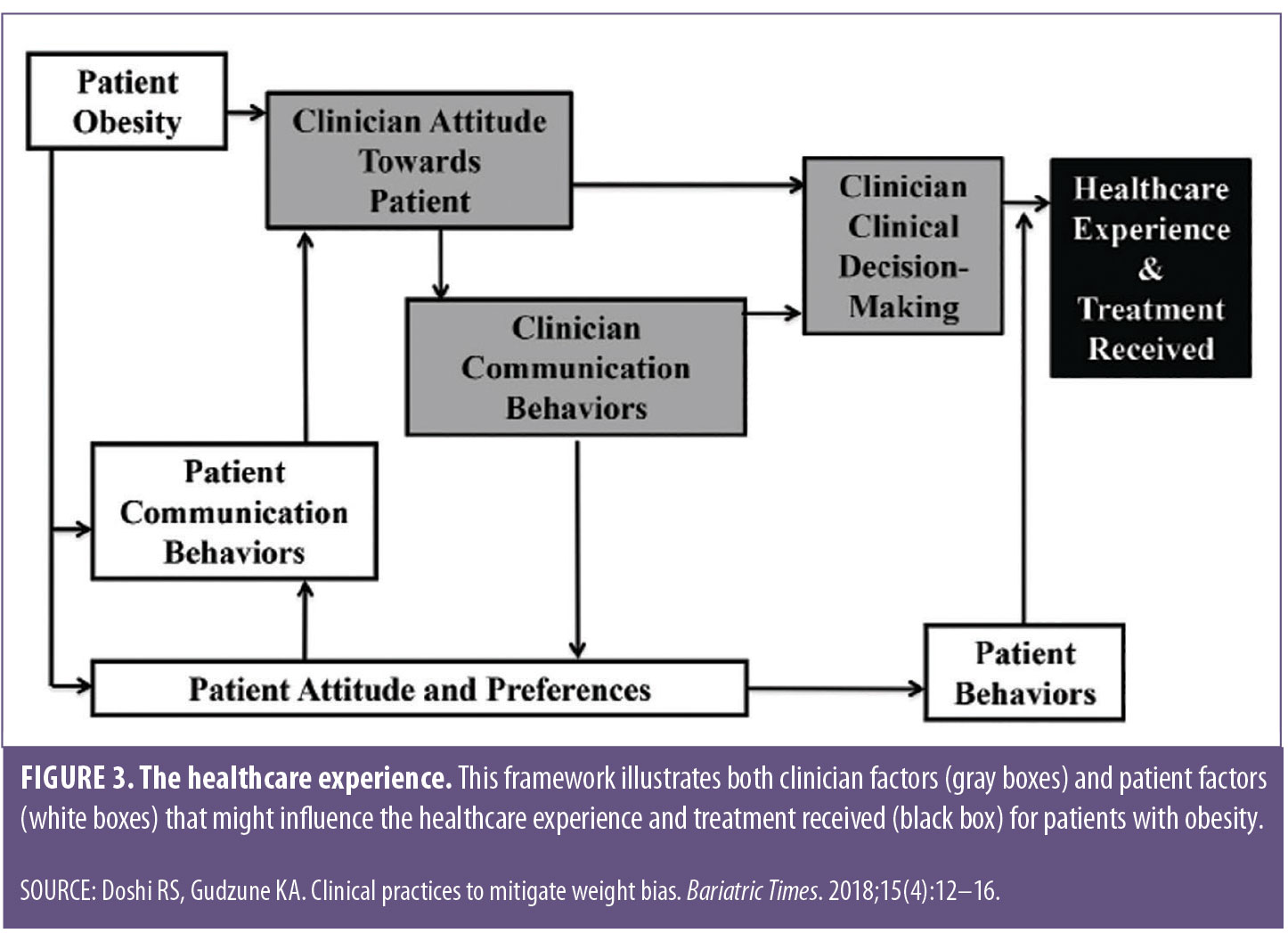 The patient-clinician relationship largely determines the healthcare experience and treatment received. Clinician’s attitude toward a patient, communication, and behavior are all important elements that might be helpful when considering how clinician bias might contribute to lower quality care and healthcare disparities for patients with obesity. (Figure 3).35 Additionally, some clinicians might lack proper education on the disease of obesity and thus feel uncomfortable and unequiped to care for this patient population.36
The patient-clinician relationship largely determines the healthcare experience and treatment received. Clinician’s attitude toward a patient, communication, and behavior are all important elements that might be helpful when considering how clinician bias might contribute to lower quality care and healthcare disparities for patients with obesity. (Figure 3).35 Additionally, some clinicians might lack proper education on the disease of obesity and thus feel uncomfortable and unequiped to care for this patient population.36
In a powerful review article, both patient and treating health professional studies were examined, primarily from community and family care providers, rather than a hospital setting. In every study included, weight was seen to impact the care individuals received in the office. A unifying factor was determined to be a sense of powerlessness on the part of patients experiencing weight bias. With poorer self-esteem, patients tended to shy away from care, and the negative effects worsened with increasing weight. Embarrassment about body image and fear of discussions about weight increased the likelihood of canceling appointments.6
Taken together, evidence of weight bias among nearly all health professional groups makes it clear that this typically undiscussed phenomenon poses a significant barrier to the treatment of overweight and obesity. We can’t point fingers at others, as all areas of healthcare provision have been guilty of this form of discrimination, and it is incumbent upon each of us to recognize that we might be part of the problem. As no discipline is immune, it becomes that much more important to first take a personal inventory of biases and then work toward helping to decrease and eliminate them within ourselves and then our respective fields. This is especially true for those who treat or conduct research about overweight and obesity. In the next section, information will be provided to help with the recognition of bias with suggested interventions to help address the problem.
Recognizing Weight Bias
