Analyzing the Efficacy of Laparoscopic Sleeve Gastrectomy and Laparoscopic Roux-en-Y Gastric Bypass Using BODY-Q

by Rushay Amarath-Madav, MD; Tyler Beauchamp, BS; Aditya Devarakonda, MD; Brianna Stadsvold, MD; Aaron Bolduc, MD; Lisa Renee Hilton, MD, FACS, FASMBS
All authors are with Medical College of Georgia in Augusta, Georgia.
Bariatric Times. 2023;20(9–10). Published online September 25, 2023.
Funding: No funding was provided for this article.
Disclosures: The authors have no conflicts of interest relevant to the contents of this article.
Correspondence: Lisa Renee Hilton, MD, FACS, FASMBS; Email: [email protected]
Abstract
Introduction: This study aimed to compare patient-reported outcomes (PROs) between laparoscopic sleeve gastrectomy (LSG) and laparoscopic Roux-en-Y gastric bypass (RYGB), chiefly focusing on body image, physical function, physical symptoms, and body satisfaction. The rising popularity of bariatric surgery has prompted the development of the validated PROs measurement tool, BODY-Q. Using BODY-Q, researchers have been able to draw distinctions between outcomes related to patient eating behaviors following bariatric procedures, such as LSG and RYGB. This study implements the BODY-Q to survey LSG and RYGB patients, with a focus on patient-reported psychological and physiological outcomes postintervention.
Methods: Surveying was performed from April to September 2021, utilizing the BODY-Q PROs measure (PROM). The independent scales utilized in this study were body image, physical function, physical symptoms, and satisfaction with body. All patient submissions were deidentified and securely stored using the QualtricsXM server. Bariatric patients were contacted via email with web links and information on how to complete the BODY-Q survey. Of the 102 RYGB patients contacted, 29 completed surveys. Of the 233 LSG patients contacted, 70 completed surveys. Averaged scores from individual questions and independent scale raw sums were compared using Mann-Whitney U tests.
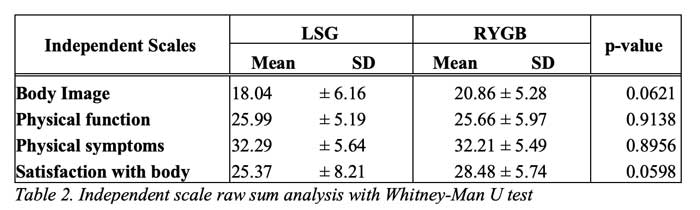
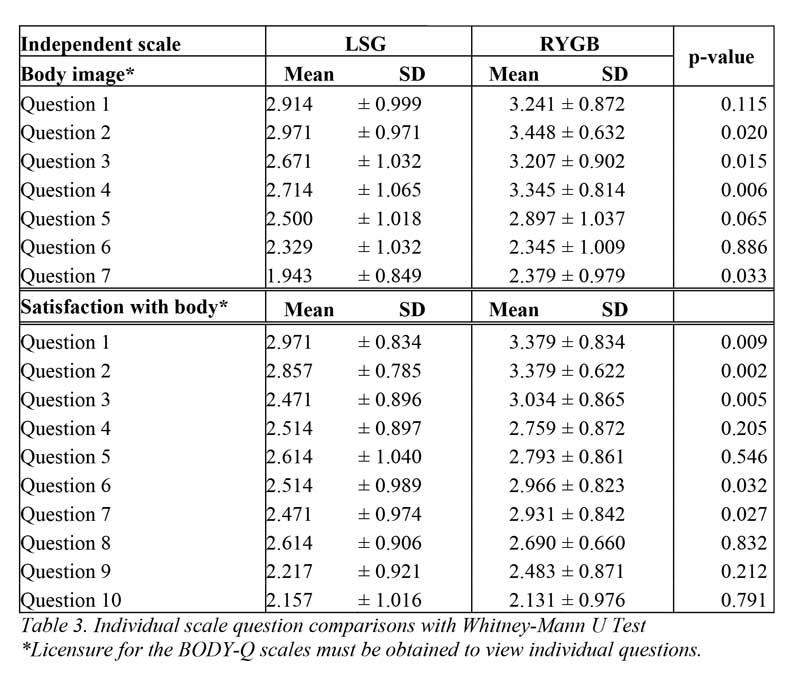
Results: Evaluation showed no significant difference between the component sums of each independent scale when comparing the LSG and RYGB populations. Regarding the body image scale, RYGB patients reported better outcomes, compared to LSG patients, in four of seven questions. Significant differences in patient scoring were observed in five out of 10 of the satisfaction with body scale questions, indicating better reported outcomes in the RYGB cohort. All other answers showed no significant difference between procedure type. Postoperative body mass index (BMI) differed significantly, with the RYGB group (mean±standard deviation [SD]: 34.05±11.53kg/m2) having lower means than the LSG group (mean±SD: 37.71±8.28kg/m2).
