Welcome to R&R Surgical Institute—Torrance, California

by Ramin Roohipour, MD; Jillian Angelo Caccamo, MS, MD; and Qemal Shaholli
Dr. Roohipour is Chief Executive Officer and Medical Director, R&R Surgical Institute in Torrance, California. Dr. Angelo Caccamo is with R&R Surgical Institute in Torrance, California. Mr. Shaholi is Chief Operating Officer, R&R Surgical Institute in Torrance, California.
Funding: No funding was provided.
Disclosures: The authors report no conflicts of interest relevant to the content of this article.
Bariatric Times. 2023;20(7–12):30–32.
R&R Surgical Institute stands as one of the most exceptional and bustling bariatric ambulatory surgery centers in California. As a standalone center, R&R proudly holds accreditations from the Centers for Medicare & Medicaid Services (CMS), Metabolic and Bariatric Surgery Accreditation and Quality Program (MBSAQIP), and Blue Distinction Center (BDC). Established in 2018 with a steadfast commitment to providing top-tier care to each patient in an opulent outpatient environment, the center has not only upheld this promise, but also flourished without any concessions.
Our Staff
We have a Chief Operating Officer (COO) who efficiently manages all business affairs. We also have dedicated bariatric surgeons, lead surgical and nursing staff, and preoperative and operating room (OR) nurses. Additional support staff handle registrations and other ancillary responsibilities. Moreover, we have clinical nurses who ensure our MBSAQIP and BDC data remain up-to-date.
We are proud to be an in-network facility, providing high-quality, cost-effective care to our patients. Notably, we are recognized for handling complex revisional surgeries, drawing patients from as far as Alaska and the East Coast.

Our Facility and Procedures
We have two separate teams for scheduling, one for the practice and another for the surgery center. Although they are independent entities, their proximity on the same floor in the same building facilitates seamless communication. This hands-on collaboration ensures no detail is overlooked.
In our waiting room, we have created a private and comfortable environment. We are situated in a prestigious, multistory building in the South Bay area of Los Angeles. Patients receive personalized guidance from our lead nurse from the moment they schedule their surgery. Preoperative workups are meticulously ensured. We have even arranged for a concierge pharmacy to deliver postoperative medications to the facility, sparing patients a trip to the pharmacy.
In the patient rooms, we have gone above and beyond to provide a tranquil experience. Each room features specialized bariatric bed recliners for family members who might stay overnight. We also provide secure closets for belongings and in-room entertainment options.
As for the OR, we have invested in cutting-edge technology. Our four integrated ORs are equipped with top-tier monitors and laparoscopic tools, enabling us to perform even the most complex procedures. Additionally, we have the capability to use fluoroscopy and live imaging from computed tomography (CT) scans or magnetic resonance imagings (MRIs) when necessary. We utilize tristapler devices, which are commonly used in the market. Additionally, we employ an ultrasonic energy device called Ligasure (Medtronic; Minneapolis, MN), which helps ensure relatively bloodless surgeries.
Our team of 11 dedicated anesthesiologists specialize in bariatric surgery. We also have established a dedicated endoscopy suite for both diagnostic and interventional procedures, which includes the ability to conduct intraoperative endoscopy if needed. We are equipped to handle cases up to 600lbs, though our outpatient facility’s cutoff is set at 600lbs.
Following surgery, patients receive postoperative care in the same preoperative area, ensuring a seamless transition to recovery. Each patient is assigned a dedicated nurse and nurse assistant throughout their 23-hour stay to diligently attend to their needs, including early ambulation postsurgery. The next day, they leave with a wireless, rechargeable sequential compression device to prevent blood clots in their legs. This allows them to walk around and even drive within the first two weeks after surgery.
Additionally, we provide a reliable intravenous (IV) line for at-home IV fluid administration for 5 to 7 days postoperatively. This proactive approach has resulted in a readmission rate of zero for dehydration or minor pain, which is highly beneficial for both patients and insurance companies.
We perform gastric bypass and revisional cases in a separate facility, allowing for the flexibility to meet the unique needs of our patients while adhering to the strict regulations of a bariatric center of excellence.
