Use of the Hill Gastroplasty for Management of Gastroesophageal Reflux Following Sleeve Gastrectomy and Gastric Bypass: A Brief Report
by Matthew T. Gust, MD; Kevin M. Reavis, MD; and Valerie J. Halpin, MD
All authors are with Legacy Weight and Diabetes Institute in Portland, Oregon. Dr. Reavis is with The Oregon Clinic in Portland, Orgeon.
Funding: No funding was provided for this article.
Disclosures: The authors have no conflicts of interest relevant to this article.
Bariatric Times. 2022;19(11):20–21.
Abstract
Objective: Gastroesophageal reflux is a significant problem following bariatric surgery that is often difficult to manage. The Hill repair might offer a solution to this problem.
Design: A brief report of literature concerning our experience with the Hill repair in the management of gastroesophageal reflux and its use in postoperative bariatric surgery patients, with comments on current technique.
Setting: Academic tertiary bariatric center.
Conclusion: There is limited research into the Hill repair in the bariatric surgery population; however, what data there remains encouraging. The Hill repair warrants further investigation as a possible management strategy for gastroesophageal reflux in this population.
Keywords: Gastroesophageal reflux, Hill repair, Hill gastroplasty gastric sleeve, gastric bypass
Gastroesophageal reflux disease (GERD) is a common problem in the bariatric population, both pre- and postoperatively. The sleeve gastrectomy (SG) has been associated with worsening reflux in multiple studies, often seeing a development of de novo reflux in as many as one-third of patients.1,2 The Roux-en-Y gastric bypass (RYGB) has traditionally been seen as a superior option for patients with GERD undergoing bariatric surgery; however, a significant number of patients report GERD symptoms following RYGB.2 In either case, the surgically altered anatomy presents challenges to managing reflux refractory to medical management. This problem is compounded by growing concerns about long term proton pump inhibitor (PPI) use. New technologies, such as the magnetic sphincter augmentation (LINX, Ethicon, Johnson Johnson; Raritan, NJ, US) and radiofrequency treatment (Stretta) procedures, have offered a possible alternative for managing GERD after bariatric surgery. However, insurance coverage for these novel procedures is often difficult to obtain, and long-term reviews are unavailable. Traditionally, the most common treatment pathway for patients with GERD has been medical treatment with PPIs or H2 blockers or SG conversion to RYGB. The Hill anti-reflux procedure offers an alternative treatment approach.
The Hill procedure was first described in 1967 as a treatment for GERD through recreation of the gastroesophageal valve and fixation of the gastroesophageal junction.3 Though an effective repair, it fell to the wayside as the Nissen fundoplication became the repair of choice for most general surgeons, due to its relative simplicity. This trend continued as the procedures moved from open to laparoscopic. In surgically unaltered anatomy, Aye et al4 showed that the Nissen and Hill repairs were functionally equivalent in the management of GERD in both short- and long-term studies.5
Given that the Hill repair is not a true fundoplication, but rather a gastric cardioplasty, it offers a pathway for patients with GERD following bariatric surgery. Both SG and RYGB anatomy can be utilized to recreate the valve mechanism to prevent gastric reflux. Diagnostic evaluation includes manometry, pH testing, and impedance studies, as well as upper endoscopy. We focus on the anatomy of the gastroesophageal junction and proximal portion of the gastric sleeve or pouch. Though we have found few absolute contraindications (e.g., presence of malignancy), we do believe there are some relative contraindications that would make the procedure prohibitively difficult. Presence of extremely short or immobile esophagus, as seen with long segment Barrett’s esophagus or long axial hiatal hernia, would present significant issues with tension in creating the gastric cardioplasty. Size is also a consideration and must be evaluated, though we do not perform formal volumetric studies. In our gastric bypass patients, we have found proximal fundus diameter greater than 3cm and pouch length greater than 3cm are adequate to perform the Hill repair. Similarly, in SG patients, proximal fundus diameter of 3cm would be required.
