Impact of a Hub-and-spokes Healthcare Model for Obesity Treatment Improving Patient Care through Affordability in the Veneto Region, Italy
 by Mirto Foletto, MD; Luca Busetto, MD; Roberto Vettor, MD; Claudio Pilerci, MD; and Domenico Mantoan, MD
by Mirto Foletto, MD; Luca Busetto, MD; Roberto Vettor, MD; Claudio Pilerci, MD; and Domenico Mantoan, MD
Drs. Foletto, Busetto, and Vettor are from the Department of Medicine, University of Padua, Padua, Italy. Drs. Pilerci and Mantoan are from Health and Social Services of the Veneto Region in Venice, Italy.
FUNDING: No funding was provided
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
Bariatric Times. 2018;16(1):14–17.
Abstract: Background: Obesity is the plague of modern society. The related healthcare costs continually clash with budget constraints, and bariatric practice with its interdisciplinary demands requires dedicated resources and expertise that are mainly institution related. No local health authority has yet implemented a plan to coordinate the bariatric activity within the administered territory. The Veneto Region of Italy has a population of more than 6 million inhabitants and a prevalence of obesity around nine percent. The Regional Administration is the primary healthcare provider and payor. Healthcare at large is delivered through dedicated networks of care. We promoted the constitution of a bariatric network involving all the regional institutions devoted, with the support of Regional Health Authority. Rationale: The establishment of a regional bariatric network, called Rete Obesità Veneto, has many advantages in terms of resource allocation, standard healthcare provision, extensive and appropriate coverage for population, risk management, and costs containment. Method: The network is based on a hub-and-spokes model, where both hub and spokes centers deliver comprehensive care to patients with obesity. Common pathways of care are shared by the affiliated centers of the network. Inpatient/outpatient activities and outcomes are assessed and recorded according to the Regional Authority requirements and subject to audits. Results: The bariatric network was approved at the end of 2016. It network currently encompasses one hub and six spoke centers scattered throughout the Region, with consolidated bariatric practice and facilities. The hub is also the Regional referral and coordination center for obesity. Conclusions: The aim of Rete Obesità Veneto is to deliver the best patterns of care for people with obesity, with the goals of improved outcomes, reduced care variability, and reduced costs. Longitudinal assessment will provide new insights on the best practices for this patient population.
Keywords: obesity, bariatric surgery, Veneto, Italy, obesity network, integrated care pathway, hub-and-spokes healthcare model
Obesity is a plague on modern society. In Italy, the mean rates for overweight and obesity are 35.3 and 9.8 percent, respectively.1 Excess weight is not only one of the top five leading causes of death, it also has relevant impact on public health, both at an individual and population level2 with estimated costs per year in Italy alone exceeding 8 billion Euros.3
In Italy, health is a fundamental constitutional right,4 and healthcare provision is equally granted to all Italian citizens. Given these premises, national healthcare is funded by public money within a regional-based framework that was put in place to guarantee the same accessibility, costs, accountability, and quality across the Country. To address these demands, each Italian region has developed individual healthcare plans.
The government of the Veneto Region ruled that healthcare provisions are to be delivered through dedicated networks of care (e.g., Oncology Network, Stroke Network) according to the guidelines reported on the Regional Healthcare Plan (Regional Law No. 19/2016). The network for obesity was approved and included in this plan in February 2016.
