The Growing Knowledge Gap in the Treatment and Management of the Disease of Severe Obesity in Medical Training

by Eileen R. Smith, MD; Bradley S. Kushner, MD; Michael M. Awad, MD, PhD; and Shaina R. Eckhouse, MD
All authors are with the Section of Minimally Invasive Surgery, Department of Surgery, Washington University School of Medicine in Saint Louis, Missouri.
Funding: No funding was provided for this article.
Disclosures: Dr. Shaina R. Eckhouse accepts consultant fees as a consultant for Gore Medical. Dr. Michael Awad accepts educational grants from Applied Medical, Baxter, Bard, Ethicon, Intuitive, Medtronic, and Stryker, as well as consultant fees for Ethicon and Intuitive. Drs. Eileen R. Smith and Bradley S. Kushner have no conflicts of interest or financial ties to disclose.
Bariatric Times. 2022;19(11):12–16.
Abstract
Objective: Although bariatric surgery is effective and safe, current medical school curricula do not supply students with the knowledge and confidence to deliver comprehensive obesity treatment. To better characterize the gap between actual and ideal knowledge of obesity treatment, we explored the understanding of the disease of obesity and its treatment options among medical students and surgical residents.
Design: Surveys were sent to surgical clerkship students and general surgery residents. Residents were used as a reference group, as their experience with bariatric surgery patients gives them a broader understanding of obesity care.
Setting: The study was conducted at an academic medical center.
Participants: The study include medical students and general surgery residents.
Measurements: Data were extracted into Excel 2018 (Microsoft; Redmond, WA, US) and statistical analysis was carried out via MedCalc (Version 20.010; Ostend, Belgium). Rating scales were treated as parametric variables and expressed as mean and standard deviation (SD). Comparisons were performed via student’s t-test. Significance was set at p=0.05.
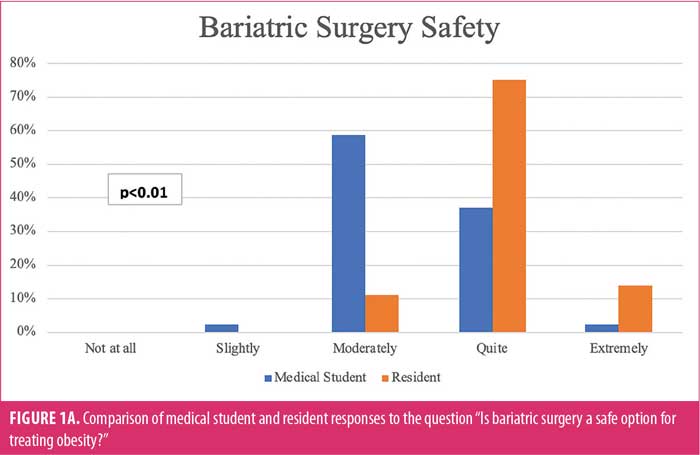
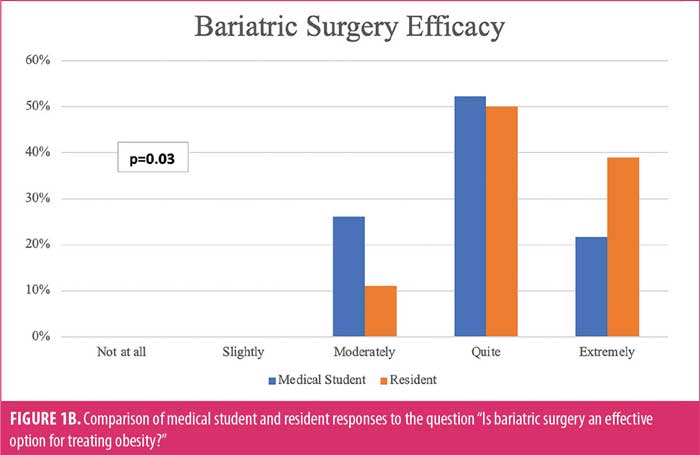
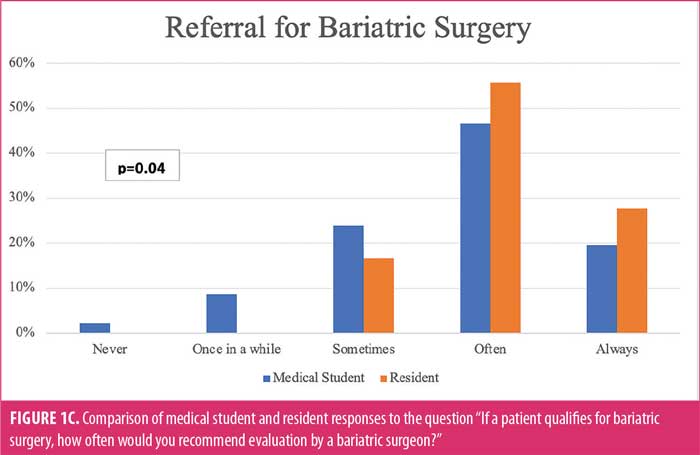
Results: Students perceived bariatric surgery as less safe and effective than did surgery residents (p<0.01 and p=0.03, respectively). Students reported significantly less confidence than residents discussing surgical treatments for obesity, the impact of bariatric surgery on medications, and “weight” with patients (p<0.01, p<0.01, and p<0.01, respectively). Students were less likely to refer a patient with obesity for surgical therapy, even if they met appropriate criteria (p=0.03).
Conclusion: Medical students begin practice lacking critical knowledge of obesity and available treatment options. Further work should be done to drive curricular changes to increase student skills in delivering comprehensive care to patients with obesity.
Keywords: Bariatric surgery, surgical education, complications of bariatric surgery, medical school education, bariatric education
The disease of obesity, recognized officially in 2013 by the American Medical Association (AMA), continues to increase rapidly in the United States (US) and worldwide.1 By the year 2030, it is estimated that 1 in 2 US adults will meet criteria for the disease of obesity.2 In parallel, obesity increases the risk of other medical conditions, including cardiovascular disease (CVD), diabetes, and overall mortality.3,4 Although lifestyle changes, which include diet and exercise, are considered the first step in the management of obesity, bariatric