Impact of a Postoperative Bariatric Surgery Phone Call Quality Improvement Intervention on 30-day Hospital Readmissions and Emergency Department Visits

by Melissa C. Majumdar, MS, RD, CSOWM, LDN; Zachary I. Grunewald, PhD, MS, RDN, LD; Elissa A. Falconer, MD; Maggie L. Diller, MD; Mobola Oyefule, MD; Federico J. Serrot, MD; Jamil L. Stetler, MD; Ankit D. Patel, MD; Jahnavi K. Srinivasan, MD; S. Scott Davis Jr., MD; Edward Lin, DO; and Elizabeth M. Hechenbleikner, MD
Ms. Majumdar and Dr. Grunewald are with Emory Healthcare, Office Quality and Risk in Atlanta, Georgia. Ms. Majumdar is with Emory University Hospital Midtown in Atlanta, Georgia. Dr. Grunewald is with Emory Johns Creek Hospital in Johns Creek, Georgia. Drs. Falconer, Diller, Oyefule, Serrot, Stetler, Patel, Srinivasan, Davis Jr., Lin, and Hechenbleikner are with the Department of Surgery, Division of General and Gastrointestinal Surgery, Emory University School of Medicine in Atlanta, Georgia.
Funding: No funding was provided for this article.
Disclosures: The authors have no conflicts of interest relevant to this article.
Bariatric Times. 2023;20(2):10–15.
Abstract
Objective: Outpatient care coordination phone calls can improve postoperative outcomes in certain surgical specialties but are not well described in metabolic and bariatric surgery (MBS). This quality improvement (QI) initiative evaluated a standardized postoperative MBS phone call intervention on 30-day emergency department (ED) visits and hospital readmissions.
Design: A phone call was conducted following MBS to inquire into patients’ postoperative recovery and wellbeing. Retrospective chart review was done pre- (1/2019–3/2020) and postintervention (5/2020–6/2021) for variables and outcomes. Two-sample t-tests were used; p-values less than 0.05 were statistically significant.
Setting: 532-bed mixed community and academic hospital.
Participants: Patients aged 18 years or older undergoing primary or revisional MBS.
Measurements: Patient and operative characteristics, monthly ED visit and readmission rates, postoperative day of presentation, and underlying reasons for ED visits and readmissions.
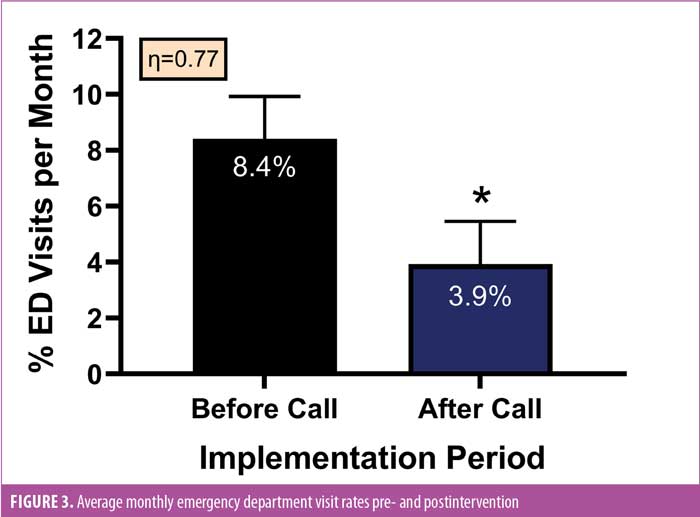
Results: Overall, 522 patients were identified (263 preintervention, 259 postintervention) with 32 (6.1%) ED visits (20 preintervention, 12 postintervention) and 23 (4.4%) readmissions (9 preintervention, 14 postintervention). The top three reasons for ED visits were oral intake problems, constipation, and wound problems. The top three reasons for readmissions included surgical complications or issues, oral intake problems, and venous thromboembolism events. Average monthly ED visit rates decreased by 54 percent, from 8.4 to 3.9 percent (pre- and postintervention, respectively), while average monthly readmission rates increased from 3.1 to 3.9 percent (pre- and postintervention, respectively).
Conclusion: Standardized MBS phone calls are a promising postoperative care coordination adjunct and might help reduce ED visits. Further QI work will include improving postoperative education, identifying higher risk patients before discharge, and larger scale data collection efforts.