Conclusion: These findings suggest that there are no significant differences in PROs related to body image, physical function, physical symptoms, and satisfaction with body among LSG and RYGB cohorts. However, individual questions within the body image and satisfaction with body scales exhibited more positive outcomes among the RYGB group, which may be explained by corresponding findings of lower mean BMI, compared to LSG patients.
Keywords: Bariatric surgery, PROM, sleeve, gastric bypass, roux-en0y gastric bypass, patient reported outcomes, health related quality of life
Bariatric surgery has proven pivotal in improving the health-related quality of life (HRQoL) of patients with complex metabolic syndromes and obesity resistant to traditional lifestyle modification and pharmaceutical intervention.1 Laparoscopic sleeve gastrectomy (LSG) and laparoscopic Roux-en-Y gastric bypass (RYGB) are two of the most popular and efficacious treatments for these patients. At the genesis of gastrointestinal surgery in the late 19th century, RYGB was described by surgeon César Roux.2 Originating as a technique to develop favorable gastric, esophageal, and biliary drainage, the technique fell out of favor over the first half of the 20th century. Since then, RYGB has made a considerable comeback, as ways to mitigate postoperative sequelae associated with the procedure have been developed. Although it has many indications today, it is commonly employed as an intervention for weight loss.2 The sleeve gastrectomy for treatment of morbid obesity was first described in 1991. It served as an element of biliopancreatic diversion and was subsequently performed laparoscopically in the early 2000s.3–5 It swiftly grew in popularity due to its efficacy in substantially increasing estimated weight loss (EWL). LSG and RYGB, while revolutionary for those in need of massive weight loss, are physical procedures that necessitate adequate surgical planning with careful consideration to the risk of peri- and postoperative adverse outcomes.
Patient-reported outcomes (PROs) remain one of the most influential measurements guiding bariatric surgical teams, helping teams to determine both differing surgical approaches and surgical versus medical management.6 These data points provide valuable perspectives that guide surgical planning and prompt further optimization of management strategies. Study results assessing PROs over the last two decades have remained less conclusive than other studies, as they are hindered by a lack of generalizability and notable risk of bias.7 The development and subsequent legitimization of the BODY-Q PROs measure (PROM) enabled researchers to perform bariatric-specific analysis that is be both exhaustive and more readily compared across clinical settings and health systems.8–12
Notable physical and psychological changes are observed in the postoperative period and have increasing relevance in optimizing patient care and improving overall prognosis. Many of these changes are associated with patient perception of their own body, physical function, and physical symptoms. The purpose of this study is to evaluate LSG and RYGB on four independent scales using the BODY-Q. We hypothesize that there will be no significant difference in scoring on all utilized scales between LSG and RYGB patients.
Methods
Participants. In this retrospective cohort study, participants were recruited from the Augusta University Center for Obesity and Metabolism for a retrospective cohort study. Bariatric patients were contacted via email with web links and information on how to complete the BODY-Q survey.