surgery is the most effective treatment for patients with severe obesity and its associated complicating comorbidities.3 It provides superior weight loss maintenance, with better long-term outcomes in decreasing morbidity and mortality, than lifestyle changes and weight loss medications.5–8 Furthermore, bariatric surgery leads to long-term direct healthcare savings, and initial surgery costs may be recovered within 3.5 years.9 Given the ever-increasing public health epidemic and the proven success of weight loss surgery, there is a mounting need for healthcare practitioners who are well versed in all aspects of obesity treatment, including lifestyle changes, medications, and surgical interventions.
To meet the growing need for practitioners versed in obesity medicine, some medical schools have incorporated formalized obesity education programs.10 In the 2017 to 2018 academic year, the Association of American Medical Colleges (AAMC) reported that 103 of 123 participating medical schools reported obesity education as part of the curriculum.11 However, it is clear that the education provided thus far is less than adequate. A 2020 study by Butsch et al10 surveyed medical school curriculum deans and administrators and found that only 10 percent of respondents believed their medical students were “very prepared” to manage patients with obesity.10 Current US physicians do not fare much better; a 2012 survey of US primary care physicians (PCPs) found that, while many doctors were able to identify patients who needed obesity education, less than half could provide specific guidance on treatment.12 Additionally, PCPs were more likely to guide patients on the importance of physical activity rather than diet and weight management, and despite publicly available guidelines, most physicians failed to integrate currently available evidence-based recommendations for advancing obesity management.13 Further still, negative attitudes toward patients with obesity remain prevalent and complicate patient care. Many physicians view patients with obesity as “weak-willed, sloppy, and lazy,”14 and many PCPs feel that these patients lack the discipline to lose weight. Interestingly, these negative attitudes are even more common in younger physicians.14 These trends and attitudes are often attributed to obesity education not being a frequent focus of medical school education and, even if present, it often varies in quality and quantity.15,16
Given the prevalence of obesity, all physicians, regardless of specialty, should have a comprehensive understanding of obesity treatment, including both medical and surgical care. Based on the currently available evidence, we hypothesized that our own institution’s current curriculum might not supply medical students with the needed knowledge and confidence to deliver comprehensive obesity care. To better characterize the gap between the actual and ideal knowledge of obesity treatment at our institution, we sought to compare the knowledge, understanding, and attitudes around the disease of obesity and its associated therapies between current medical students and surgical residents, whose experience caring for bariatric surgery patients gives them a broader understanding of obesity care. As a needs assessment, we sought to identify areas in which we could improve the education and comfort of medical students caring for patients with obesity, and, in the future, set the groundwork for a curricular design that adequately addresses this knowledge gap.
