A Comparison of Abdominal Computerized Tomography Versus Magnetic Resonance Imaging in the Evaluation of Abdominal Pain after Gastric Bypass
 by Ann M. Rogers, MD, and Jared Cappelli, RN, BS
by Ann M. Rogers, MD, and Jared Cappelli, RN, BS
Ann Rogers, MD, is from The Pennsylvania State University, College of Medicine, Hershey, Pennsylvania. Jared Cappelli, RN, BS, is from Department of Surgery, The Pennsylvania State University, College of Medicine, Hershey, Pennsylvania.
Bariatric Times. 2017;14(7):15–17.
Funding: Funded by the Penn State Association of Family and Friends.
Keywords: magnetic resonance imaging, computerized tomography, gastric bypass, abdominal pain
Abstract: Objective: The authors aimed to determine whether magnetic resonance imaging would be as effective as computerized tomography scan for the evaluation of chronic idiopathic abdominal pain in postoperative gastric bypass patients.
Design: Patients seen in clinic with complaints of chronic, recurrent central abdominal pain with no identifiable cause were scanned with conventional computerized tomography scan with oral contrast, followed by magnetic resonance imaging with an abdominal protocol, on the same day. Each computerized tomography scan was interpreted by a dedicated body-imaging radiologist. Each magnetic resonance imaging was separately evaluated by a different body-imaging radiologist, blinded to the identity of the gastric bypass patient or the results of the computerized tomography scan.
Setting: Outpatient surgical weight loss clinic at the Penn State Hershey Medical Center, Hershey, Pennsylvania. Participants: Eight Roux-en-Y gastric bypass patients, all women aged 32 to 59 years, at a mean of five years after surgery.
Measurements: Measurements in this study were radiology reports created by body-imaging radiologist for both computerized tomography scan and magnetic resonance imaging results.
Results: All gastric bypass patients were shown to have normal post-gastric bypass anatomy by computerized tomography scan and magnetic resonance imaging. Six patients had additional computerized tomography scan findings necessitating additional interventions, none of which revealed any significant findings nor led to further treatment. Four patients had additional magnetic resonance imaging findings; none required further evaluation except for one finding of pancreatic cysts for which an interval magnetic resonance imaging was recommended.
Conclusions: Both computerized tomography scan and magnetic resonance imaging may be equally useful studies for the elective evaluation of nonspecific abdominal pain after gastric bypass. Magnetic resonance imaging confers no ionizing radiation, so may be the preferred modality.
Background
Gastric bypass patients are frequently subjected to ionizing radiation (IR), sometimes during upper gastrointestinal (UGI) swallow studies but more often during computerized tomography (CT) to evaluate internal anatomy, generally in the setting of postoperative abdominal pain. About 30 percent of gastric bypass patients present emergently in the postoperative period, over half present for central abdominal pain.[1] The current gold standard study to evaluate such symptoms in gastric bypass patients is CT of the abdomen and pelvis. Such studies, depending on whether they are performed with or without contrast material, may subject patients to a range of 8 to 15 millisieverts (mSv) of IR.
The average adult living in the United States receives an estimated 3 mSv per year in background radiation, and another 3 mSv per year from medical procedures.[2] The Biological Effects of Ionizing Radiation (BEIR) VII model for lifetime risk of developing cancer from low-level IR estimates that 1 out of 1,000 people exposed to 10 mSv of IR will develop cancer in their lifetime.[3] Based on a prior study,[4] we determined that in a cohort of laparoscopic gastric bypass patients, some individuals underwent as many as 25 abdominal CT scans in the first five years postoperatively. This suggests that some gastric bypass patients may be at significantly higher than average risk for the development of future cancers.[5] On the other hand, magnetic resonance imaging (MRI) uses radio waves, non-ionizing electromagnetic radiation.
Despite the different techniques, there is often significant overlap between the readings of CT and MRI diagnostic images. We were interested in comparing such imaging in known patients, and to this end, applied for and received grant funding for a pilot study. In this pilot study we aimed to determine whether concurrent CT and MRI for gastric bypass patients presenting with abdominal pain would be sufficiently similar to allow a recommendation that the preferred standard be MRI.
Methods
After Institutional Review Board (IRB) approval, and receipt of a small grant to cover the costs of MRI scanning, enrollment was opened for all laparoscopic gastric bypass patients of a single surgeon at a university hospital tertiary care center. Gastric bypass patients were seen in our clinic for chronic, recurrent central abdominal pain with no clearly identifiable cause (e.g., absent gallbladder or no biliary symptoms to indicate biliary ultrasound or functional scanning). Patients were first electively scanned with conventional CT with oral contrast only, paid for by insurance coverage, followed by abdominal protocol MRI on the same day. According to our protocol plan, if there was a finding on either study mandating urgent operation, intraoperative findings would be correlated with imaging readings. A total of eight gastric bypass patients were enrolled and scanned. Each CT was interpreted by a dedicated body-imaging radiologist (BIR). MRIs were separately evaluated by another BIR, blinded to the identity of the patient or the CT results. Both readings were reviewed by the research team to determine if there were significant diagnostic differences between modalities.
