Access to Bariatric Surgery—Knocking Down Barriers ONE DAY AT A TIME!
 by Adrian Dan, MD, FACS, FASMBS
by Adrian Dan, MD, FACS, FASMBS
Dr. Dan is Medical Director, Weight Management Institute at Summa Health in Akron, Ohio, and Associate Professor of Surgery at Northeastern Ohio Medical University (NEOMED) in Rootstown, Ohio.
Funding: No funding was provided.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Bariatric Times 2021;18(7):10–11
It’s a Friday afternoon and winter’s grasp on Northeast Ohio is starting to loosen. As I make my attempt to escape early for the weekend, my phone rings. It’s one of our cardiologists asking to discuss a potential bariatric referral. The patient is a 52-year-old male individual with morbid obesity, diabetes, hypertension, and obstructive sleep apnea who will need a major open-heart surgical intervention. But to be a candidate, he would need to lose a substantial amount of weight and control his many comorbid conditions. It was quickly agreed by all that the best path forward was to first proceed with a sleeve gastrectomy. DONE DEAL…
…NOT SO FAST. We offered an appointment within days and the plan seemed clear. A sleeve gastrectomy would be his ticket for another life-saving procedure. Without a doubt, this was an opportunity to save a life. The stars aligned for all of the specialists to come together and render this patient some of the best therapies that modern medicine has to offer. But the exuberance was short lived. While the clinical plan was solidified, the patient’s insurance plan excluded benefits for metabolic and bariatric surgery…WAIT, WHAT? The best first step in this patient’s treatment plan, agreed upon by the entire multidisciplinary team, is not covered by the insurance plan? How can this be? While I attempt to inject a bit of drama into the story, I’m reminded that this scenario is unfortunately all too common for anyone working in our specialty. But how did we get to the point where the one therapy that might optimize him as a suitable candidate for another lifesaving procedure is off the table?
The most obvious culprits to blame are the insurance carriers, most of which do not include metabolic surgery as a basic universal benefit in all of their plans. The issue is much more complex, however, as employers often demand tailored plans to control costs. Also, consider the business models of the third party payers and the limited funds of government plans. Despite the numerous studies that have shown that surgery reduces the overall cost of medical care to the system, the purse string holders often focus on the immediate bottom line and the potential savings accrued by excluding bariatric surgery (and other services). To be fair, many insurers have accepted the advantages of surgery for obesity and, to their credit, have made efforts to eliminate barriers. But despite the enormous amount of evidence, others have found creative ways to limit the access to surgery for the multitude of patients who need it.
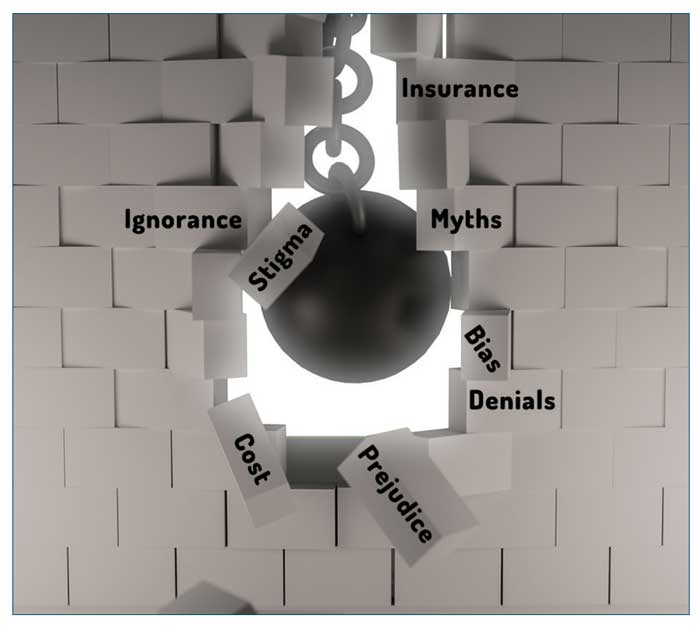
There is also the fierce prejudice that hangs over patients with obesity and those who seek treatment for what some erroneously consider to be a self-inflicted condition. This persists due to the lack of education about obesity and bariatric surgery among many medical professionals, including some surgeons. The pathophysiology of this disease and the true mechanisms by which metabolic surgery work are just now coming to light, and our educational efforts to catch up in medical schools and residencies are still sorely lagging.
The public perception of metabolic surgery still remains problematic. Surgical procedures, in general, are thought of as last resort radical efforts to remove or repair diseased organs. It is difficult for the lay public to understand how operating on a functional gastrointestinal (GI) tract can impact their metabolism (a conceptual network rather than an actual organ). It is understandable that patients first want to exhaust any nonsurgical options rather than surgery on what is falsely perceived to be a healthy GI tract. It falls on us to provide outreach and public education about the real underpinnings of obesity as well as the curative and preventative benefits of surgery.