To better appreciate your own implicit biases, you can take Project Implicit’s IATs, and you can choose to measure implicit weight bias or any number of other variables. Yet, a practice or program is made up of a group of individuals, each with his or her own beliefs and biases. To recognize or identify bias among a group, especially in a setting where based on the specialty, one could assume weight bias would be nonexistent or minimal, it is not uncommon for hospitals, surgeons, and programs to survey their patients regarding their experiences; however, are the appropriate questions included?
Asking the following questions can helping identify one’s own biases:37
- Do I make assumptions based only on weight regarding a person’s character, intelligence, professional success, health status, or lifestyle behaviors?
- Am I comfortable working with people of all shapes and sizes?
- Do I give appropriate feedback to encourage healthful behavior change?
- Am I sensitive to the needs and concerns of individuals with obesity?
- Do I treat the individual or only the condition?
The stigma of obesity is so strong that implicit bias can be evidenced even by those among the most knowledgeable of the disease.30 As is so often the case, we need look no further than our own patients to evaluate the level of sensitivity afforded to their care. One does not have to look far to find multiple anecdotal patient reports of bias among bariatric professionals.
Case Studies
“Sandy” is a 34-year-old woman who presented to an established, high-volume, fully accredited Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) bariatric program for a primary bariatric surgery procedure. After completing all insurance and program requirements, she underwent a laparoscopic Roux-en-Y gastric bypass by a MBSAQIP-verified surgeon in practice for 12 years. Sandy attended her scheduled postoperative visits at one, six, and 12 weeks post-surgery. After her last visit, she contacted the program and said, “I wanted to let you know I won’t be coming back for additional follow up. After spending most of my adult life trying to lose weight, I thought I had found a safe place to go for treatment. The dietitians and nurses made me feel so welcome and inviting, but I’ve left my last two appointments with the surgeon in tears. I didn’t think surgery would be easy, but I also didn’t expect to be yelled at and told I wasn’t losing enough weight. I am doing everything the dietitian has asked; I’m exercising more than I ever have and when he (the surgeon) saw my weight, he told me there was no way I was eating and exercising appropriately, or I would have lost more weight.” After a profuse apology, several options were offered to Sandy, including having a staff member attend her next appointment with her and the option to transfer to another surgeon within the program. The damage however, was done, and she refused both options.