Materials and Methods
This study was approved by our Institutional Review Board. With the input of an experienced attending bariatric surgeon and a senior surgical educator, a set of paired surveys were designed to assess the baseline knowledge, attitudes, and understanding of the disease of obesity among current medical students rotating on their required surgical clerkship, and we compared these results to current surgical residents. The surveys utilized a unipolar rating scale. As part of their required clerkship, medical students are given a series of core lectures by faculty. Immediately prior to their planned educational session on the surgical treatment of obesity, medical students were asked to complete the survey on paper. This group did include several medical students participating in the bariatric surgery service; to preserve anonymity, students were not asked to identify their current rotation. At the time of the survey, students had completed about two weeks of their surgical clerkship. As a comparison, current general surgery residents in all postgraduate years (PGYs) in our institution completed the survey. The survey for surgical trainees was distributed on paper at our weekly educational conferences. Participation for both residents and students was voluntary.
Our current institutional educational offerings on the topic of obesity were reviewed prior to executing this study. The medical student preclinical curriculum includes two hours of lectures on obesity and gut hormones and one hour of lecture on medical management of obesity. Additionally, all medical students receive three lectures on the management of obesity, one focused on genetic causes of obesity and adolescent obesity during their pediatric clerkship, one focused on the impact of obesity on obstetric and gynecologic care, and one focused on bariatric surgery during their general surgery clerkship. A smaller subset of medical students will have direct patient care experience with patients undergoing bariatric surgery, should they rotate on the minimally invasive surgery service. The general surgery resident curriculum on the disease of obesity includes lectures at both the junior and senior resident level, with discussion of both operative and nonoperative therapies, a practical surgical skills lab focused on sleeve gastrectomy and gastric bypass in a porcine model, and dedicated time on bariatric surgical service, with exposure to outpatient and inpatient settings in all years of residency.
All survey responses were kept confidential and anonymous. To allow for direct comparison, the surveys for the students and residents were nearly identical. Both included questions on the respondent’s confidence in discussing obesity treatments (lifestyle changes, medical management, and surgical management), comfort and interest in discussing the disease of obesity with patients, and several specific, knowledge-based questions regarding indications for and outcomes after bariatric surgery. As we recognize there are some differences in the roles and responsibilities of medical students and residents, we wanted to collect some targeted information about each, rather than collect data for comparison’s sake alone. For instance, surgical residents are responsible for completing consent processes for surgeries, so we wanted to know about their comfort level discussing the impact of obesity on surgical procedures in the consent process. This was meant to better inform our needs assessment and allow for more targeted curricular design. While respondents were encouraged to answer all survey questions, each question was considered optional.
Data management. Surveys were distributed on paper, and data were stored in a secure web-based survey platform (QualtricsXM; Provo, UT, US). Data were extracted into Excel 2018 (Microsoft; Redmond, WA, US), and statistical analysis was carried out via MedCalc (Version 20.010; Ostend, Belgium). Rating scales were treated as parametric variables and expressed as mean and standard deviation (SD). Comparisons were performed via student’s t-test. Questions that did not use a rating scale were treated as categorical variables, reported using percentages, and compared via Chi-squared tests. Significance was set at p=0.05.