Results
All study patients were women with a mean age of 46, and a mean postoperative body mass index (BMI) of 32.2kg/m2 (range 20.9–50.7kg/m2). All had undergone laparoscopic Roux-en-Y gastric bypass by the same surgeon with an identical technique (antecolic, antegastric, total linear stapled anastomoses, alimentary limb length between 100 and 150cm depending on BMI, with suture closure of all internal hernia defects). The mean time after bypass was 60.9 months (range: 26.2–101). Results of the CT and MRI scans of the eight patients are collated in Table 1. The mean IR dose conferred per CT was 11.19 mSv, amounting to about twice the IR an average United States adult receives as part of life on the planet. All patients were shown to have normal post-gastric bypass anatomy by CT as well as MRI, thus excluding the more commonly expected findings, such as leaks, evidence of internal hernia, lengthened blind limbs, intussusception, and fistula, in all patients.[6] Based on this, no patients underwent operative procedures. Six patients had additional CT findings that led to the need for multiple additional interventions, including colonoscopies, upper endoscopies, specialist consultations, and interval CT scans, neither of which revealed any significant findings nor led to further therapeutic treatment. Four patients had additional MRI findings; none required further evaluation except for one finding of pancreatic cysts for which an interval MRI was recommended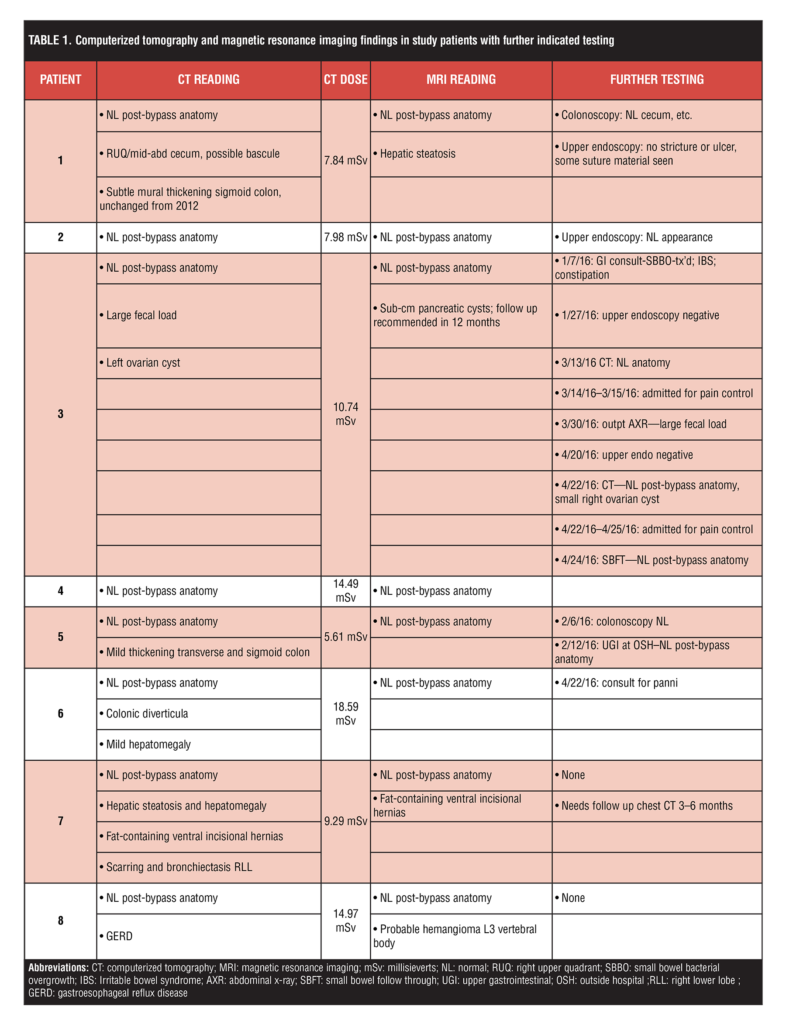
Conclusion
CT is currently the gold standard study for emergent evaluation of gastric bypass patients with abdominal pain because of its ready availability at all hours, no contraindication for patients with metallic implants or shards, and no significant issue with claustrophobia because of the more open environment. However, both CT and MRI may be equally useful studies for the elective evaluation of nonspecific abdominal pain after gastric bypass. Insurance coverage for CT scans is almost universal, while precertification for MRI studies generally requires another level of approval. In our pilot study, the evaluation of post-bypass anatomy was identical between the two modalities. Additional incidental findings were more common after CT, and mandated additional work-up, some of which entailed even more IR, but further evaluation never led to significant findings. While the cost of MRI is somewhat higher than the cost of CT, the additional medical investigations necessitated by the CTs made the CT-related cost of care overall much higher. We suggest that MRI may be a superior modality for the elective work-up of gastric bypass patients with undifferentiated central abdominal pain, not only because of the lack of IR, thus conferring no additional cancer risk, but also because it may be equivalently diagnostic and overall more cost effective. We hope to pursue funding for a larger study to look for significant differences or similarities between the two modalities.
References
- Cho M, Kaidar-Person O, Szomstein S, Rosenthal RJ. Emergency room visits after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Obes Relat Dis. 2008;4:104–109.
- Mettler FA, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog 1. Radiology. 2008;248:254–263.
- Semelka RC, Armao DM, Elias J, Huda W. Imaging strategies to reduce the risk of radiation in CT studies, including selective substitution with MRI. J Magn Reson. 2007;25:900–909.
- Rogers AM, Dudeck B, Winder J. Evidence for and potential causes of high postoperative radiation exposure in gastric bypass patients. Surg Obes Relat Dis. 2015;11:s86–87.
- Sodickson A, Baeyens PF, Andriole KP, et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults 1. Radiology. 2009;251:175–184.
- Greenstein AJ, O’rourke RW. Abdominal pain after gastric bypass: suspects and solutions. Am J Surg. 2011;201:819–827.
Category: Original Research, Past Articles