“Alison” is a 43-year-old woman with a BMI of 35kg/m2 and significant comorbidities, including diabetes, hypertension, and reflux. At the first support group she attended after undergoing vertical sleeve gastrectomy surgery, Alison shared that prior to attending the information seminar, she had wondered if surgery was taking the “easy way out,” or if her willpower just wasn’t strong enough; however, based on the information presented, she finally realized she needed formal treatment for her obesity. During her hospital stay, she was questioned by staff in the pre-admission testing area, the surgery check-in area, and the postoperative unit if she was sure she met criteria for surgery and asked, “Why would someone as small as she resort to surgery?” She told the group the questioning from staff in multiple areas reinforced her previous concerns, and she almost left before surgery.
“Jenny” is a 50-year-old woman who started her weight loss journey weighing 542Lbs. She shared a weight bias experience that occurred during her monthly preoperative weight loss program, which was mandated by her insurer. The hospital did not have a scale that went beyond 450Lbs, so the only way her dietitian could get an accurate weight was to take her downstairs to the loading dock and have her step on a freight scale in front of the shipping and receiving staff. Thankfully, this ritual waited until the end of their meeting to minimize the number of people who might witness her walk of shame. She left the appointments in tears each time as she felt the sting of bias and inadequate equipment which left her feeling totally dehumanized. Despite this experience, she persisted and lost 50 percent of her body weight through hard work and bariatric surgery.
These cases only represent three patient scenarios, two of which are from one support group over a three-month period. There are many more examples just like these. This is not acceptable. This is not quality care. We are always leading by example. The examples we provide must be stellar and above board, or we will never gain and maintain patient trust.
Addressing Weight Bias
The presence of and adherence to bariatric-specific guidelines ensure the availability of size-appropriate equipment and furniture and mandate sensitivity training as one of the ongoing competencies for those providing direct care to the patient undergoing bariatric surgery.38 Unfortunately, the guidelines are not able to mandate empathy, understanding, and acceptance of all individuals who present to us for treatment. We must assess and treat our individual bias while establishing the highest of standards for how patients are treated within our programs and facilities. It might be cliché, but it really does begin with you.
The following are suggestions to help mitigate weight bias in the healthcare environment:39
- Avoid stigmatizing or blaming words. Avoid using words that are perceived negatively when talking to patients. Replace negative words such as “obese,” “morbidly obese,” or “fat” with terms like “unhealthy weight” or “high body mass index.”
- Use “patient-first” language. When talking about obesity, use “patient-first” language, such as “patients with obesity” or “patients affected by obesity.” Patient-first language allows the patient to be distinguished from their weight, whereas “obese” encapsulates the patient and his or her weight all in one. People are not their disease, and we must remember that when discussing obesity.
- Be mindful of your approach when discussing weight. The following questions are all constructive ways you can discuss weight with your patients:
- “Could we talk about your weight today?”
- “How do you feel about your weight?”
- “What words would you like us to use when we talk about weight?”
- Implement sensitivity training. If not already offered, annual sensitivity training might be implemented for staff working with bariatric patients, including those outside of the bariatric program. Such training might include an education session on obesity as a multifactorial disease and/or a presentation by a patient volunteer sharing their weight loss experience, good or bad.
- Examine your program’s education and marketing material for appropriate language and imagery. You can view https://www.obesityaction.org/image-gallery/ and http://www.uconnruddcenter.org/image-library for more information.
- Educate. Inform. Be the example. Take every opportunity to use patient-first language and educate colleagues on treating patients with obesity. Discuss obesity as a disease, review the treatment options available, and focus on humanizing individuals affected by obesity during case presentations.
- Speak up. Do not tolerate or accept weight bias in any form.