Keywords: Emergency department utilization, metabolic and bariatric surgery quality improvement, sleeve gastrectomy, gastric bypass, outcomes
The demand for metabolic and bariatric surgery (MBS) continues to rise, matching the ongoing surge in the national and global obesity epidemic. While MBS is arguably the cornerstone for sustainable weight loss, with an excellent safety profile, postoperative emergency department (ED) visits and hospital readmissions are common and potentially preventable. ED visits occur in 10 to 12 percent of MBS patients, with early readmissions ranging from 0.6 to 11.3 percent.1,2 Based on December 2019 Metabolic and Bariatric Surgery Quality Improvement Program (MBSAQIP) data, national 30-day readmission rates were 4.5 percent.3 The most common reasons for readmissions and ED visits included abdominal pain, nausea, vomiting, dehydration, and wound-related issues.4,5 Notably, Petrick et al6 estimated potentially preventable readmissions after MBS are as high as 48 percent.
Hospitals are evaluated on postoperative outcomes, such as ED visits and readmission rates, which affect MBSAQIP national benchmarks, as well as patient satisfaction and quality of care. These unplanned healthcare visits can be impacted by inadequate communication between MBS patients and clinical care teams after their index surgery. Furthermore, outpatient care coordination phone calls have been shown to improve outcomes across several surgical specialties; however, postoperative phone call interventions remain poorly described among MBS patients.7 Of note, the MBSAQIP quality improvement (QI) initiative, Decreasing Readmissions through Opportunities Provided (DROP), successfully reduced all-cause 30 day-readmissions by implementing a variety of bundled perioperative interventions, including discharge planning education, use of same-day appointments for clinical concerns, and implementing registered nurse phone calls the day after hospital discharge.8 Although impactful, not all bariatric centers have the ability to deploy large programs like DROP; thus, having scalable resources for designing and implementing interventions, such as outpatient care coordination phone calls, following MBS could be very beneficial.
Therefore, the aim of this study was to reduce 30-day hospital readmissions and ED visits by 25 percent after the implementation of a standardized outpatient phone call QI initiative for MBS patients at a single-site 532-bed hospital.
Methods
Hospital setting. Emory University Hospital Midtown is an urban MBSAQIP-accredited center in Atlanta, Georgia. It is a 532-bed mixed community and academic institution designated as a comprehensive center with adolescent and obesity medicine designations.
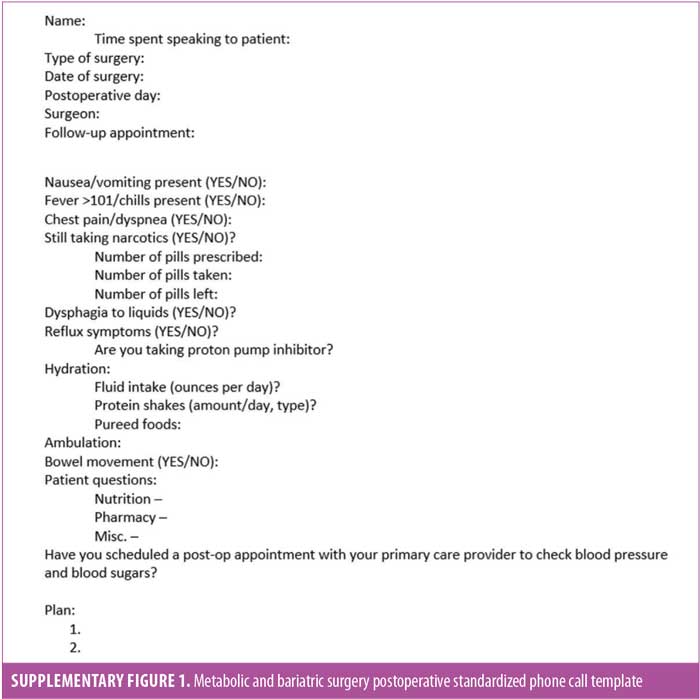
Postoperative phone call intervention. A standardized outpatient phone call template with 10 questions surrounding common postoperative issues was employed by the institutional MBS coordinator or physician assistants specializing in obesity medicine. If clinically indicated, a patient care escalation pathway with targeted interventions was utilized. The phone call template and clinical escalation pathway were evaluated and approved by a multidisciplinary team of clinicians, including nursing staff, obesity medicine specialists, surgeons, and registered dietitian nutritionists. Additional ad hoc feedback was garnered through the hospital’s Patient Family Advisory group for targeted education and medication interventions.