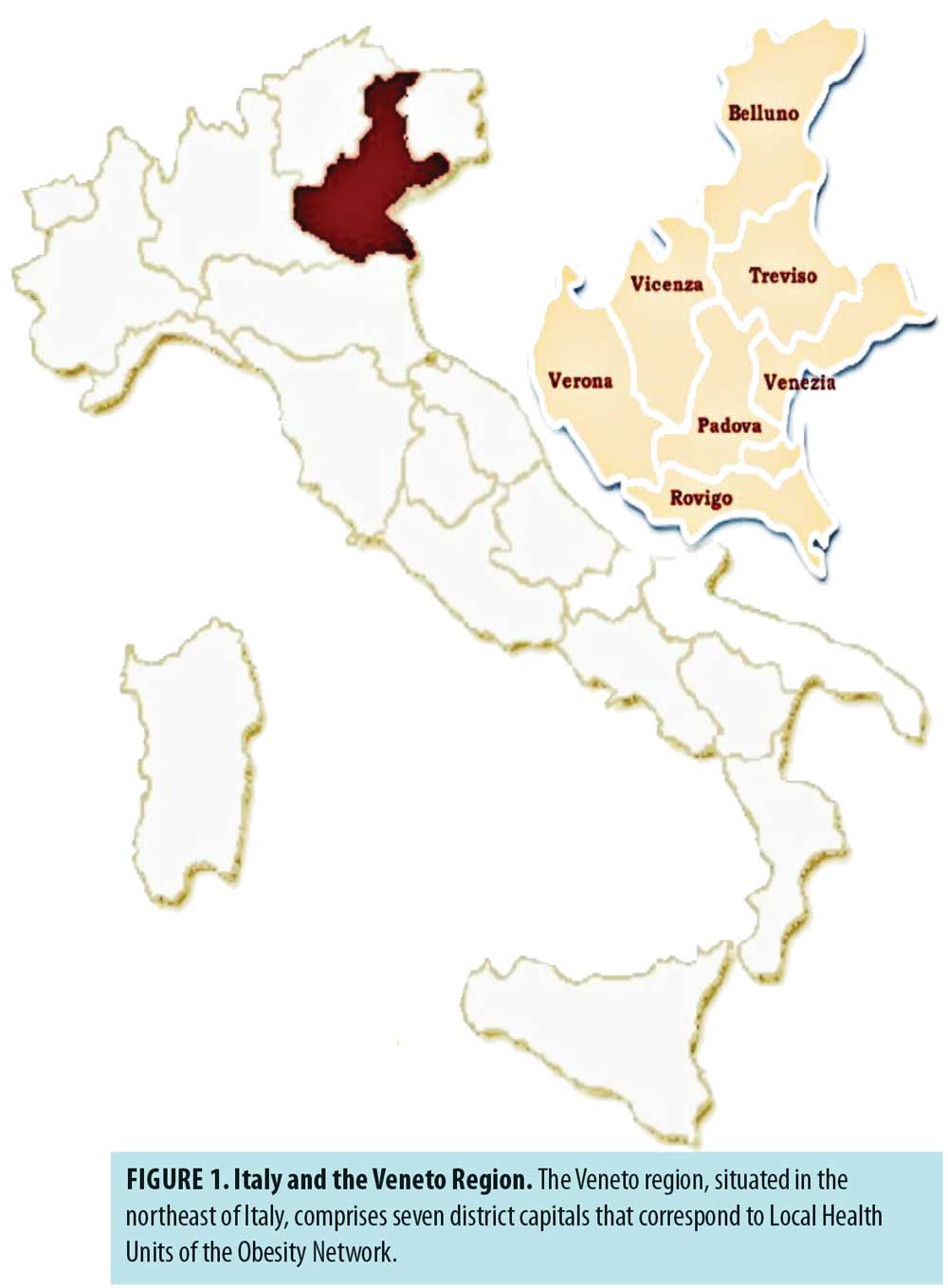
Moreover, healthcare provision are locally delivered and administered through Local Healthcare Units (LHU), geographically based in seven districts of Veneto (Figure 1). The Veneto Region has a population of 6 million inhabitants. Overweight and obesity rates among adults are 34.5 and 9.6 percent, respectively.1 This means that at least 1 out of 10 people seeking healthcare has obesity and requires proper resource allocation in terms of facilities, logistics, expertise, provision-related costs (e.g., medications) regardless of whether bariatric surgery is even considered. The “globesity challenge” spurs overall healthcare-related cost to soar and subsequently clash with budget constraints. These considerations directly involve the Regional Administration, as it is the primary healthcare provider and payor.