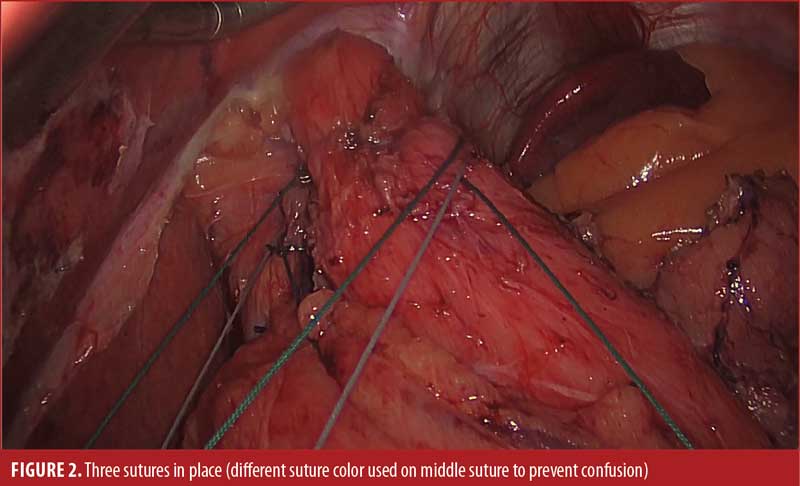
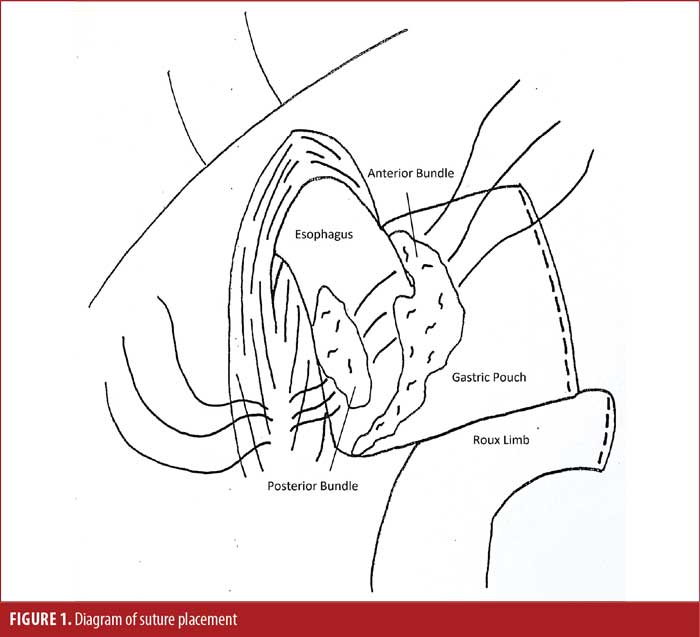
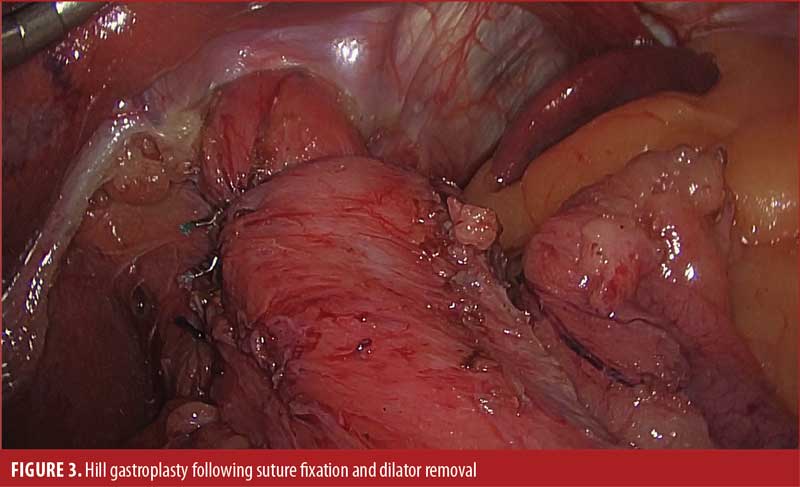
We begin with dissection of the gastroesophageal junction with sufficient mobilization of the intra-abdominal esophagus. If a hiatal defect is noted, it is repaired primarily with posterior interrupted sutures. The anterior and posterior bundles, as well as the Vagus nerves, are identified and preserved. In our reference video, first presented by Pescarus et al,6 four permanent sutures were passed sequentially through the anterior, then posterior, phrenoesophageal bundle of the gastroesophageal junction, then through the preaortic fascia over a 48F dilator. In practice, we have shifted to using three sutures to minimize the risk of postoperative dysphagia (Figures 1 and 2). Classically, Aye et al4 described titrating this repair using intraoperative manometry; however, in practice, that is logistically challenging, and we have not found it to be necessary. Moving forward, there is consideration for the use of intraoperative impedance planimetry (Endoflip™, Medtronic; Minneapolis, MN, US), which could provide an option for tailoring and assessing the results of the operation. The dilator is removed, and an upper endoscopy may by performed with leak test prior to closure (Figure 3).