Phone call implementation and data collection. The postoperative phone call was originally initiated on postoperative day (POD) 2 to 3 beginning in May 2020; this day was selected based on postdischarge phone call timing recommendations from the Agency for Healthcare Research and Quality’s (AHRQ) Re-Engineered Discharge (RED) toolkit.9 Initial trends were observed in ED visits and diet progression challenges over a three-month pilot period, which showed the majority of MBS patients presented to the ED within the first week of surgery, while hospital readmissions were typically noted two weeks postoperatively. Of note, challenges with drinking and eating following MBS are common in the early postoperative days and therefore difficult to identify a frank medical concern when phone calls were employed on POD 2 to 3. Based on these initial findings, the postoperative call was shifted to POD 6 to 7 starting in August 2020. This better aligned with diet progression issues and aimed to counteract preventable problems related to dehydration and constipation via appropriate clinical escalation.
Following implementation of the phone call intervention, patient charts were retrospectively reviewed for patients aged 18 years or older who underwent primary or revisional MBS before (January 2019–March 2020) and after implementing (May 2020–June 2021) the phone call intervention (Supplementary Figure 1) and escalation pathway. Due to the COVID-19 pandemic, there were no elective surgeries in April 2020, and thus this month was excluded from data analysis. All patients underwent appropriate preoperative multidisciplinary evaluation and counseling in preparation for MBS and met standard American Society for Metabolic and Bariatric Surgery (ASMBS) and National Institutes of Health (NIH) guidelines.
All data were abstracted from the electronic medical record (EMR) and/or MBSAQIP institutional database. Patient characteristics recorded were as follows: age, sex, and body mass index (BMI). Perioperative details included surgery type (primary sleeve gastrectomy [SG], primary Roux-en-Y gastric bypass [RYGB], revision or conversion surgery), case volumes, and length of stay following index procedure. Patients who underwent adjustable gastric band placement or removal were excluded from data collection.
Outcome measures collected were as follows: 1) overall and monthly 30-day ED visit and hospital readmission rates, 2) postoperative day of presentation, and 3) underlying reasons for ED visits and readmissions. Pertinent phone call measures collected for operational purposes included the following: 1) number of attempted calls, 2) number of phone calls completed, 3) POD of phone call attempt, 4) patient phone call or message occurrences prior to ED visit or readmission, and 5) phone call duration.
Statistical analysis. Run charts were used to demonstrate monthly ED visit and hospital readmission rates. A Pareto chart was created to visualize trends in underlying reasons for ED visits and readmissions. Descriptive statistics and two-tail t-tests were used for comparison of pre- and postintervention variables and outcomes. An effect size (Cohen’s d) was calculated to further reveal the impact of the postoperative call intervention on ED visits. GraphPad Prism (version 9.0, GraphPad Prism Software; La Jolla, CA) was used for statistical analysis, with significance determined at a p-value less than 0.05. All averaged data are presented as means ± standard error of the mean (SEM).
This study was exempt by the Institutional Review Board (IRB) because it was deemed nonhuman subjects research as a local QI initiative. All procedures were conducted in accordance with the institution’s committee on ethical standards.
Results
Patient and surgical characteristics. A total of 522 patients were identified for study inclusion, with 263 identified before the standardized phone call intervention and 259 identified postintervention. Overall, 85 percent of patients were female, with an average age of 44.0±0.51 years and an average BMI of 46.0±0.35kg/m2. Operative index case volumes were 68.6 percent SG, 26.1 percent RYGB, and 5.4 percent revision/conversion procedures. While similar patient characteristics were noted during the study period, only 1.9 percent of revision/conversion cases were completed, preintervention compared to 8.9 percent postintervention (Table 1). Length of stay after MBS was typically 1 to 2 days, with an initial office visit within 30 days of the index procedure. A total of 201 patients (78%) successfully received the standardized phone call during the call intervention period. The MBS coordinator performed 95 percent of the phone calls, while the obesity medicine specialists completed five percent of calls. The average timeframe following index operation for call completion was 5.9±0.12 days. Of the patients who presented to the ED or were readmitted, 20 patients (36%) called or sent an EMR message prior to ED visit or readmission. Total time to complete the phone call ranged from 8 to 30 minutes.