While media is often seen as a source of weight stigma promotion, the constantly connected nature of our society also presents a unique opportunity for us to inform through various media formats. Research has shown that education, specifically use of video, is effective in reducing stigmatizing attitudes. Two studies investigated the effects of brief (17 minutes) educational films, “Weight Bias in Healthcare” and “ Weight Prejudice: Myths and Facts” developed by the Rudd Center for Food Policy and Obesity, to challenge negative attitudes to obesity. Researchers found that viewing the videos and engaging in a discussion increased beliefs among study participants that obesity is caused by multiple factors (and not simply under personal control). The intervention also decreased negative stereotypes about patients with obesity, confirming that changing attributions of causality and controllability of weight can improve beliefs and stereotypes toward individuals with obesity.40,41
Doshi and Gudzune35 review the effects of different intervention tools used to mitigate weight bias in the healthcare setting, including traditional classroom and web-based educational curricula and experiential learning —witnessing the treatments recommended for patients with obesity, interacting with patients with obesity, and working with senior healthcare professionals who treat patients with obesity. They concluded that programs with a combination of intervention components and multi-faceted content seem most effective in reducing weight bias.35
Conclusion
As outlined above, we are all susceptible to implicit bias as it is formed by our long-standing beliefs. Implicit bias spurs how we immediately react and may reveal itself as our “gut response” to an individual or a setting. It is the unconscious instigator of our conscious reactions directed toward others.
The first step toward changing any behavior is self-awareness followed by a deliberate desire and rationale for change. In this article, we have outlined myriad ways weight bias negatively impacts people with obesity. As healthcare providers, we routinely make the argument with insurers for obesity to be treated as a chronic disease worthy of treatment. It is time we as healthcare providers routinely make the argument for people with obesity to be treated with respect and without bias. We must conquer the enemy within, and it begins with self-awareness, conversation, and education.
References
- Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;19(12):788–805.
- Fruh SM, Nadglowski J, Hall HR, et al. Obesity stigma and bias. J Nurse Pract. 2016;12(7):425–432.
- Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. 2008;16(5):1129–1134.
- Puhl RM, Andreyeva T, Brownell KD. Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int J Obes. 2008;32(6):992–1000.
- Smigelski-Theiss R, Gampong M, Kuraski J. Weight bias and psychosocial implications for acute care of patients with obesity. AACN Adv Crit Care. 2017;28(3):254–262.
- Mold F, Forbes A. Patients’ and professionals’ experiences and perspectives of obesity in health-care settings: a synthesis of current research. Heal Expect. 2013;16(2):119–142.
- Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obes Rev. 2018 Aug;19(8):1141-1163. Epub 2018 May 22
- 8. World Health Organization Regional Office for Europe. Weight bias and obesity stigma: considerations for the WHO European Region. Copenhagen, Denmark; 2017.
- 9. Banting W. Letter on Corpulence, Addressed to the Public. 3rd ed. London: Harrison; 1864.)
- Project Implicit. https://implicit.harvard.edu/implicit/. Accessed February 4, 2019.
- Phelan S, Dovidio J, Puhl R, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity. 2014;22(1):1201–1208.)
- Blanton C, Brooks JK, Mcknight L. Weight bias in university health professions students. J Allied Health. 2016;45(3):212–218.
- Panza, GA, Armstrong L, Taylor B, et al. Weight bias among exercise and nutrition professionals : a systematic review. Obes Res. 2018;19:1492–1503.
- Setchell J, Watson B, Jones L, Gard M. Weight stigma in physiotherapy practice: patient perceptions of interactions with physiotherapists. Man Ther. 2018;20(6):835–841.
- Jung FUCE, Luck-Sikorski C, Wiemers N, Riedel-Heller SG. Dietitians and nutritionists: stigma in the context of obesity. A systematic review. PLoS One. 2015;10(10):1–16.
- Puhl R, Wharton C, Heuer C. Weight bias among dietetics Students: implications for treatment practices. J Am Diet Assoc. 2009;109(3):438–444.
