Women in Surgery: Interview with Saniea F. Majid, MD, FACS, FASMBS
 Featuring Saniea F. Majid, MD, FACS, FASMBS
Featuring Saniea F. Majid, MD, FACS, FASMBS
Founder and President of the Weight Loss and Wellness Center in Livingston, New Jersey; Diplomate of American Board of Obesity Medicine (ABOM); and Vice President of the New Jersey Chapter of American Society for Metabolic and Bariatric Surgery (ASMBS).
The Bariatric Times editors interviewed prominent New Jersey bariatric surgeon Saniea Majid, MD, FACS, FASMBS, about her original research based on a survey of a small group of members of the American Society for Metabolic and Bariatric Surgery (ASMBS). She provides context for what she found and how it relates to weight regain (WR) and inadequate weight loss (IWL).
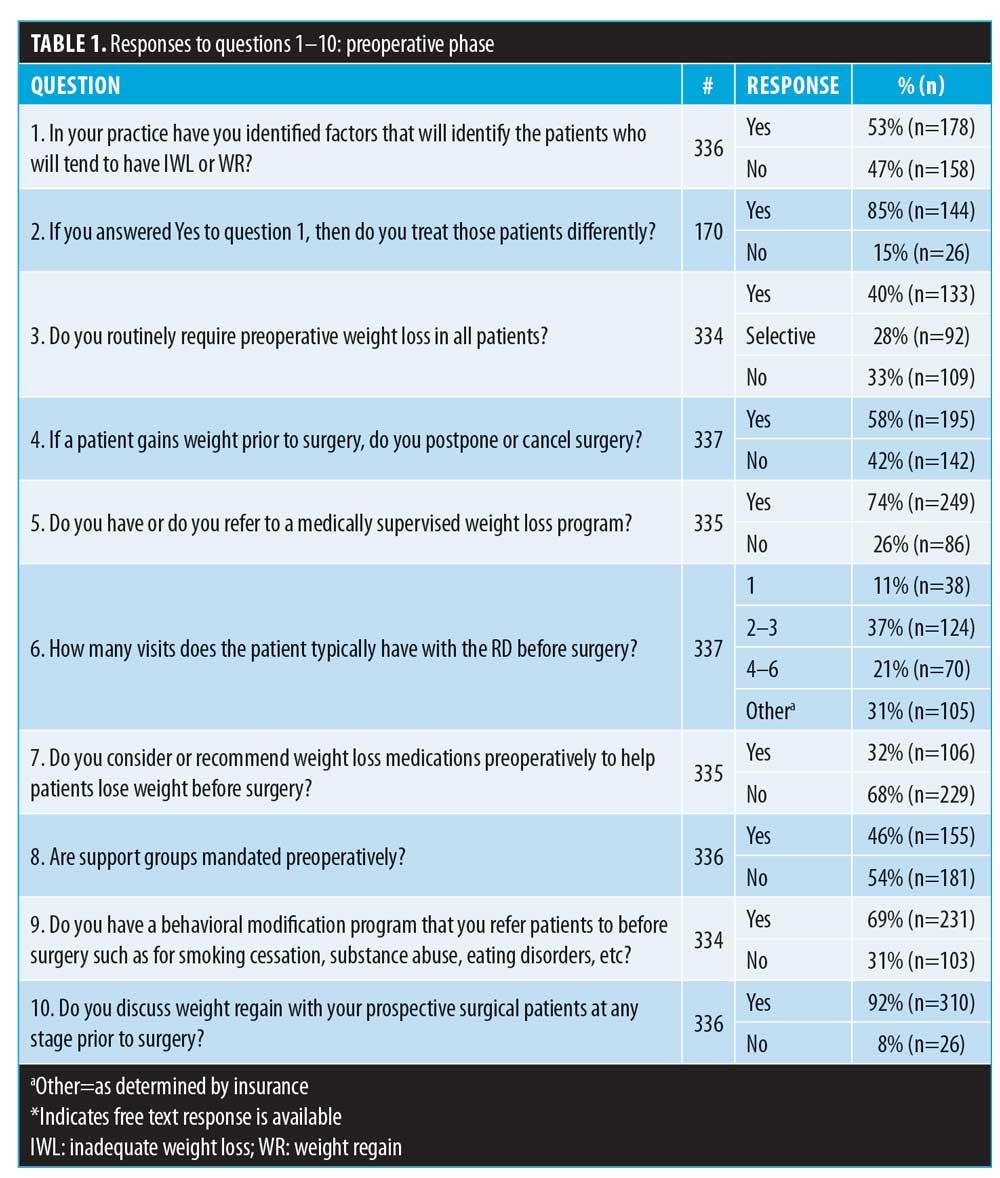
The ASMBS completed a survey of its members on a variety of topics related to weight regain (WR) and inadequate weight loss (IWL). What are the key takeaways from the survey?