Results
A total of 46 out of 46 eligible medical students (100% response rate) completed their respective survey (Table 1a). All medical student respondents completed all questions (100% completion rate). The majority of medical students were in their third clinical year (87.0%), and most were exposed to obesity education during their preclinical years (56.5%). However, 17.4 percent of medical student respondents had no obesity education, despite the fact that the vast majority felt that obesity education should be a required component of medical education, both in the preclinical and clinical years (95.6%). Concurrently, 36 of 52 eligible general surgery residents (69% response rate) completed their survey (Table 1b). Again, all resident respondents completed all questions (100% completion rate). Two-thirds of the resident responders were junior trainees (PGY 1 and 2). Among resident respondents, 8.3 percent reported no previous education on the disease of obesity, and 13.9 percent received education on the disease of obesity in residency only. All residents (100%) felt obesity education should be required in either medical school and/or residency education.
Medical students reported significantly less confidence answering patient questions about obesity, discussing bariatric surgery as a treatment for obesity, and understanding the impact of bariatric surgery on medications, compared to resident respondents (p<0.01, p<0.01, and p<0.01, respectively; Table 2). While both medical students and residents felt comfortable answering questions about the disease of obesity, neither group felt confident discussing medications as a treatment; 93.4 percent of medical students and 77.8 percent of residents were either “not at all confident” or “slightly confident” discussing medical therapy. Medical students also had significantly decreased comfort having weight-related conversations with patients, compared to the resident respondents (p<0.01). However, the majority of medical students remained either “quite interested” or “extremely interested” (74%) in further specific training on effective patient communication about “weight.”
Medical students perceived bariatric surgery as both less safe and less effective than general surgery residents (p<0.01 and p=0.03, respectively), and medical students were less likely than surgical residents to refer a patient with obesity for surgical therapy, even if they met the appropriate criteria (p=0.04) (Figures 1A–1C). Furthermore, medical students were less likely to correctly answer the average expected excess percent weight loss of patients following a Roux-en-Y gastric bypass (RYGB) (p<0.01) (Table 3). Medical students also incorrectly felt that bariatric surgery was not a safe option for adolescents. Only 13.0 percent of respondents felt that bariatric surgery was “quite safe” or “extremely safe” for this population.
The survey results focused on the treatment of severe obesity, with an emphasis on surgical therapies. However, the survey also revealed that both medical students and residents lacked confidence discussing medical therapies for obesity. Specifically, 63 percent of students and 50 percent of residents stated they were not at all confident discussing weight loss medications. Additionally, the largest number of medical student and resident respondents stated they were only moderately confident discussing lifestyle changes as a treatment for obesity (46% and 47%, respectively).
Discussion
The prevalence of obesity among adults and adolescents in the US is rapidly increasing.17 Therefore, having a capable working knowledge of the disease of obesity and its related complications, as well as its medical and surgical management, is vital for future medical professionals. To better characterize the current state of obesity knowledge and education in medical education, we queried medical students and surgical residents at our institution about their confidence, interest, knowledge, and exposure to the medical and surgical management of obesity. There are several important findings of this needs assessment. First, medical students at our institution had little confidence discussing the medical and surgical management of obesity with patients and had little comfort discussing “weight” with patients. Second, our medical students had poor literacy on the safety and efficacy of bariatric surgery, despite the overwhelming primary literature suggesting both its safety and efficacy for long-term weight loss. Last, despite this knowledge gap, almost all students recognized the importance of this topic and expressed a desire for a structured curriculum around this chronic illness.
The findings of this needs assessment suggest that while medical students might have exposure to curriculum on the disease of obesity, the volume or type of education they might receive could be inadequate. Our institution includes curriculum on obesity in the preclinical space, but 17 percent of current medical students surveyed reported no prior exposure to obesity training during their undergraduate medical education. Despite obesity’s enormous health and economic impact and its substantial impact on patient care, medical school education on obesity leaves many physicians ill-prepared to address the needs of this population.15,16,18 Structured obesity education is so impactful that previous studies have shown that with at least one hour of obesity training, PCPs are more likely to believe that obesity is a chronic disease process, refer appropriate patients for bariatric surgery evaluation, and feel that bariatric surgery is safe and effective.18 Additionally, physician-identified barriers to caring for patients with obesity have centered around a lack of training in weight counseling and poor knowledge of the tools needed for treating obesity.12 Despite the AMA’s formal recognition of obesity as a separate disease entity in 2013, our findings here suggest that exposure to undergraduate medical students remains varied, and many physicians will still be inadequately trained to treat the enormous health impact of obesity. This knowledge gap was even recognized by the vast majority of both residents and medical students in this study, who desired additional, formalized obesity education curricula.
