Raising the Standard: MBSAQIP Patient-reported Outcomes
 by Meridith Greene, PhD, and Matthew Hutter, MD, MPH
by Meridith Greene, PhD, and Matthew Hutter, MD, MPH
Dr. Greene is a Research Scientist at the Codman Center for Clinical Effectiveness in Surgery at Massachusetts General Hospital in Boston, Massachusetts. Dr. Hutter is a General and Laparoscopic Surgeon in the Department of Surgery; Director, Codman Center for Clinical Effectiveness in Surgery, Massachusetts General Hospital Weight Center at Massachusetts General Hospital in Boston, Massachusetts.
Funding: No funding was provided for this article.
Disclosures: The authors report no conflicts of interest relevant to the content of this article.
Bariatric Times. 2020;17(3):18
The Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP) has launched an exciting new Patient Reported Outcomes Measures (PROMs) program that is now available to all participating accredited centers. PROMs are considered the next frontier in healthcare, allowing healthcare providers to capture valid measurement of subjective elements of health. The goal of the MBSAQIP PROMs program is to capture the voice of our patients and better understand what matters most to them regarding their general health, obesity/weight-loss related issues, and quality of life before and after bariatric surgery.
The program, managed by the American College of Surgeons, is available to all MBSAQIP participating centers at no additional cost, and signing up is easy—you just opt-in. Participating centers register preoperative patients using an online portal. Patient name, email, and surgery details are entered. The system then takes over, and automatic emails are sent inviting patients to take the survey before surgery and annually on their surgical anniversary. In addition to three validated surveys selected for the program, postoperative patients are asked about their satisfaction with the decision to have surgery and about their status with the five most common obesity-related comorbidities—hypertension, hyperlipidemia, diabetes, gastroesophageal reflux disease (GERD), and sleep apnea. Upon completion of the survey online, patients receive a report detailing their scores on the three surveys. This report updates each year, allowing patients to track their changes over time.
Participating centers have access to two dashboards. The first displays patient-level data that clinicians (nutritionist, psychologists, nurse practitioners [NPs], and medical doctors [MDs]) are encouraged to view with their patients in the clinic (Figure 1). This provides an opportunity to discuss quality of life, general health outcomes, and changes over time with the patients, and it adds a positive dimension to the postop visits. The second dashboard is intended only for clinicians and provides aggregate data at the surgeon, hospital, and national levels, which can be filtered and compared by bariatric surgery procedure type (Figure 2). You can assess how your patients are doing compared to all the participating centers across the country.