Dr. Majid: The key takeaway is that there is a lot of variation in the way weight recurrence and inadequate weight loss are being addressed by programs all over the country. This is an area that requires additional research and understanding in order to develop best practices that can be easily adapted all over the country, by all practices—large or small, community-based or academic.
Based on the responses, there seemed to be a discrepancy in how facilities handle issues such as weight gain prior to surgery and whether or not preoperative weight loss is required. What do you think are the reasons for this?
Dr. Majid: There are several reasons for this variation in practice. Insurance coverage is a big one. Preoperative weight loss has been used by insurance companies as a reason to deny patients access to bariatric surgery. The ASMBS has issued a statement discrediting the requirement of preoperative weight loss for insurance approval. Where this is not being followed, programs and practices have to still comply with the insurance companies’ policies. Some programs might still look at the preoperative weight loss as a gauge to patient commitment and compliance. Others look at it as a barrier to getting patient access to care.
The majority of respondents said they do not recommend weight loss medications prior to surgery. Why do you think this is the case? Do you think the field as a whole is trending toward more acceptance of medical weight loss drugs in conjunction with surgery?
Dr. Majid: The use of weight loss medications is still in its infancy. We are still not completely embracing the concept of obesity being a chronic disease that might require a multimodal treatment approach. However, the field as a whole is trending toward accepting the weight loss medications, especially in the last few years with more United States Food and Drug Administration (FDA)-approved weight loss medications being available. The use of these medications as a “neoadjuvant” versus an “adjuvant” therapy, like in the field of oncology, is yet to be fully determined.
The results were split almost evenly regarding the use of an exercise physiologist/personal trainer postoperatively. Do you think this is more a product of the size of the facility/access to these professionals, or is it more of a philosophy of the facilities?
Dr. Majid: We think it is most likely a combination of lack of resources—usually personal trainers and exercise physiologists are at an additional cost to the patient and the program. These modalities are only effective when used consistently over an extended period of time and the cost adds up. Also important to accept is that there are still programs that might consider this to be not an important aspect of the care of a patient with obesity. On the same token, there are patients who will not feel that the cost of an exercise physiologist to be justified. This presents an opportunity to educate all parties.
Were there any results to questions that surprised you? If so, which ones and how?
Dr. Majid: Bariatric surgery is a powerful tool. It is the only tool proven to help patients struggling with the disease of obesity. For decades, people have tried to find a “magic diet” or a “magic pill.” We have this great tool that has helped a lot of patients. The wide variability in the way this powerful tool is being adopted is surprising. Variability is across some significant areas, such as support groups and RD visits.This can potentially impact the outcomes from bariatric and metabolic surgery, without realizing that it is, especially from the patient’s standpoint.
Based on the variety of responses in the survey as a whole, do you think developing a nationwide set of guidelines for handling patients pre- and postoperatively are necessary, or is this too difficult to enforce?
Dr. Majid: Age-adjusted prevalence of obesity in adults in the United States is 42.4 percent based on 2017–18 Centers for Disease Control and Prevention (CDC) data. With the current COVID-19 pandemic, these numbers are mostly likely only going to go up. We are talking about the epidemic of obesity. Since this disease affects so many, a nationwide set of guidelines is very important. This will also improve our ability to measure the outcomes both in the short and long term and to come up with better treatment algorithms. The more clear and simple the guidelines are, the easier it would be to enforce. But it needs to be done to get this epidemic under control.
This interview has been edited for length and clarity.
Category: Interviews, Past Articles