Given the clinical complexity behind obesity, the interdisciplinary nature of bariatric practice demands dedicated resources and expertise that are mainly institution-related. Neither national nor local health authorities have yet implemented a plan to coordinate the bariatric activity within ruled territories. In cooperation with the Regional Health Authority we have promoted the constitution of a Bariatric Network (Rete Obesità Veneto – RObV) in the wake of the Regional Healthcare Plan, involving all the existing Institutions and healthcare providers committed to the treatment of obesity.
Rationale
There is a logic in setting up a regional bariatric network in terms of resource allocation, standard healthcare provision, extensive and appropriate coverage for population, risk management, and costs containment. Moreover, such a network can significantly promote research and partnership.
Methods
As with other Regional Networks of Care, RObV is based on a hub-and-spoke model. The large “hub” center and smaller “spoke” centers are set up to deliver comprehensive care to patients with obesity. The hub is responsible for planning and coordination according to Regional Health Authority. The hub also serves as an end-referral tier for spoke centers and headquarters for research and partnerships programs. The development of RObV was designed according to the following milestones:
- State of the art obesity in Veneto. A position paper was prepared by the Bariatric Unit of Padova to address the epidemiological relevance and the impact on health care of general population at a regional level. This paper was presented to the Regional Health Authority.
- Constitution of a regional interdisciplinary obesity working group. The Regional Administration invited all the healthcare professionals involved in obesity treatment to take part in a regional interdisciplinary obesity working group (IOWG). The final aim was to develop and share common clinical pathways and protocols of care on the basis of available published literature and guidelines.
- Draft of the Integrated Care Pathway on Obesity Official Document. The IOWG was assigned to draft the official Integrated Care Pathway (ICP) for the Veneto Region to be approved and published by the Regional Health Authority in its official bulletin (Bollettino Ufficiale della Regione del Veneto [BUR]).
- Establishing interdisciplinary obesity teams at the LHU level (hub and spokes). Every LHU had to establish an interdisciplinary obesity team (IOT) involving all the healthcare professionals (i.e., physicians, surgeons, integrated health) devoted to comprehensive obesity care and nominate a team leader for Institutional contacts.
- RObV semi-annual meetings. To align and update the clinical practice and activities of hub and spoke centers, dedicated one-day (maximum 7 hour) semi-annual RObV Meetings (Fall and Spring) were established and directly promoted by the Regional Health Authority, including continuing medical education (CME) credits allowance. The general format was divided into two sessions. The first session covered different topics related to physiology of the obesity disease, with a keynote lecture, presentations by RobV speakers, and a general discussion. The second session provided an RObV update based on results of questionnaires delivered to the participating centers on local achievements and critical issues. A discussion on future perspectives and proposals followed.
