Spotlight on the Bariatric Program at BayCare Mease Dunedin Hospital
This column is dedicated to featuring accredited bariatric centers around the world, with a focus on their facilities, staff, statistics, processes, technology, and patient care.
by Vicky Blackard, RN, BBA, CBA
Vicky Blackard, RN, is the program manager for Mease Dunedin Hospital’s bariatric program.
Funding: No funding was provided.
Disclosures: The author reports no conflicts of interest relevant to the content of this article.
Bariatric Times. 2017;14(8):16–18.
 Welcome to Mease Dunedin Hospital Bariatric Surgery Program
Welcome to Mease Dunedin Hospital Bariatric Surgery Program
Mease Dunedin Hospital is part of the not-for-profit BayCare Health System, which operates 14 hospitals and five bariatric programs across Tampa Bay and central Florida. Mease Dunedin is a 120-bed acute care facility with nearly 700 employees and recently celebrated 80 years of service to the community. The bariatric program primarily serves clients from upper Pinellas and Pasco counties, though patients have come from all over the state to receive care and undergo surgery at our facility. Our surgeons have been performing bariatric surgeries since 2005. The bariatric program was developed in 2006 and later moved to its primary location at Mease Dunedin, which has proven to be a high-quality destination for bariatric surgical patients. In 2015, the Mease Dunedin Hospital Bariatric Program became the first BayCare bariatric program to receive accreditation from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). Site surveyor Harvey J. Sugerman, MD, FACS, gave Mease Dunedin glowing reviews during the accreditation process.
Our Practice
Our fast-growing bariatric program doubled in surgery cases from 2015 to 2016. Our patients range in age from 20 to 72 (average age: 25 to 40 years). Twelve percent of our patients are over 65, and 85 percent are female. In 87 percent of our cases, patients undergo the vertical sleeve gastrectomy procedure. From January 2016 to June 2017, eight percent of the procedures were Roux-en-Y gastric bypass, and five percent were laparoscopic adjustable gastric band (LAGB) removal or revision.
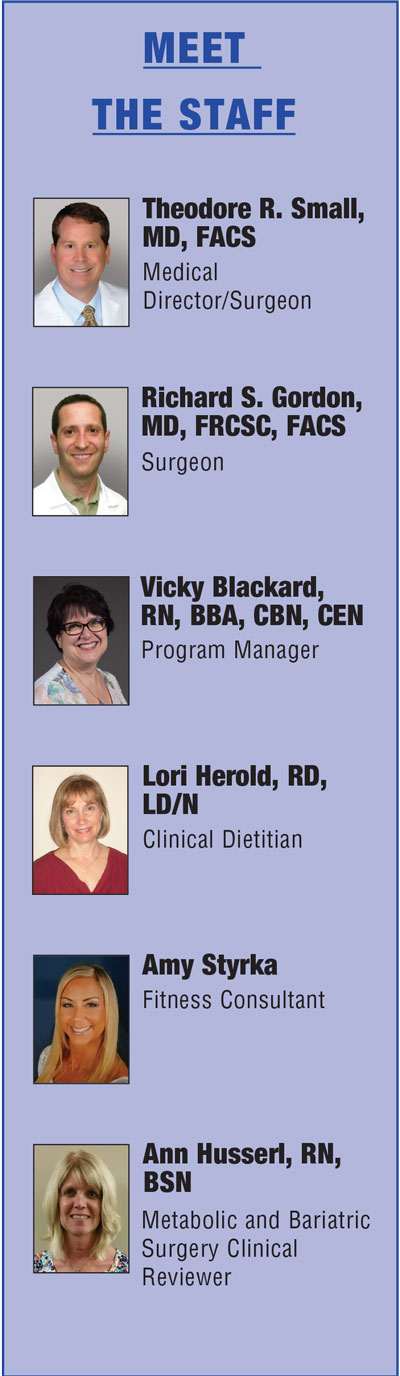
Our Staff
The bariatric program requires close collaboration among the program manager, our surgeons, and nutrition and fitness experts. We work primarily with two surgeons—Theodore Small, MD, FACS, and Richard Gordon, MD, FRCSA, FACS. Drs. Small and Gordon are credentialed through the American College of Surgeons (ACS)/American Society for Metabolic and Bariatric Surgery (ASMBS) Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). Strong support from our senior leadership has propelled the growth and reputation of our program. The bariatric program reports directly to Kelly Cullen, RN, BSN, MBA/HCM, Director of Operations.