Bariatric Patient Assessment and Care
We adhere to the guidelines set by the National Institutes of Health (NIH), American College of Surgeons (ACS), and MBSAQIP. However, it is important to note that insurance guidelines often come into play, which can sometimes be more stringent. We work through the layers of appeal and peer review with payors to ensure patients can use their coverage benefits. In many practices, a significant portion of patients might drop out due to frustration with the insurance process. However, in our practice, we take on the responsibility of dealing with insurance companies on behalf of the patient. We prepare a tailored cover letter detailing the patient’s qualifications and necessary workups, and we put the insurance company on notice. Our team diligently follows up, often every 48 hours, to ensure a smooth process. For patients interested in paying out of pocket, as long as they meet the minimum criteria, we offer them surgery.
Initial consultations provide a good assessment from a guideline standpoint, but our back office conducts thorough insurance verification. There are more interactions with patients during endoscopy, follow-up visits, and other engagements to ensure they are committed and compliant. Additionally, they undergo a psychiatric evaluation to ensure they have a good understanding of the program and are mentally prepared.
On average, we handle between 450 to 550 bariatric cases annually. In 2020, due to the impact of COVID-19, the numbers were lower, but in 2021, our cases numbered closer to 400. For 2022, we saw an increase, approaching 500 cases. This year, we are on track for an 18- to 20-percent growth in the third quarter.
For primary procedures, such as sleeve gastrectomy, the majority of patients are within a 120-mile radius of our location. However, 5 to 10 percent of our patients travel from other states for these primary procedures.
Long-term Adherence
In the first year postsurgery, patients have follow-up visits at one week, four weeks, three months, six months, and one year. After that, it transitions to annual visits, but we encourage ongoing communication. We provide access to Health Insurance Portability and Accountability Act (HIPAA)-compliant chat platforms where patients can connect with our team members 24/7; this includes nurse practitioners, physician assistants, facility nurses, and administrators, with all clinical matters directed to me.
The majority of our patients are proactive in seeking support. Our follow-up rates remain above 80 percent even beyond the first year.
MBSAQIP-certified Center
MBSAQIP certification is a rigorous process that goes beyond a mere rubber stamp. Facilities must meet specific benchmarks and demonstrate positive outcomes to receive this certification. Fortunately, when we started in 2018, we had a substantial volume of cases, with an impeccable record of zero mortality, zero hospital transfers, and only minor complications. Patients are becoming increasingly savvy about their healthcare choices. They often inquire about board certification, experience, and outcomes, which speaks to our patient-centered approach.
Patient and Staff Safety
We have implemented several measures to ensure both physical and patient safety. All entrances and exits require secure access codes. We have three indoor egress exits in case of emergencies. Our doors are 120-minutes fireproof, and we have an outdoor terrace and balcony on the fourth floor for additional egress options. In the event of a power outage, we have an electric generator that can provide power for up to 120 minutes if all four ORs are running.
We conduct routine safety training sessions for our staff, covering areas such as cyber and physical safety. In terms of patient safety, we have transfer agreements with local hospitals, allowing for efficient and prompt care if needed. Additionally, we conduct emergency drills to ensure preparedness in unforeseen situations.
Staff Training
We provide specialized, bariatric-oriented training based on each staff member’s role within the practice and surgery center. Sensitivity training around bariatric surgery is offered to all members of our workforce, regardless of their position.
A High-quality Practice
Our uniqueness lies in being one of the very few outpatient facilities solely dedicated to bariatrics. We take pride in providing high-quality care while ensuring patient safety and satisfaction. Our record speaks for itself, and we have garnered recognition from major payors for our commitment to excellence.
Beyond the tangible infrastructure and accreditation, it is the qualitative aspects that truly set us apart. Our team is deeply committed to supporting individuals on their transformative journey toward a healthier life. We see this as a lifelong partnership, not just a transaction, and believe in the lasting impact we have on our patients’ lives.
We had a new colleague and partner, Dr. Jillian Angelo, join us in 2022. She completed her general surgery training at Harbor University of California, Los Angeles (UCLA) and bariatric surgery fellowship at Brigham and Women’s Medical Center (Harvard University). Dr. Angelo is an outstanding surgeon and a great addition to our team and prepared the clinical vignette below.