- Central Audit (Regional Administration) to assess RObV outcomes.
Results
The first move of RObV stemmed from the Institutional ICP on Obesity published in 2012 by the Interdisciplinary Obesity Group of Azienda Ospedaliera-Università of Padova. This document aimed to regulate the comprehensive care of obesity within this institution according to up-to-date standards of care.5
A position paper was then presented to the Regional Health Authority with data regarding the epidemiology and the state-of-the-art obesity healthcare in the Veneto Region. The paper was based on regional data derived from the reports of two periodic epidemiologic surveys conducted by the Italian National Institute of Health (Istituto Superiore di Sanità) on the adult and pediatric Italian population.6,7
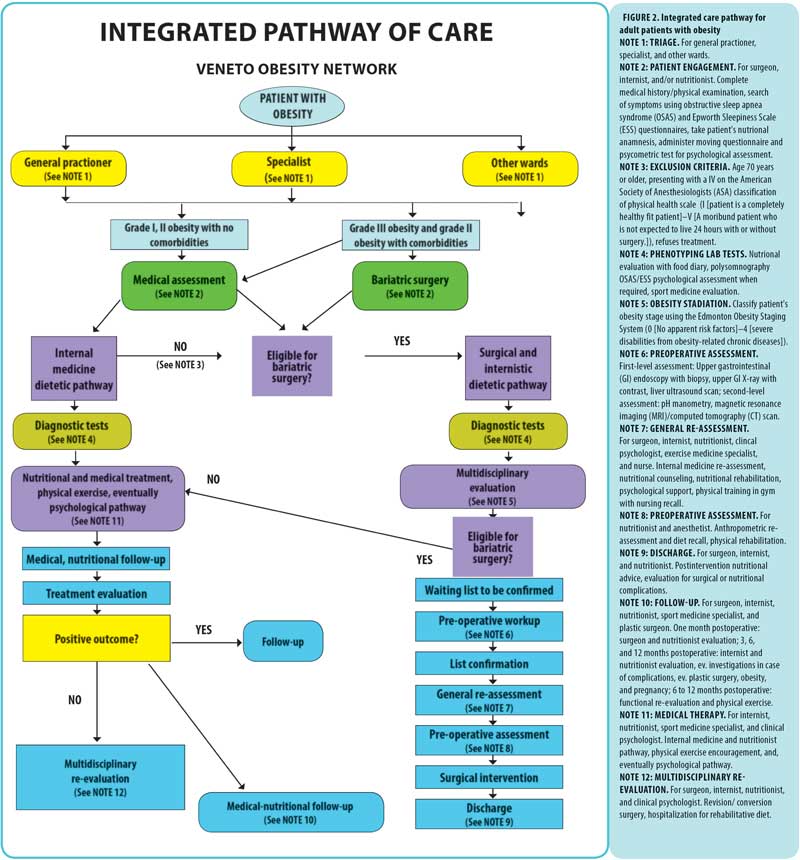
The Regional Administration designated the Padova University Hospital (Azienda Ospedaliera-Università of Padova) as the Hub Center of Comprehensive Obesity Care for the Veneto Region in 2015.8 The IOWG was then established to promote the constitution of RObV and draft the Regional ICP on Obesity. In 2016, the Regional Administration ruled to include RObV in the Regional Network of Care system.9 Accordingly, the general manager of each LHU had to promptly establish a local IOT to activate RObV at both hub and spokes levels and nominate a team leader. The Official Regional ICP on Obesity was finally approved and published in 201710 and represents the clinical referral for bariatric practice in the Veneto Region. The ICP provides clear guidelines for the referral of patients with obesity to medical obesity clinics or to the bariatric units, according to the severity of obesity and its related complications. Moreover, indications and contraindications to bariatric surgery are clearly specified, and the diagnostic minimal multidisciplinary workup for patients assigned to both medical and surgical obesity management is indicated. Finally, the multidisciplinary follow-up and the re-assessment of the clinical outcomes are considered as an integral part of the clinical pathway (Figure 2).
RObV Semiannual Meetings were preceded by two regional events. The first event occurred after the Network approval and aimed to promote and disseminate RObV at the LHU level. The second event was dedicated to presentation of the Regional ICP on Obesity, drafted by the IOWG and approved by the Regional Health Authority, which was to publish in the BUR. The Spring 2017 (June) meeting, focused on “Obesity Unit” in terms of clinical daily practice and research opportunities. The Fall 2017 (October) meeting focused on new concepts of obesity, such as basic science, new pharmacological approaches, and advantages and limitations of metabolic surgery. The Spring 2018 (June) meeting focused on Obesity ICP. Specific areas of concern included Health Technology Assessment (HTA), costs, adequacy and issues, with extra time to address body image, sex, fertility, and pregnancy after bariatric surgery. The Fall 2018 meeting (October) involved regional general practioners in an effort to consolidate and fulfill the link between hospitals, patients, and family doctors. All the events achieved the financial coverage through ad-hoc partnerships with private investors. At present time, Central Audit is not fully operating.
