Raising the Standard: Operating Room Patient Safety Measures
 by Walter Samojeden, RN, BSN, MBA, and Dominick Gadaleta, MD, FACS, FASMBS
by Walter Samojeden, RN, BSN, MBA, and Dominick Gadaleta, MD, FACS, FASMBS
Mr. Samojeden is Assistant Director Perioperative Services, Southside Hospital, Northwell Health in Hempstead, New York. Dr. Gadaleta is Chair of the Department of Surgery at Southside Hospital and Director of Metabolic and Bariatric Surgery at North Shore University Hospital, Northwell Health in Manhasset, New York; and Associate Professor of Surgery at Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York.
Funding: No funding was provided for this article.
Disclosures: The authors reports no conflicts of interest relevant to the content of this article.
Bariatric Times. 2020;17(1):14
In May 2019, the World Health Assembly endorsed the establishment of World Patient Safety Day to be observed annually on September 17. The annual observance of this day was intended to raise global awareness about patient safety. Four of 10 patients are harmed in primary and ambulatory care settings, and 134 million adverse events occur each year in hospitals in low- and middle-income countries, contributing to 2.6 million deaths annually due to unsafe care.1
It is estimated that there is a 1 in 3 million risk of dying while travelling by airplane. In comparison, the risk of patient death occurring due to a preventable medical accident while receiving healthcare is estimated to be 1 in 300.1 In the last 30 years, aviation has had a radical cultural transformation. The transformation has been a critical shift in an industry where safety is the number one priority. Using checklists has made all the difference in this industry, and aircraft accidents have been on a steady decline since the 1980s, when checklists were developed for flight crews.2 These facts have prompted the World Health Organization (WHO) to initiate a Surgical Safety Checklist in 2008 intending to assist operating teams in addressing safety concerns and inadequate practices while increasing communication among the team members resulting in lower incidence of complications.
The WHO checklist was evaluated in a study of eight hospitals in different parts of the world; some of these hospitals provided primary care, while others provided complete (tertiary) care. The study included 3,733 patients, who were studied longitudinally and prospectively before the WHO checklist was introduced, and 3,955 patients were studied afterward. The perioperative morbidity and mortality up to the time of discharge or within 30 days of surgery were assessed with standardized questionnaires.
The introduction of the checklist was found to have the following effects, independently of the socioeconomic characteristics of the hospitals:
- A statistically significant relative reduction of mortality in major surgery by 47 percent, from 56 in 3,733 cases (1.5%) to 32 in 3,955 cases (0.8%)
- A statistically significant relative reduction of major morbidity by 36 percent, from 411 in 3,733 cases (11%) to 288 in 3,955 cases (7%)
- The WHO therefore recommended that the checklist be used in all operations and integrated into surgical training3
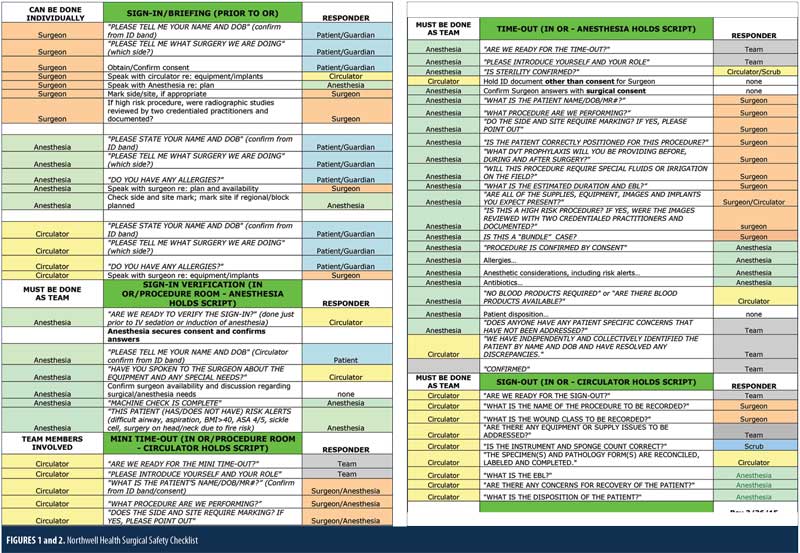
The Surgical Safety Checklist identifies three crucial phases of an operation and is performed by the operating team. The team consists of surgeons, anesthesia specialists, nurses, technicians, and other operating room personnel involved in surgery. Each safety check has been included based on clinical evidence or expert opinion that its inclusion will reduce the likelihood of serious, avoidable surgical harm and that adherence to it will likely not introduce injury or unmanageable cost.4 The Surgical Safety Checklist phases consist of a “sign in” in conjunction with patient participation when possible, “timeout” before skin incision, and the “sign out” before the patient leaves the operating room. The “sign in” consists of identity, procedure, and laterality confirmation, as well as any necessary surgical site markings and signed consents. The “time out” is performed just prior to skin incision, where a “pause” usually is initiated