Hospital readmissions. Overall, 23 hospital readmissions (4.4%) occurred during the data collection period, nine (3.4%) during preintervention and 14 (5.4%) during postintervention. The average monthly readmission rate increased from 3.1±1.2 percent preintervention to 3.9±1.7 percent postintervention (data not shown). The average day of presentation for a 30-day readmission preintervention was POD 16 and POD 13 postintervention. The top reasons for readmissions were technical or surgical problems, difficulty with oral intake (i.e., nausea or vomiting), and venous thromboembolism events (Figure 1). The index procedures for readmitted patients were as follows: SG (n=13, 57%), RYGB (n= 8, 35%), and revisional cases (n=2, 9%). Upon further chart review, 19 readmissions (83%) were deemed related to the index operation, eight preintervention (89%) and 11 postintervention (79%), and only seven readmissions (30.4%) overall were deemed potentially preventable (2 preintervention, 5 postintervention). In addition, five patients required a reoperation, either due to a technical problem related to the index procedure (n=4) or an unrelated surgical issue (n=1). Reoperations included an open cholecystectomy for acute cholecystitis (n=1), diagnostic laparoscopy for abdominal fluid collection (n=1), exploratory laparotomy with small bowel resection and anastomosis for bowel obstruction (n=1), and diagnostic laparoscopy with enteroenterostomy for bowel obstruction (n=2). The increase in hospital readmissions noted in the postintervention group was random in relationship to the study time frame and, more importantly, the underlying clinical conditions required inpatient management, regardless of implementing the standardized phone call intervention. Upon further review of readmission cases, there appeared to be an increase in rates in the postintervention group for patients who underwent RYGB (n=2 [2/9, 22%] preintervention vs. and n=6 [6/14, 43%] postintervention) and revisional cases (n=0 preintervention vs. n=2 [2/14, 14%] postintervention) (data not shown).
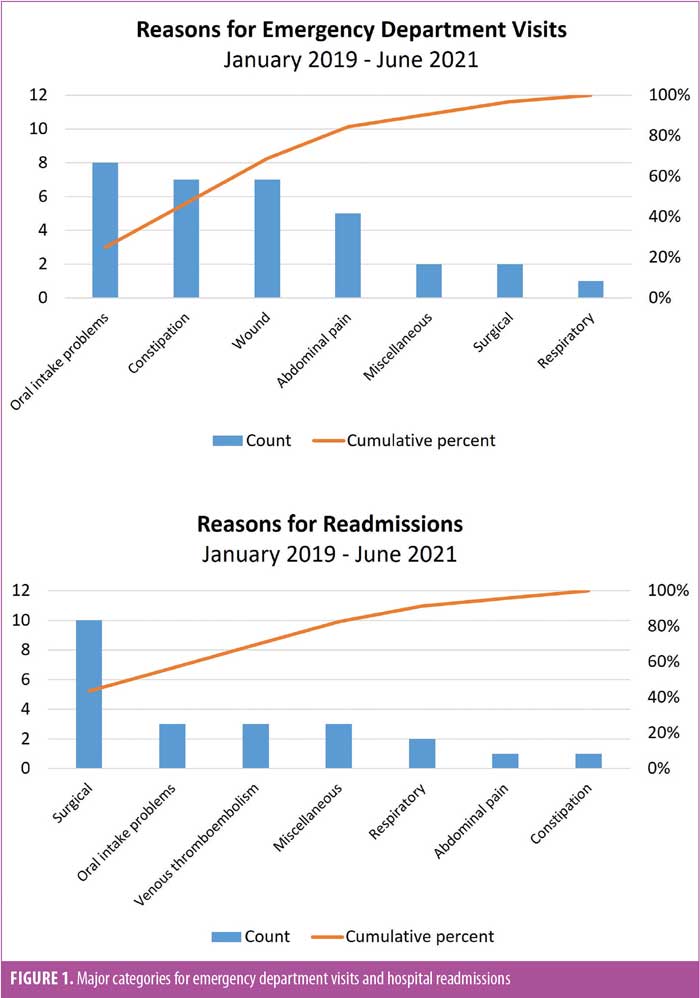
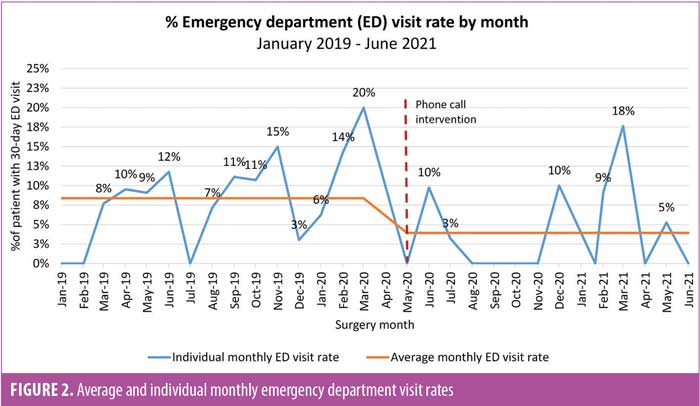
Hospital ED visits. A total of 32 ED visits (6.1%) occurred during the data collection period, 20 (7.6%) during preintervention and 12 (4.6%) postintervention. There were no ED visits for eight of the 14 months postintervention, compared to only three of the 15 months preintervention (Figure 2). The average monthly ED visit rate dropped by 54 percent, from 8.4±1.5 percent preintervention to 3.9±1.5 percent postintervention (p=0.05; effect size Cohen’s d [η]=0.77) (Figure 3). The average day of presentation for an ED visit was POD 11 and was not affected by the phone call intervention. The top reasons for ED visits were difficulty with oral intake, constipation, wound problems, and abdominal pain (Figure 1). The index procedures for ED visit patients were as follows: SG (n=20, 62.5%) and RYGB (n=12, 37.5%). Upon further chart review, 29 visits (91%) were deemed related to the index operation, 18 (90%) preintervention and 11 (92%) postintervention. A total of 23 ED visits (71.9%) were deemed potentially preventable, 13 in the preintervention period and 10 in the postintervention period.
Discussion