Clinical Vignette
A 61-year-old female patient with a history of bariatric surgery presented to our clinic for a chief complaint of heartburn and regurgitation. She reported she had an open Roux-en-Y gastric bypass (RYGB) in 1994, at which time her weight was 235lbs, for a body mass index (BMI) of 37kg/m2. Her nadir after index surgery was 170lbs (BMI: 26kg/m2). At the time of presentation, she weighed 214lbs (BMI: 33kg/m2). She endorsed daily heartburn unresponsive to maximal medical management. She also endorsed lack of restriction without adequate satiety. Additional comorbidities included hypertension, high cholesterol, and depression. Records could not be obtained, as the patient did not remember any details regarding her surgery.
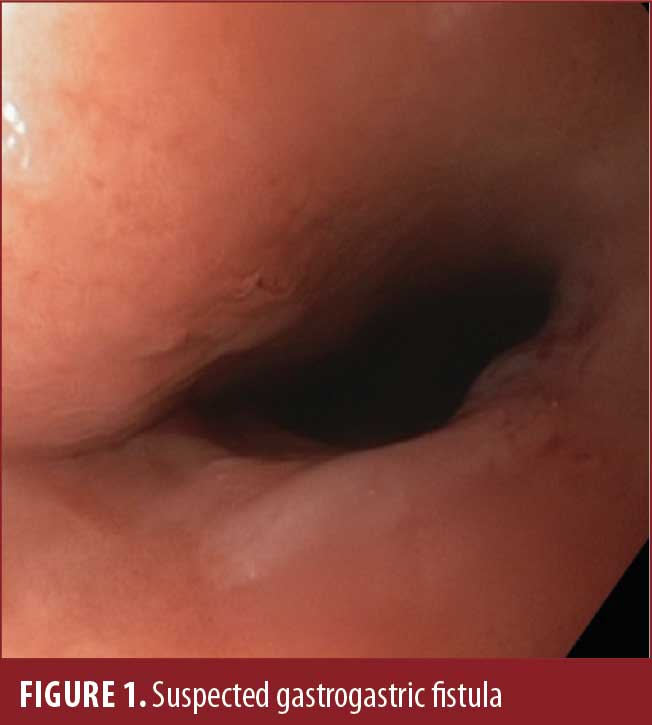
Upper endoscopy was performed and showed a 3cm hiatal hernia with moderate distal erosive esophagitis, a large gastric pouch, and a presumed large gastrogastric fistula (Figure 1). The suspected gastrojejunostomy (GJ) (Figure 2) was located posteriorly, with exposed silk suture noted, and was collapsed and unable to be intubated. Upper gastrointestinal (GI) series showed a large fistula between the fundus and the body of the stomach without evidence of patent GJ (Figure 3).


The patient was offered an operative revision of RYGB with hiatal hernia repair and taken to the operating room. A diagnostic laparoscopy was performed and found a large, intact stomach (Figure 4) with a Silastic ring around the superior aspect of the lesser curvature, with extensive scarring precluding safe dissection (Figure 5).
Discussion
The vertical band gastroplasty was a weight loss surgery popularized in the 1980 to 1990s that functioned primarily through restriction. It involved creating a pouch from the lesser curvature using a small Silastic ring for the outflow of the food. A noncutting TA stapler was likely used to divide this pouch from the fundus, funneling food through the lumen with the ring around it. The procedure was largely abandoned because it provided inadequate weight loss with a high complication rate.1
The entrance through the Silastic ring was what had been assumed to be the obliterated GJ at the time of endoscopy. The original TA staplers were noncutting, and the lumen can become patent with time. In our patient, this area was likely what we had assumed to be the gastrogastric fistula.
There are three major learning points from this case. It is particularly important when performing revisional surgery to be aware of the now largely abandoned surgical techniques that were not unpopular in the 1990s to 2000s, such as the vertical band gastroplasty or gastric bypass with Fobi ring.2 Obtaining prior operative reports can add substantial information. Finally, if the anatomy is not straightforward, have a low threshold to discuss alternative scenarios with your radiology team when reviewing imaging for preoperative planning.
References
- Balsiger BM, Poggio JL, Mai J, et al. Ten and more years after vertical banded gastroplasty as primary operation for morbid obesity. J Gastrointest Surg. 2000;4(6):598–605.
- Bessler M, Daud A, Kim T, DiGiorgi M. Prospective randomized trial of banded versus non-banded gastric bypass for the super obese: early results. Surg Obes Relat Dis. 2007;3(4):480–484; discussion 484–485.
Category: Bariatric Center Spotlight, Current Issue