In a recent case series, our group reviewed 18 patients who underwent Hill gastroplasty following bariatric surgery for GERD from 2014 to 2020.7 GERD was defined as DeMeester score of greater than 14.7 or endoscopic evidence of GERD in the form of Barrett’s esophagus or Los Angeles (LA) class C/D esophagitis. Previous bariatric surgery included 12 RYGBs, four SGs, and two duodenal switches. Nearly all patients (16/18) also underwent a simultaneous hiatal hernia repair at time of Hill gastroplasty. All procedures were performed laparoscopically, and there were no immediate complications. Four patients reported postoperative dysphagia, which was successfully managed with balloon dilation. Quality of life outcomes were obtained from 15 of the 18 patients, with nine patients overall satisfied, three neutral, and three dissatisfied due to persistent symptoms.
As this is a new area of study, there has been limited publication on the topic. We noted recent publications by Gero et al8,9 concerning the use of the Hill repair in the bariatric surgery population. These articles looked at postoperative, as well as simultaneous, Hill repairs in limited case series and demonstrated the principles that we have discussed and future benefits that may be achieved from spreading use of this technique.
Currently, GERD is a major factor affecting the bariatric surgery population. As the utilization of bariatric surgery continues to grow, management of GERD becomes an important topic for every bariatric surgeon. We believe the Hill repair offers a new pathway using well-established techniques to help manage symptomatic GERD in post-bariatric surgery patients. Further studies on long-term recovery and objective measurements of esophageal pH and surveillance endoscopy are indicated to better elucidate true patient benefit.
References
- Oor JE, Roks DJ, Ünlü Ç, Hazebroek EJ. Laparoscopic sleeve gastrectomy and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Surg. 2016;211(1):250–267.
- Leslie D, Wise E, Sheka A, et al. Gastroesophageal reflux disease outcomes after vertical sleeve gastrectomy and gastric bypass. Ann Surg. 2021;274(4):646–653.
- Hill LD. An effective operation for hiatal hernia: an eight year appraisal. Ann Surg. 1967;166(4):681–692.
- Aye RW, Swanstrom LL, Kapur S, et al. A randomized multiinstitution comparison of the laparoscopic Nissen and Hill repairs. Ann Thorac Surg. 2012;94(3):951–957; discussion: 957–958.
- Park Y, Aye RW, Watkins JR, et al. Laparoscopic Hill repair: 25-year follow-up. Surg Endosc. 2018;32(10):4111–4115.
- Pescarus R, Sharata AM, Dunst CM, et al. Hill procedure for recurrent GERD post-Roux-en-Y gastric bypass. Surg Endosc. 2015;30(5):2141–2142.
- Fairley R, Reavis K, DeMeester S, et al. Hill gastroplasty for gastroesophageal reflux disease after bariatric surgery. Presented at: Society of American Gastrointestinal and Endoscopic Surgeons Meeting 2021; August 31–September 3, 2021; Las Vegas, Nevada.
- Gero D, Karila-Cohen P, Marmuse J-P. Simplified laparoscopic Hill repair for the treatment of symptomatic sliding hiatus hernia after bariatric surgery. Surg Obes Relat Dis. 2016;12(8):1630–1634.
- Gero D, Ribeiro-Parenti L, Arapis K, Marmuse J-P. Sleeve gastrectomy combined with the simplified Hill repair in the treatment of morbid obesity and gastro-esophageal reflux disease: preliminary results in 14 patients. World J Surg. 2016;41(4):1035–1039.
Category: Brief Report, Past Articles