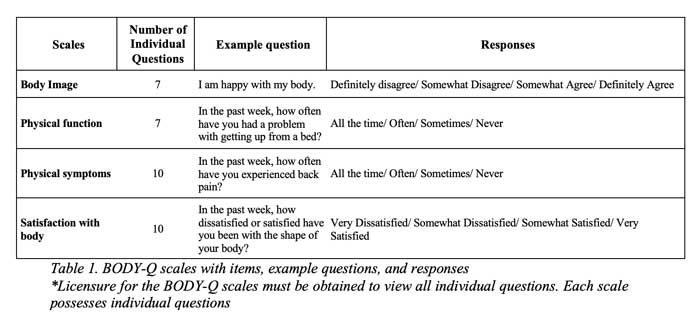
BODY-Q PROM. Licensure for the BODY-Q PROM was obtained for the purposes of this study. The survey design implemented specific scales within the BODY-Q to measure patient-reported satisfaction and postoperative improvements in health. Each scale within the BODY-Q is standardized and can be used independently, allowing the team to design a specific survey optimal for this study. The independent scales utilized in the survey were body image, physical function, physical symptoms, and satisfaction with body. Response options for the BODY-Q ranged and scored from 1 to 4; examples of response options can be seen in Table 1. Raw sums of each independent scale were used for analysis. Details are summarized in Table 1.
Data collection and analysis. All participants were offered a cover letter and consent form. Consenting patients were presented the survey digitally through the QualtricsXM platform. Submissions were deidentified and securely stored using the QualtricsXM server. Surveying was performed from April to September 2021. Averaged scores from individual questions and independent scale raw sums were compared using Mann-Whitney U tests. Data analysis was performed using R-Studio. A p-value below 0.05 was considered statistically significant.
Surgical procedures. Patients underwent either LSG or RYGB with or without robotic assistance. Two primary surgeons performed all operations, utilizing four working ports and an epigastric Nathanson retractor.
LSG was performed in standard fashion, with the removal of approximately 80 percent of the stomach. The branches of the gastroepiploic and short gastric arteries were divided, and the greater curve of the stomach was skeletonized to the crus of the diaphragm. The creation of the gastric sleeve was then performed over an endoscope. Leak tests were subsequently completed with the previously placed endoscope.
RYGB was performed in an antecolic/antegastric fashion. Following creation of the gastric pouch, a loop of jejunum, 40cm distal to the ligament of Treitz, was brought to the posterior side of the gastric pouch to create the side-to-side gastrojejunostomy with a linear stapler. The loop of jejunum was then transected. A 125cm Roux limb was measured, and a side-to-side jejunojejunostomy with the biliary limb was created. Mesenteric defects were closed with permanent suture. An endoscope was introduced to perform leak tests.
Results
Of the 102 RYGB patients contacted, 29 completed surveys. Of the 233 LSG patients contacted, 70 completed surveys. The total number of participants was 99; 70.7 percent received LSG, and 29.3 percent received RYGB.
Evaluation showed no significant difference between the averaged raw sums of each independent scale when comparing the LSG and RYGB populations (Table 2). Further analysis showed a significant difference among individual responses within the body image scale, with RYGB patients reporting better outcomes, compared to LSG patients, in four of seven individual questions. Significant differences in patient scoring were observed in five out of 10 of the satisfaction with body scale questions, indicating better reported outcomes in the RYGB cohort (Table 3). All other answers showed no significant difference between procedure type. Patient body mass index (BMI) by procedure differed significantly, with the RYGB group (mean±standard deviation [SD]: 34.05±11.53kg/m2) having a lower mean than the LSG group (mean±SD: 37.71±8.28kg/m2).
Discussion
LSG and RYGB are the two most common bariatric and metabolic surgeries performed for safe and effective weight loss and improvement in comorbid conditions. The improvement in diabetes mellitus following these procedures is superior to intensive medical management.13 Conclusions drawn on the risks and benefits of LSG and RYGB in terms of weight loss surgery hold tremendous value in patient-centered care. Increasing significance is being placed on data points obtained from patient reports. Utilizing PROMs, such as the BODY-Q, enhances efforts to better describe the trends in postoperative patient-reported satisfaction. With an expanded understanding of physical and psychosocial measures of HRQoL, clinically relevant improvements in surgical planning can be made.