by the circulating nurse. During this pause, each team member identifies themselves and their role, two forms of patient identification are confirmed, and procedure verification, laterality, patient allergies, and any other pertinent information, including prophylactic antibiotics that have been administered are verified. During this phase, all necessary equipment and implants are identified and confirmed to be available. The “sign out” phase occurs before the surgeon and patient leave the operating room. This phase ensures the proper procedure is recorded, specimens are reconciled, and estimated blood loss and patient disposition are confirmed. By following these crucial checks, the operating room personnel can minimize the most common and avoidable risks endangering the lives and well-being of surgical patients.
While the checklist is used as a tool to enhance patient safety, other factors, such as early education and training of staff, multidisciplinary involvement, and ongoing feedback identifying areas of improvement are needed for successful outcomes in patient safety.
Institutions have implemented remote video auditing (RVA) while maintaining patient integrity with visual cues ensuring the proper time is spent during each phase of the checklist process. Northwell Health began RVA in the operating room at its Forest Hills location in March 2013, while Southside Hospital implemented RVA in February 2017. The RVA service was provided through a disinterested third party. Arrowsite’s RVA services provide direct observation in the hospital setting and help providers raise their adherence to hospital protocols resulting in a safer environment for their patients. RVA in the healthcare industry increases patient safety, reduces infection rates, and improves operating room turnover times. Review of an extensive range of criteria helps providers adhere to their hospital’s protocols. Near real-time video auditing provides prompt feedback and relevant metrics to increase use in operating rooms.5 These criteria are initiated by the circulating nurse and include a “colored cue card,” which contains the list of checks necessary during each phase of the safety check process.
RVAs are used for ongoing feedback in real time and monthly for review by senior leadership. Through real-time feedback loops via RVA, management can immediately question the operating team as to why there was “fallout.” Fallouts consist of abbreviated times for a specific phase indicating the complete checklist was not completed. Fallouts also consist of no visual cues observed at all, indicating a phase might have been omitted. These fallouts can be reviewed, and the surgical team can be debriefed to reinforce and identify areas of opportunity. Monthly meetings with key leadership review all phases of the surgical safety checklist. Areas of exceptional performance are highlighted as well as areas for opportunity. Southside Hospital moved its compliance on timeouts from 93.2 percent in 2017 to 98.6 percent in 2019.
These high-level meetings allow leadership to question why certain rooms are consistently underperforming. Camera positioning, blind spots, or human error can be potential areas of fallout. Continued education with feedback on performance, and heightened awareness as to each room’s blind spots combined with multidisciplinary involvement will ensure proper safety standards are met.
References
- Patient Safety. World Health Organization. https://www.who.int/patientsafety/en/. Accessed January 3, 2020.
- Clarke T. Lessons we can learn from aviation checklists. Safety Culture. https://blog.safetyculture.com/checklist-best-practices/lessons-we-can-learn-from-aviation-checklists. Accessed January 3, 2020.
- Fudickar A, Horle K, Wiltfang J, Bien B. The effect of the WHO Surgical Safety Checklist on complication rate and communication. Dtsch Arztebl Int. 2012;109(42):695–701.
- Implementation Manual Surgical Safety Checklist. https://www.who.int/patientsafety/safesurgery/tools_resources/SSSL_Manual_finalJun08.pdf. Accessed January 3, 2020.
- Healthcare Solutions. https://www.arrowsite.com/healthcare. Accessed January 3, 2020.
Category: Past Articles, Raising the Standard