Medical Director/Surgeon. Theodore R. Small, MD, FACS, has been with BayCare Health System since 2000 and has served as our medical director since the program started in 2006. He has also served as the president of the medical staff for Mease Dunedin and Mease Countryside hospitals. Dr. Small earned his medical degree at Medical University of South Carolina, Charleston, South Carolina, and completed his general surgery residency at Spartanburg Regional Medical Center, Spartanburg, South Carolina.
In addition to serving as our medical director, Dr. Small has been a consultant surgeon for Ethicon (Cincinnati, Ohio) and Bard Davol (Warwick, Rhode Island) for the past two decades. He also serves as course director for advanced laparoscopic surgery programs and instructs various surgeons across the country on the newest laparoscopic techniques. Dr. Small is a fellow of ACS and a member of the ASMBS, Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), and Society of Laparoscopic Surgeons. He has been in private practice with Surgical Associates of West Florida for the past 17 years.
Dr. Small served in the United States Air Force with tours at Incirlik Air Base in Turkey and Eglin Air Base in Florida. During his Air Force career, he performed and taught techniques in advanced laparoscopic surgery, particularly heartburn surgery and laparoscopic colon resections.
Surgeon. Richard S. Gordon, MD, FRCSC, FACS, started with BayCare Health System in 2005. He earned his medical degree at the University of Ottawa, Ottawa, Ontario, Canada, and completed his residency at The Ottawa Hospital, Ottawa. Dr. Gordon completed his fellowship at The Cleveland Clinic, Cleveland, Ohio, and his internship at the University of Ottawa. He is board certified in general surgery in the United States and Canada, and is fellowship trained as a weight loss and laparoscopic surgeon. He also has interest in surgery in reflux, hernias, and gallbladder disease in addition to minimally invasive colon and bowel resection. Dr. Gordon is a member of the ASMBS, SAGES, ACS, and Royal College of Surgeons of Canada. Dr. Gordon is assisted in his bariatric cases by his surgical partner Sebastian Tas, DO.

Drs. Theodore Small (left) and Richard Gordon (right) performing surgery at BayCare Mease Dunedin Hospital, Dunedin, Florida
Dr. Gordon received institutional review board (IRB) approval in April 2017 for a new procedure called single anastomosis bypass with sleeve gastrectomy. This procedure is a modification of the Biliopancreatic diversion with duodenal switch but with only one anastomosis. Weight loss is achieved both through
restriction of food consumption and malabsorption.
Program Manager. Program Manager Vicky Blackard, RN, BBA, CBN, CEN, has worked for the BayCare Health System for five years. She is a certified bariatric nurse and a certified emergency nurse. Vicky earned her degree in nursing from St. Petersburg College and graduated with honors with a bachelors in business administration from Northwood University, Midland, Michigan. She is currently pursuing her master’s degree from the University of North Carolina, Wilmington, North Carolina. Ms. Blackard is active with AMSBS as a member of the Integrated Health Support Group Committee. Her passion for the bariatric program stems from her own story as a bariatric patient. Her journey in bariatrics began by losing more than 125 pounds, and now she strives to help others through this life-changing surgery. Ms. Blackard recently wrote a workbook titled, “My Bari Pre-Surgical Workbook,” to help guide her surgery patients through the process. At this time the book has not been officially published, it is used solely for BayCare patients.
Clinical Dietitian. Lori Herold, RD, LD/N, is a registered dietitian nutritionist who has been with BayCare Health System for 19 years, working in both the inpatient and outpatient settings. Herold joined the bariatric program in 2010. She graduated from Eastern Illinois University, Charleston, Illinois, with a bachelor of science degree and completed an internship for medical science at the University of Arkansas, Little Rock, Arkansas. Ms. Herold is a member of the Academy of Nutrition and Dietetics and also of the Weight Management Practice Group. She received her Adult Weight Management Certificate and also specializes in eating disorders.