- Obara AA, Vivolo SRGF, Alvarenga MDS. Weight bias in nutritional practice: a study with nutrition students. Cad Saude Publica. 2018;34(8).
- Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes. 2006;30(1):147–155.
- Waller T, Lampman C, Lupfer-johnson G. Assessing bias against overweight individuals among nursing and psychology students: an implicit association test. J Clin Nurs. 2012;21:3504–3512.
- Ward-Smith P, Peterson JA, Associate FC. Development of an instrument to assess nurse practitioner attitudes and beliefs about obesity. J Am Assoc Nurse Pract. 2016;28(3):125–129
- Goad, E, Gleeson K, Jackson S. Personal factors associated with the attitudes of nurses towards patients with obesity: a literature review. Clin Obes. 2018;8(16):444–451.
- Wang Y, Ding Y, Song D, et al. Attitudes toward obese persons and weight locus of control in Chinese nurses. Nurs Res. 2016;65(2):125–131.
- Puhl RM, Latner JD, King KM, Luedicke J. Weight bias among professionals treating eating disorders: attitudes about treatment and perceived patient outcomes. Int J Eat Disord. 2014;47(1):65–75.
- Pratt KJ, Palmer E, Cravens JD. Marriage and family therapy trainees’ reports of explicit weight bias. J Marital Fam Ther. 2016;42(2):288–298.
- Murphy AL, Gardner DM. A scoping review of weight bias by community pharmacists towards people with obesity and mental illness. Can Pharm J. 2016;149(4):226–235.
- Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity. 2006;14(10):1802–1815.
- Phelan SM, Burgess DJ, Yeazel MW, et al. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–326.
- Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? 2001;25(10):1525–1531.
- Wadden TA, Anderson DA, Foster GD, et al. Obese women’s perceptions of their physicians’ weight management attitudes and practices. Arch Fam Med. 2009;9:854– 860.
- Schwartz MB, Chambliss HON, Brownell KD, et al. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11(9):1033–1039.
- Tomiyama AJ, Finch LE, Belsky ACI, et al. Weight bias in 2001 versus 2013: contradictory attitudes among obesity researchers and health professionals. Obesity. 2015;23(1):46–53.
- Raves DM, Brewis A, Trainer S, et al. Bariatric surgery patients’ perceptions of weight-related stigma in healthcare settings impair post-surgery dietary adherence. Front Psychol. 2016;7:1–13.
- Puhl R, Phelan S, Nadglowki J KT. Overcoming Weight Bias in the Management of Patients With Diabetes and Obesity. Clin Diabetes J. 2016;34(1):44-50.
- Gudzune KA, Beach MC, Roter DL, Cooper LA. Physicians build less rapport with obese patients. Obesity. 2013;21(10):2146–2152.
- Doshi RS, Gudzune KA. Clinical practices to mitigate weight bias. Bariatric Times. 2018;15(4):12–16.
- Block JP, DeSalvo KB, Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Prev Med. 2003;36(6):669–75.
- The Obesity Action Coalotion. Weight Bias in Healthcare: A Guide for Healthcare Providers Working with Individuals Affected by Obesity. 2015. https://www.obesityaction.org/action-through-advocacy/weight-bias/weight-bias-guides/. Accessed February 4, 2019.)
- Brethauer S, Clements R, Dallal R, et al. Standards Manual: Resources for Optimal Care of the Metabolic and Bariatric Surgery Patient V2.0 (p. 63). 2016. Retrieved from www.facs.org/mbsaqip. Accessed February 4, 2019.
- Still C. More than a Word—Putting Patients First. Bariatric Times. 2018; 15(2):3.
- Swift JA, Tischler V, Markham S, et al. Are anti-stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized control trial. Obes Facts. 2013;6(1):91-102.)
- Poustchi Y, Saks NS, Piasecki AK, Hahn KA, Ferrante JM. Brief intervention effective in reducing weight bias in medical students. Fam Med. 2013 May;45(5):345-8.).
Category: Past Articles, Review