Findings from this QI initiative suggested that a postoperative phone call intervention might help reduce the number of patients presenting to the ED following MBS but did not decrease hospital readmissions. We found that implementation of a standardized postoperative call intervention was associated with a 54 percent reduction in average monthly ED visits with a moderate-to-robust effect size, surpassing our initial goal of a 25 percent reduction. This is likely due to the fact that many ED visits were potentially preventable for frequent issues, such as dehydration and constipation, where early intervention and communication prevented worsening of a patient’s clinical condition. In contrast, for hospital readmissions the most common underlying reason was a surgical or technical issue either related to the index procedure itself and/or was unavoidable altogether.
As a result of the MBS phone call intervention and clinical escalation pathway, multiple interventions were developed for the inpatient and outpatient setting. For example, an outpatient preventive bowel regimen was developed and started on POD 2 to help decrease constipation-related ED visits. This was followed by formal inpatient discharge education led by the MBS coordinator and nursing staff involving a handout and teach-back patient worksheet to ensure appropriate comprehension of verbal instructions provided for medications to treat constipation, pain, nausea, and heartburn. In addition, an outpatient intravenous fluid (IVF) infusion pathway was created to address issues with postoperative dehydration, facilitating more efficient resolution of clinical issues and avoiding ED visits for some patients. This clinical pathway included purchasing of supplies, staff training, and creation of a standard ordering process to administer IVFs as needed in the outpatient MBS clinic. Alternatively, if clinic staff cannot accommodate IVF requests, patients are scheduled for infusions in an outpatient center located in close proximity to the office. In their 2018 study, Petrick et al6 identified outpatient services targeting oral intake problems (i.e., giving providers electronic access to infusion centers) as a key opportunity for mitigating potentially preventable readmissions. Moreover, the phone call intervention identified additional gaps related to care coordination, including challenges with prescription acquisition prior to discharge, which prompted adding pertinent questions to the call template, tracking medication errors, and creating interventions to improve medication discharge processes.
Postoperative phone calls following MBS are appealing for many reasons, including standardization of care transitions, improvement in the quality of care delivered, and identification of barriers to health and comprehension. A 2016 study among outpatient endocrine surgery patients demonstrated that four percent of ED visits were avoided by nursing staff simply addressing patient concerns and providing reassurance over the phone.10 To that end, any opportunity to improve communication and patient engagement as issues arise during postoperative recovery, regardless of the surgical specialty, can have a major impact on care. The success of our phone call intervention was multifactorial; in addition to improved communication, multiple interventions happened simultaneously, creating a “bundled” phenomenon for improving patient care, with detailed discharge education sheets for common postoperative problems, standard prescription orders prior to discharge, inpatient MBS coordinator rounding to increased patient education, and an outpatient constipation prevention regimen. More importantly, implementation of a standardized phone call helped us identify common issues, questions, and challenges earlier in the postoperative phase, and as such, structured interventions were more likely to elicit a positive impact on patient outcomes.