Fitness consultant. Amy Styrka has worked at BayCare in the fitness center for five years. This year Amy joined Mease Dunedin’s bariatric team as the fitness consultant. She graduated from Purdue University, West Lafayette, Indiana, with a bachelor of science degree. Ms. Styrka is an American Council on Exercise (ACE) certified personal trainer and a CrossFit level ll trainer. Metabolic and Bariatric Surgery Clinical Reviewer. Ann Husserl, RN, BSN, has been with BayCare for 34 years and joined BayCare’s quality department in 2010 as the research outcomes coordinator. From 2011 to 2014, Ms. Husserl worked primarily as a metabolic and bariatric surgery clinical reviewer (MBSCR) for an ASMBS outpatient facility. In 2014, she assumed the role as MBSCR for the Mease Dunedin bariatric program. She earned her bachelor of science degree in nursing from the University of Wisconsin-Madison, Madison, Wisconsin.
Volunteers. Many of our former patients volunteer on consultation days to help facilitate the flow between providers and patients. We have initiated a new, highly successful program called “Bari Buddies,” in which patients who are more than one year post surgery are paired with new patients for support. These volunteers call and follow up with patients as they go through the process. Recently, we started patient-led support group meetings. Patients chosen to be peer leaders are former patients who have been active with a support group and have proven to be positive, enthusiastic role models. The program manager oversees these groups. Volunteers also help in our program store.
A Unique Program
At Mease Dunedin, Ms. Blackard, program manager, also serves as the patient navigator. Each patient has full access to her throughout the process, beginning with the first meeting. She goes into surgery with the patient, serving as a liaison for the surgery staff, the surgeon, and the family. On the first day postoperative, she follows the patient through the process. She begins with the swallow study in the morning, rounds with the surgeon, and works through discharge.
The bariatric program at Mease Dunedin works to educate the patient and the hospital staff. Hospital staff must attend annual required training, along with information sessions during hospital unit staff meetings. Our patient education includes two monthly support groups, nutrition classes, vitamin clinics, and protein education. For our patients’ convenience, we have a store inside the hospital where we offer bariatric vitamins and supplements. We also carry a variety of protein drinks, snacks, and meal replacements for the different phases of the diet progression.
Timeline of Process
Patients begin the process by attending a seminar in person or online where they receive information about the types of surgeries, the surgeons and the process. Then, we verify insurance to inform the patients of what is covered and required.
After choosing a surgeon, the surgeon schedules a consult with the patient to determine what medical clearances and further testing will need to be done. After this step, the program manager receives the referral.
Next, patients meet individually with our program manager who arranges the prerequisite nutrition class and fitness education, as well as the psychologic consult. For convenience, twice a month the psychologist, fitness instructor, and registered dietitian are all in the department at the same time to meet with the patient for the required consult. If any further testing, such as a sleep study, upper gastrointestinal, or ultrasounds are ordered, we arrange them then.
For 3 to 6 months, depending on insurance requirements, patients must have monthly supervised diets. Patients may see their own physician or our registered dietitian for these appointments.
Patients receive a surgery date after all the requirements for the program, surgeon, and insurance company are met.
Patients undergo surgery on their scheduled date. Bariatric surgery patients stay on a specific floor of Mease Dunedin, where the staff is highly trained, dedicated and compassionate to our patients. During their hospital stay, we continue to re-educate the patients and their families on diet and what to expect in the days, weeks, and months ahead.
The program manager follows up on each patient one week after surgery. Patients follow up with their surgeon in both the second week and one month after surgery. The surgeon continues to follow each patient alongside the primary physician for the next year.
Patient Adherence
We try to reinforce with our patients that bariatric surgery is not a “fix all” or “quick fix,” but rather a tool. To help our patients effectively use their new tool, we offer a program called “SUCCESS.” SUCCESS is a fully customized program based on individual weight loss goals. Patients have one-on-one coaching with a registered dietitian, who helps with meal planning and offers tips on eating out. A behavioral health specialist assists with developing the tools and skill set needed for long-term lifestyle changes. Patients also meet with a fitness professional, who helps patients reach full physical activity potential. Patients usually schedule for SUCCESS at nine, 12, and 15 months postsurgery but can schedule earlier if needed. Monthly weigh-ins are offered in the department, and patients have the option to set up one-on-one appointments with the program manager for extra support as needed. Our surgeons are proactive in the success of our patients, sending them to the appropriate professional in the program. If it is noted that a patient needs extra support, they will refer to colleagues.
Conclusion
The BayCare Mease Dunedin Hospital Bariatric Program is unique and fast growing, consisting of a multidisciplinary group of providers serving a vital need for our community. For further information please visit: www.YouTransformed.org.
Category: Bariatric Center Spotlight, Past Articles