Discussion
Although the prevalence of severe obesity is significant and well rooted in modern and developed societies, and the impact in terms of comorbidity, disability, and social discomfort are well known, the penetration of comprehensive obesity treatment is not yet satisfactory. Generally, there is little compassion shown to individuals who struggle with food choices and portion control, and thus, stigmatization exists. Obesity is more than just quantity and quality of food,11,12 it often involves genetics, environment, and environment-gene interaction. The misalignment between the obesity epidemic with related health costs and the provision of adequate comprehensive obesity management will not be solved without taking into account the two major issues affecting the provision of care in different models—accessibility and allotted resources. In Italy, healthcare provision should be equally granted to all citizens, but this must be done by matching resource allocation with healthcare costs and budget constraints. In this scenario, comprehensive obesity care centers compete for resources with other diseases or healthcare needs, like cancer and transplantation, and this presents a challenge. Increased social awareness, empathy, and compassion surrounding individuals with obesity might result in a more powerful political and financial yield, thus facilitating the allocation of resources for obesity care.
The best way to achieve this goal was to act within the Regional Healthcare Plan, gathering all the involved professional caregivers around the same ICP and within the same network (RObV). Joining forces provided two immediate advantages: equal accessibility for citizens across the regional territory with direct cost containment for the community. The adoption of common validated and shared clinical practices could also improve the quality of care at large, preventing stigmatization while enhancing patients’ engagement. Moreover, the creation of a network of clinical units specifically dedicated to obesity management may facilitate the access to this type of care to the patients, also favoring a better penetration of bariatric surgery, which is currently utilized by less than 0.02 percent of the eligible population.
Central Audit will assess whether all these efforts aimed to improve comprehensive obesity care will translate into a reduction of all direct and indirect costs and increase the penetration of bariatric surgery when deemed a necessary treatment option. Until now, different clinical conditions, such as type 2 diabetes mellitus, nonalcoholic fatty liver disease, and joint degradation, were separately budgeted, although directly related to obesity.
Conclusion
Presently, our biggest achievement has been heightened obesity awareness among policy makers. Ultimately, with proper recognition of the impact of obesity, resources will be allocated. Although a first step, this was a great professional opportunity for both caregivers and managers.
Professional and institutional networking can be reasonable, advantageous, and also cost effective in different settings of healthcare provision, although it demands a higher vision and greater effort to put together different stakeholders.
References
- Istituto di Sanità Pubblica, Sezione di Igiene. Osservatorio Nazionale sulla salute nelle regioni italiane. Rapporto Osservasalute 2016.
- World Health Organization. Obesity: preventing and managing the global epidemic. In: Report of a WHO consultation. WHO Technical Report Series 894. Geneva (Switzerland): World Health Organization; 2000.
- Turchetti G. Indagine sul fenomeno dell’obesità, Scuola Superiore Sant’Anna. 2009.
- La Costituzione della Repubblica Italiana. Parte I, Titolo 2. Articolo 32.
- www.sanita.padova.it
- ISS. Regione del Veneto. PASSI in Veneto. Analisi dei dati attraverso le serie storiche 2008-2016. http://www.epicentro.iss.it/passi/pdf2017/Serie_2008_2016.pdf
- ISS. Regione del Veneto. Okkio alla Salute. Risultati dell’Indagine 2016. http://www.epicentro.iss.it/okkioallasalute/ReportRegionali2016.asp
- Deliberazione della Giunta Regionale n. 2707 del 29 dicembre 2014. BUR n 11 del 27 gennaio 2015.
- Deliberazione della Giunta Regionale n. 142 del 16 febbraio 2016. BUR n 17. Del 26 Febbraio 2016.
- Decreto DEL DIRETTORE GENERALE DELL’ AREA SANITA’ E SOCIALE n. 26 del 09 marzo 2017. BUR n 41s del 28 Aprile 2017.
- Xia Q, Grant SF. The genetics of human obesity. Ann N Y Acad Sci. 2013;1281:178-90.
- Sun X, Li P, Yang X, et al. From genetics and epigenetics to the future of precision treatment for obesity. Gastroenterol Rep. 2017;5(4):266–270.
Category: International Perspective, Past Articles