Measured outcomes were similar between the LSG and RYGB cohorts across all independent scales. Such findings support the hypothesis that no significant difference in PROs exist between surgical procedure types. Significant differences between mean BMI in the two cohorts were observed, with a lower mean in the RYGB group, which is consistent with current literature. It is unclear whether these differences were due to differences in EWL since intervention, as patient deidentification did not permit exhaustive review of patient histories. Individual questions within the body image and satisfaction with body scales suggested better outcomes among the RYGB cohort (Table 3). The observed association between averages of individual question responses and patient BMI suggests a plausible relationship between patient views on body image and overall satisfaction and current habitus. The remaining scales, physical function and physical symptoms, showed similar findings between the two groups for each individual question. The observed findings show that the greatest discrepancy between individual answer choices in scales is more closely tied to psychosocial aspects of post-bariatric care, compared to reported physical improvement after intervention, which might also be related to the BMI variation among the cohort groups (Table 3). It is important to note, however, that the BODY-Q scales are designed to be compared as sums of collective questions, rather than individual question averages themselves. Thus, little can be drawn from this observation, given that no statistical difference was seen in all-scale mean sums (Table 2).
In the last two decades, numerous studies have compared outcomes of LSG and RYGB. Some of these studies have focused on weight loss, postoperative complications, and metabolic changes, including disease and symptom resolution. Results remain varied, with some studies reporting increased efficacy of one modality and others showing similar efficacy between procedures.14–17 More recent studies using the BODY-Q show significantly improved EWL and increased postprandial symptoms following RYGB, compared to LSG.18,19 Studies have also successfully used the BODY-Q to assess specific weight loss interventions in an independent fashion using similar scales.20 However, there is limited data in the literature comparing LSG to RYGB with the BODY-Q, and further research is needed to better assess trends in PROs using this tool.
A future non-deidentified five-year study of new candidates undergoing LSG or RYGB will achieve a more robust analysis of candidates at various stages of their postoperative period, with special consideration given to patient demographic information, comorbidities, and lifestyle behaviors. During response collection, a participant sent an individual email to a member of the data-handling team expressing regret for undergoing surgery due to the unfavorable aesthetics of excess skin. This instance presents another unique avenue with which to further utilize the BODY-Q within an interdisciplinary study among surgical specialists that may better discuss the toll massive weight loss takes on patients with and without subsequent body contouring surgery. Such studies have proven to be areas of keen interest within the field and could present clear guidance on how to navigate complex mental and physical health concerns within the community.8,21,22
Limitations. The main, inherent bias of our study is the nonresponse bias, with a response rate of 29.5 percent. We believe that the information we were able to obtain can give insight to differences in outcomes using the BODY-Q tool. To improve response rates, the BODY-Q survey could be collected from patients at their scheduled postoperative visits. This retrospective cohort study served as a pilot study implementing BODY-Q scales and was limited in its capacity to analyze identifiable information, as all participants were deidentified. This limitation might have prevented a more accurate assessment of potential confounders or modifiers leading to observed findings. Factors, such as, but not limited to, EWL, socioeconomic status, time since intervention, and having received body contouring surgery, could have significant effects on PROs and overall scoring.
Conclusion
Findings show the body image and satisfaction with body scales of the BODY-Q exhibited more positive outcomes among the RYGB group, which may be explained by corresponding findings of lower mean BMI, compared to the LSG group. There were no significant differences when comparing PROs related to body image, physical function, physical symptoms, and satisfaction with body among the LSG and RYGB cohorts. More data from a prospective study is needed to better understand how patient demographics, EWL, and time since intervention can play a role in PROs. Conclusions drawn on the risks and benefits of LSG and RYGB in weight loss surgery hold tremendous value in patient-centered care. Increasing significance is being placed on data points obtained from patient reports. Utilizing PROMs, such as the BODY-Q, enhances efforts to better describe the trends in postoperative patient-reported satisfaction. With an improved understanding of these outcomes, clinically relevant improvements in surgical planning can be made, which should lead to better patient satisfaction.
Ethics Statement
This study was approved by the Institutional Review Board of The Medical College of Georgia at Augusta University.
Author Contributions
Mr. Amarath served as lead manuscript writer and aided in study design and data collection. Mr. Beauchamp aided in manuscript writing, study design, and data collection. Mr. Devarakonda served as the study’s statistician. Drs. Stadsvold and Bolduc aided in manuscript writing. Dr. Hilton served as the study’s principal investigator.