While the postoperative call intervention was largely positive for patients and providers, this intervention was not without barriers. While the MBS coordinator was able to complete 95 percent of the phone calls to maintain consistency, patient follow-up was still difficult at times, which led to a completion rate of only 78 percent; thus, the impact on ED visits could have been greater. Of note, each MBS patient has an individualized experience, and some aspects of postoperative care have to be tailored to meet these individual needs, which the phone call intervention was not designed to do. The targeted inpatient discharge teaching and postoperative phone call were also time consuming, with an estimated duration of 30 minutes and 15 minutes per patient, respectively, assuming no clinical or administrative escalation was required. In addition, some patients viewed the call as burdensome and required careful and thorough reiteration of patient escalation pathways, as the MBS coordinator’s phone number was not intended for clinical support outside of the phone call intervention.
Compared to the controlled design of research studies, QI initiatives have an adaptive, iterative process with the benefit of rapidly adopting findings into local care delivery.11 Keeping a pulse on appropriate clinical progression and outcomes following MBS with the use of QI techniques and tools helps improve processes through quantitative (e.g., run charts) and qualitative structures (e.g., Pareto charts). As processes improve through interventions, such as standardized phone calls, discharge education sheets, and other clinical care pathways, the ultimate goal is to have a positive impact on patient outcomes, such as decreasing 30-day ED visits, as was shown in this study.
Limitations. The results of this standardized outpatient phone call QI intervention have to be interpreted with caution, given that this was not a study controlling for patient-, operative-, surgeon- or hospital-level factors. Providers used clinical judgment rather than established criteria for determining potentially preventable ED visits and readmissions. While MBS patients all received a similar enhanced recovery inpatient care pathway, there was still room for individualized care within this protocol, based on surgeon preference. In addition, this was a single-institution retrospective study with a relatively small number of patients
Conclusion
In conclusion, implementation of a structured postoperative phone call and clinical escalation pathway might help to reduce ED visits following MBS. Future QI work and research among MBS patients should focus on deploying more mobile health interventions, improving perioperative education, identifying higher risk patients before discharge following index operation, and conducting larger scale data collection efforts.
References
- Khouri A, Alvarez R, Matusko N, Varban O. Characterizing the preventable emergency department visit after bariatric surgery. Surg Obes Relat Dis. 2020;16(1):48–55.
- Berger ER, Huffman KM, Fraker T, et al. Prevalence and risk factors for bariatric surgery readmissions: findings from 130,007 admissions in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program. Ann Surg. 2018;267(1):122–131.
- Landin MD, Gordee A, Lerebours RC, et al. Trends in risk factors for readmission after bariatric surgery 2015-2018. Surg Obes Relat Dis. 2022;18(5):581–593.
- Macht R, George J, Ameli O, et al. Factors associated with bariatric postoperative emergency department visits. Surg Obes Relat Dis. 2016;12(10):1826–1831.
- Chen J, Mackenzie J, Zhai Y, et al. Preventing returns to the emergency department following bariatric surgery. Obes Surg. 2017;27(8):1986–1992.
- Petrick AT, Brindle SA, Vogels E, et al. The readmission contradiction: toward clarifying common misconceptions about bariatric readmissions and quality improvement. Surg Obes Relat Dis. 2018;14(7):1026–1032.
- Harrison PL, Hara PA, Pope JE, et al. The impact of postdischarge telephonic follow-up on hospital readmissions. Popul Health Manag. 2011;14(1):27–32.
- Petrick AT, Gadaleta D. Raising the standard: DROP—the first national MBSAQIP quality improvement project: decreasing readmissions through opportunities provided. Bariatr Times. 2019;16(2):16.
- Agency for Healthcare Research and Quality. Tool 5: how to conduct a postdischarge followup phone call. https://www.ahrq.gov/patient-safety/settings/hospital/red/toolkit/redtool5.html. Accessed 25 Feb 2022.
- Brekke A, Elfenbein DM, Madkhali T, et al. When patients call their surgeon’s office: an opportunity to improve the quality of surgical care and prevent readmissions. Am J Surg. 2016;211(3):599–604.
- Children’s Hospital of Philadelphia Institutional Review Board. Quality improvement vs research. https://irb.research.chop.edu/quality-improvement-vs-research. Accessed 10 Feb 2022.
Category: Original Research, Past Articles