Bariatric surgery remains the single most effective treatment option for patients with obesity and results in long-term weight loss and significant improvement in obesity-related comorbidities.5 Yet, medical students at our institution lack confidence discussing surgical weight loss with patients and continue to underestimate its safety and efficacy. Furthermore, nearly half of the medical student respondents felt that weight loss surgery in adolescents is unsafe, despite current longitudinal data supporting its safety, its ability for marked weight loss, and its success in resolving diabetes and hypertension.19 Although many medical students will enter into fields other than bariatric surgery, most students will ultimately interact daily with patients with obesity. These future physicians will need to be comfortable caring for and diagnosing patients, as well as referring them to bariatric surgeons. Currently, we are not meeting these goals; in a study that surveyed PCPs about the health professionals most qualified for helping patients lose or maintain weight, bariatric surgeons were not even on the list of chosen answers.12 Access to bariatric surgery is further limited by an obvious deficiency in the knowledge of bariatric surgery among the lay population. In a population-wide study, only 18 percent of respondents felt surgery was the most effective method for weight loss, 65 percent thought bariatric surgery had a greater than 40 percent complication rate, and nearly 50 percent would not advise a patient with morbid obesity to seek a bariatric surgeon’s help.20 Often a patient’s first access to care, the PCP must possess solid fundamental knowledge of the benefits of weight loss surgery to correct patients’ often misguided perceptions on obesity surgery. Students who learn that bariatric surgery is an accepted option for weight loss are more likely to properly refer patients for bariatric surgery.14
Unfortunately, the training of medical students in obesity and its management strategies has not changed significantly in decades.14 Traditional medical education has structured curricula around one discipline or body system, which helps to explain why the disease of obesity is often formally neglected.16 However, the fact that obesity as a disease can transcend traditional barriers should appeal to the increasing interdisciplinary clinical infrastructure of medicine.12 In fact, pilot programs that approach obesity through repeated, interdisciplinary, longitudinal experiences, which allow students to establish relationships with patients, have shown positive effects on student attitudes toward patients with obesity and has increased provider willingness to refer patients for weight loss surgery.14 It should be noted that challenges in developing a comprehensive obesity curriculum are likely multifactorial. As reported by Butsch et al, the undergraduate medical school curriculum is overcrowded, and obesity education is underprioritized. This might be compounded by limited faculty understanding of the topic, lack of relevant standardized testing, and even negative perceptions of the disease of obesity.10 Future work at our institution will utilize the findings of this needs assessment to drive curricular changes aimed at increasing student exposure and enhancing the skill of navigating the disease of obesity through a formalized, multidisciplinary curriculum, with the help of bariatric nurse coordinates, surgeons, nutritionists, and medical weight loss specialists.
Limitations. There are several important limitations of this study to acknowledge. First, although our response rates of 100 percent for medical students and 69 percent for residents are on par with other reported survey-based studies, respondents more familiar or more interested in obesity care were probably more likely to respond. Second, this was a single institutional study of a medical school and residency program associated with a Midwestern academic quaternary care medical center, and the generalizability of the results to other medical schools and residency programs is unknown. As obesity rates vary across the country, future work should examine whether bariatric surgery attitudes vary among multiple different centers and/or training/practice environments (e.g., rural vs. urban). Additionally, there might be a significant element of recall bias at play here, and both student- and resident-reported exposure to obesity curriculum might not reflect reality. Lastly, the comparison group used in this pilot study was composed of general surgery residents. While the majority of resident respondents were juniors in the program, they do receive training in bariatrics as part of their core curriculum. Additional specialized knowledge in both medical and surgical treatments is available in fellowship opportunities. Nevertheless, we feel strongly that the foundation should be set during medical education. In comparing medical students to surgical residents, the study aimed to demonstrate that medical students lack foundational knowledge in this arena, which is important, as the majority will not go on to receive additional training in the management of severe obesity and indications for bariatric surgery. Moreover, this study was meant to be a needs assessment to identify potential gaps in our institution’s education curriculum on obesity, rather than a true head-to-head comparison between medical students and residents, and, as such, the results should be interpreted with caution. Further work to better understand the knowledge gaps should also include fellows focused on the treatment of severe obesity and practicing providers.