References
- Lindekilde N, Gladstone BP, Lübeck M, et al. The impact of bariatric surgery on quality of life: a systematic review and meta‐analysis. Obes Rev. 2015;16(8):639–651.
- Hutchison RL, Hutchison AL. César Roux and his original 1893 paper. Obes Surg. 2010;20(7):953–956.
- Scopinaro N. Why the operation I prefer is biliopancreatic diversion (BPD). Obes Surg. 1991;1(3):307–309.
- Marceau P, Biron S, St Georges R, et al. Biliopancreatic diversion with gastrectomy as surgical treatment of morbid obesity. Obes Surg. 1991;1(4):381–386.
- Ren CJ, Patterson E, Gagner M. Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg. 2000;10(6):514–523.
- Simonson DC, Halperin F, Foster K, et al. Clinical and patient-centered outcomes in obese patients with Type 2 diabetes 3 years after randomization to Roux-en-Y gastric bypass surgery versus intensive lifestyle management: the SLIMM-T2D study. Diabetes Care. 2018;41(4):670–679.
- Coulman KD, Abdelrahman T, Owen‐Smith A, et al. Patient‐reported outcomes in bariatric surgery: a systematic review of standards of reporting. Obes Rev. 2013;14(9):707–720.
- Klassen AF, Cano SJ, Alderman A, et al. The BODY-Q: a patient-reported outcome instrument for weight loss and body contouring treatments. Plast Reconstr Surg Glob Open. 2016;4(4):e679.
- Klassen AF, Cano SJ, Kaur M, et al. Further psychometric validation of the BODY-Q: ability to detect change following bariatric surgery weight gain and loss. Health Qual Life Outcomes. 2017;15(1):227.
- Poulsen L, McEvenue G, Klassen A, et al. Patient-reported outcome measures: BODY-Q. Clin Plast Surg. 2019;46(1):15–24.
- de Vries CEE, Kalff MC, Prinsen CAC, et al. Recommendations on the most suitable quality‐of‐life measurement instruments for bariatric and body contouring surgery: a systematic review. Obes Rev. 2018;19(10):1395–1411.]
- de Vries CEE, Mou D, Poulsen L, et al. Development and validation of new BODY-Q scales measuring expectations, eating behavior, distress, symptoms, and work life in 4004 adults from 4 countries. Obes Surg. 2021;31(8):3637–3645.
- Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376(7):641–651.
- Silecchia G, Boru C, Pecchia A, Rizzello M, et al. Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients. Obes Surg. 2006;16(9):1138–1144.
- Lakdawala MA, Bhasker A, Mulchandani D, et al. Comparison between the results of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass in the Indian population: a retrospective 1 year study. Obes Surg. 2010;20(1):1–6.
- Khan S, Rock K, Baskara A, et al. Trends in bariatric surgery from 2008 to 2012. Am J Surg. 2016;211(6):1041–1046.
- Gu L, Huang X, Li S, et al. A meta-analysis of the medium-and long-term effects of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass. BMC Surg. 2020;20(1):30.
- Mou D, de Vries CEE, Tesfasilassie T, et al. Using the novel BODY-Q bariatric module patient-reported outcomes measures tool to compare sleeve gastrectomies against Roux-en-Y gastric bypasses. J Am Coll Surg. 2019;229(4 Suppl 1):S31–S32.
- Mou D, DeVries CEE, Pater N, et al. BODY-Q patient-reported outcomes measure (PROM) to assess sleeve gastrectomy vs. Roux-en-Y gastric bypass: eating behavior, eating-related distress, and eating-related symptoms. Surg Endosc. 2021;35(8):4609–4617.
- Varban OA, Bonham AJ, Finks JF, et al. Is it worth it? Determining the health benefits of sleeve gastrectomy in patients with a body mass index<35 kg/m2. Surg Obes Relat Dis. 2020;16(2):248–253.
- Klassen AF, Cano SJ, Scott A, et al. Assessing outcomes in body contouring. Clin Plast Surg. 2014;41(4):645–654.
- Bennett BL, Grilo CM, Alperovich M, Ivezaj V. Body image concerns and associated impairment among adults seeking body contouring following bariatric surgery. Aesthet Surg J. 2022;42(3):275–282.
Category: Online Only, Original Research