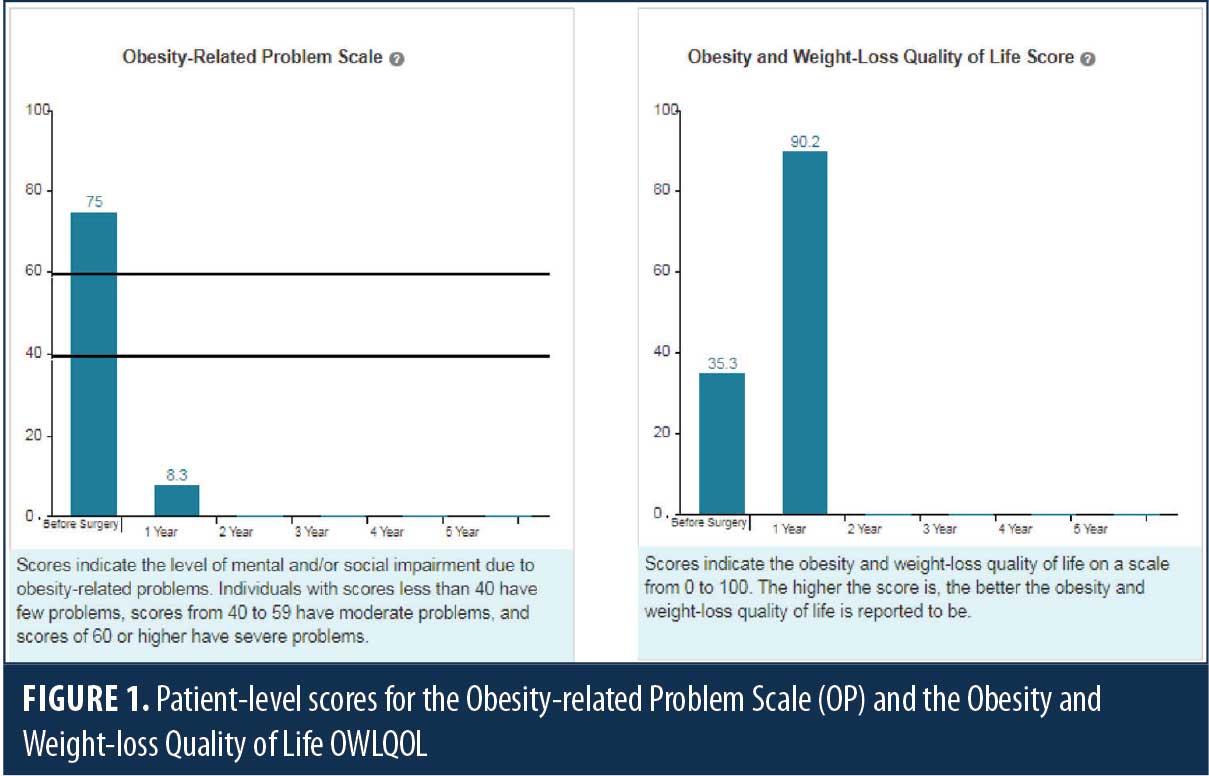
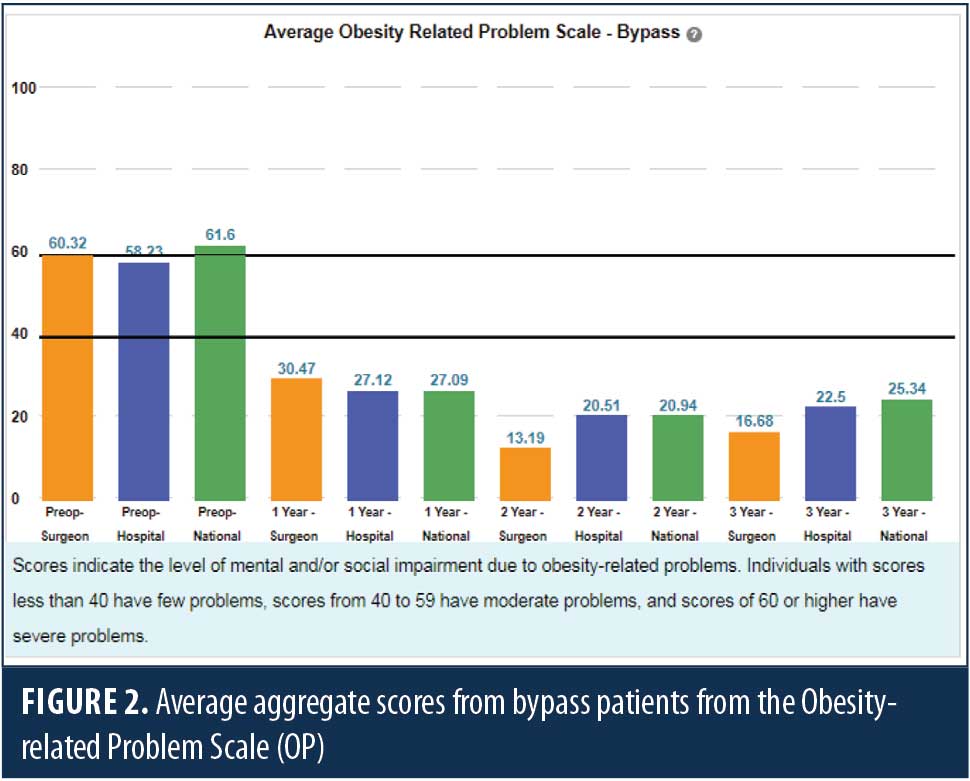
The program was designed with input from preoperative patients, postoperative patients, patient family members, and bariatric healthcare clinicians in a series of more than 20 focus groups and interviews, which were funded by the Patient Centered Outcomes Research Institute (PCORI). Outcomes in the domains of health, activities of daily living, relationship with food, self-esteem, mobility, social/interpersonal issues, sexual life, and work/school were discussed and ranked by the focus group participants. This feedback was used to narrow the field of six general health measures, two symptom measures, and 18 obesity and weight-loss measures for review with the focus groups. The team did not attempt to create any new PROMs for the program, but rather selected from previously validated measures. Following analysis of the feedback from the second round of focus groups, PROMIS 10 was selected to measure general health, and the Obesity-related Problem Scale (OP) and the Obesity and Weight-loss Quality of Life (OWLQOL) Instrument were selected to measure disease specific outcomes. These three surveys comprise the heart of the MBSAQIP PROMs Program.
The program was first piloted in the Boston area at five Partners Hospitals in 2015. It expanded to a national sample in 2016 and is now open to all accredited bariatric programs. Interested centers should complete an electronic opt-in form to join the program. There are currently 60 centers participating in the MBSAQIP PROMs program, with over 10,000 patients enrolled. Feedback from participating centers has been favorable. The automated nature of the program, once the patient is enrolled (which takes less than one minute per patient), makes it user friendly and sets it apart from other MBSAQIP initiatives. Feedback from patients has been overwhelmingly positive. Patients have expressed excitement that their doctors are measuring the things that matter most to them in addition to their weight loss and cessation of comorbidities. They are also excited to be able to track their own progress over time through the program.
The MBSAQIP PROMs program is an exciting opportunity to engage with bariatric patients about their quality of life and general health before and after surgery. Participation in the program is expanding the understanding of how bariatric surgery influences the lives of our patients and could provide insights on who will benefit most from which procedure.
Any accredited center interested in learning more or joining the PROMs program should reach out to the team at the MBSAQIP via email at [email protected]
Category: Past Articles, Raising the Standard