Conclusion
Given the prevalence of obesity, all physicians, regardless of specialty, should have a comprehensive understanding of obesity treatment, including both its medical and surgical care. This needs assessment identifies that medical students at our institution are entering the physician workforce lacking key critical knowledge of obesity as a disease and a thorough understanding of available treatment options. Further work will utilize this needs assessment to drive curricular changes aimed at increasing student knowledge and enhancing skill sets to deliver comprehensive care to patients with obesity.
References
- Puhl RM, Liu S. A national survey of public views about the classification of obesity as a disease. Obesity (Silver Spring). 2015;23(6):1288–1295.
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected US state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440–2450.
- Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014;149(3):275–287.
- Garg SK, Maurer H, Reed K, Selagamsetty R. Diabetes and cancer: two diseases with obesity as a common risk factor. Diabetes Obes Metab. 2014;16(2):97–110.
- Keith CJ, Jr., Goss LE, Blackledge CD, et al. Insurance-mandated preoperative diet and outcomes after bariatric surgery. Surg Obes Relat Dis. 2018;14(5):631–636.
- Love KM, Mehaffey JH, Safavian D, et al. Bariatric surgery insurance requirements independently predict surgery dropout. Surg Obes Relat Dis. 2017;13(5):871–876.
- Gerber P, Anderin C, Thorell A. Weight loss prior to bariatric surgery: an updated review of the literature. Scand J Surg. 2015;104(1):33–39.
- Wolfe BM, Kvach E, Eckel RH. Treatment of obesity: weight loss and bariatric surgery. Circ Res. 2016;118(11):1844–1855.
- Sampalis JS, Liberman M, Auger S, Christou NV. The impact of weight reduction surgery on health-care costs in morbidly obese patients. Obes Surg. 2004;14(7):939–947.
- Butsch WS, Kushner RF, Alford S, Smolarz BG. Low priority of obesity education leads to lack of medical students’ preparedness to effectively treat patients with obesity: results from the US medical school obesity education curriculum benchmark study. BMC Med Educ. 2020;20(1):23.
- AAMC curriculum inventory. Curriculum inventory: coverage of obesity education content. https://www.aamc.org/data-reports/curriculum-reports/report/curriculum-reports. Accessed 24 Oct 2022.
- Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians’ perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2(6):e001871.
- Pasarica M, Topping D. An evidence-based approach to teaching obesity management to medical students. MedEdPORTAL. 2017;13:10662.
- Roberts DH, Kane EM, Jones DB, et al. Teaching medical students about obesity: a pilot program to address an unmet need through longitudinal relationships with bariatric surgery patients. Surg Innov. 2011;18(2):176–183.
- Martins C, Norsett-Carr A. Obesity knowledge among final-year medical students in Norway. Obes Facts. 2017;10(6):545–558.
- Banasiak M, Murr MM. Medical school curricula do not address obesity as a disease. Obes Surg. 2001;11(6):677–679.
- Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21(Suppl 1):S1–S27.
- Stanford FC, Johnson ED, Claridy MD, et al. The role of obesity training in medical school and residency on bariatric surgery knowledge in primary care physicians. Int J Family Med. 2015;2015:841249.
- Inge TH, Courcoulas AP, Jenkins TM, et al. Five-year outcomes of gastric bypass in adolescents as compared with adults. N Engl J Med. 2019;380(22):2136–2145.
- Altaf A, Abbas MM. Public perception of bariatric surgery. Saudi Med J. 2019;40(4):379–384.
Category: Original Research, Past Articles