My patient is just one out of millions across the world who find themselves in such a quandary. A safe and effective remedy for their disease exists but is unavailable to them. The problem is not access but rather the many obstacles that exist. Patient advocacy to address these barriers should be embraced by the surgical community and accepted as a responsibility that comes with the privilege of being a surgeon. Whether serving on a society committee or working to educate our colleagues and public locally, there is no shortage of opportunity for surgeons to make a difference. Leading the charge on this initiative in the American Society for Metabolic and Bariatric Surgery (ASMBS) for the better part of a decade, Dr. Joe Northup has gained a unique perspective from the proverbial trenches that exist in the battle for access to metabolic and bariatric surgery. For those who wish to join the cause, here is how you can get involved!
Guest Perspective
by C. Joe Northup, MD, FACS, FASMBS
Chair, American Society for Metabolic and Bariatric Surgery (ASMBS) Access to Care Committee ASMBS Executive Council.
Gender. Race. Ethnicity. Sexual orientation. Age. Weight. Unfortunately, a commonality among all these factors is discrimination. For patients living with obesity, access to care remains a moving target and a manifestation of this cruel reality. Obesity discrimination continues to be an overlooked prejudice that also has biases and shame that prevent its victims from speaking out. No other proven medical specialty has such incessant struggles with coverage. We are repeatedly obligated to prove our cost-effectiveness and safety. Even when patients have coverage, preoperative medical weight loss prerequisites, excessive requirements, and disproportionate copays delay lifesaving therapy.
There have been some tangible triumphs in the past few years. We have been able to persuade several national insurance plans to eliminate a six-month diet requirement for a significant number of patients. While not ubiquitous across these companies, this has been a step in the right direction for access. The ASMBS leadership and members of its Access to Care committee should be commended for their relentless dedication and tireless efforts to achieve this progress. The Obesity Action Coalition (OAC) is also a tremendous resource for patient advocacy. I encourage every program to promote membership in the OAC to their patients. The more people who become involved, the louder our collective voice will become.
Currently, a notable number of patients still do not have adequate or reasonable bariatric surgery coverage. Our efforts must begin at home. It remains shocking that many hospitals, health systems, and universities that provide bariatric services still do not provide coverage for their own employees. For Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) site surveyors, the employee coverage status is one of the first signs of an institution’s true commitment. While this certainly is not an accreditation standard, it is an important topic to discuss when reviewing a program. Some large institutions will not provide coverage or might have a dollar cap limit. Many institutions’ insurance policies require higher copays for bariatric surgery compared to other essential surgical procedures. This should be considered unacceptable and a primary action item if you practice in such an organization.
The most important thing to remember is that surgeons do have a voice. With determination and perseverance, an individual surgeon can make a significant difference. As we look at the access-to-care victories we have had to date, it almost always starts with one single person. Even more powerful than our own voices are those of our patients. If you have the opportunity to meet with an insurance medical director, an administrator, or a politician, consider having one of your patients accompany you. We have all been moved by stories of patients who overcame obstacles to positively impact their health. When patients also describe the psychosocial and economic impact that surgery has had on their life, the narratives will stand out even further in the minds of the decision makers.
If we want to make changes, it will take all of us working together to advocate for our patients. I will take this opportunity to challenge every bariatric surgeon. Make advocacy your priority.
ONE DAY… take just one day from your practice each year. Do not see patients, operate, or even make rounds that day. Make it your own advocacy day. Meet with your local, state and national politicians. Meet with your state insurance commissioner or the regional medical director of your largest commercial plan. Meet with some of the primary care providers and even your surgical colleagues. Schedule one meeting or as many as you can. Encourage your patients to get involved and come along. Engage employees who lack bariatric coverage and help them become advocates for themselves. Make their employers aware of the discrimination to which they are (probably unknowingly) contributing. Make calls to key stakeholders. The only way we can continue to improve access is to individually take action one such day at a time.
We have come a long way over the past several years in improving coverage and access. While our future remains optimistic, many challenges still remain. Insurance companies continue to use our own MBSAQIP data to block center accreditation, thus limiting the number of programs providing access. The impacts of bundled care payments and the effort to force our practice to outpatient/same day surgery are yet to be realized. These topics could have significant bearing on our practices and our patients’ access to care in the immediate future. Although we still have a long way to go, we have made progress, and I remain hopeful that one day we will be able to achieve the goal of providing a metabolic and bariatric procedure to any patient who needs it. Remember… ONE DAY!
Category: Past Articles, Perspectives



