Analysis of Bariatric Surgery Outcomes in the Geriatric Population at a Rural Teaching Hospital

by Kristin McCoy, MD; Michael Nussbaum, MD, FACS; and Arnold Salzberg, MD, FACS, FASMBS
Drs. McCoy, Nussbaum, and Salzberg are with Carilion Roanoke Memorial Hospital in Roanoke, Virginia.
Funding: No funding was provided for this article.
Disclosures: The authors have no conflicts of interest relevant to this article.
Bariatric Times. 2021;18(12):8–10.
Abstract
Obesity rates in the United States continue to rise, particularly among aging patients. There is an estimated 60 million people in rural areas, which have 20 to 30 percent less access to medical care. Literature has shown that people living in rural areas are sicker, poorer, and older than urban populations. This elderly population is not immune to obesity or obesity-related diabetes, hypertension, hyperlipidemia, and osteoarthritis. Based on a review of the literature, there is little standardized treatment for the geriatric bariatric cohort, and cutoff parameters are variable. The primary aim of the present study is to evaluate bariatric surgery outcomes in the geriatric population. This study is a retrospective chart review of 34 patients over the age of 65 years who underwent bariatric surgery. The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Project (MSAQIP) was accessed to evaluate weight loss. A chart review was implemented from 2016 through 2020 and data for patients who presented for bariatric surgery was evaluated. Data retrospectively collected included patient demographics and body mass index (BMI). In addition, we investigated complication rate, readmission rate, mortality rate and length of hospital stay. We analyzed the outcomes at one year. Preoperative average BMI was 48.3kg/m2 and postoperative average BMI at one year follow up was 36.9kg/m2. Total percentage body weight loss was 18.4 percent. The percentage of BMI reduction was 23.6 percent. The percentage of excess BMI lost was 48.9 percent. The complication rate was 5.9 percent. The average total length of stay was 2.5 days. Bariatric surgery can be performed in the elderly population with a comparable complication rate with the average age population. Bariatric surgery in a rural setting can achieve substantial weight loss in the geriatric population and help with the resolution of comorbidities.
Keywords: Geriatrics, bariatric surgery
The global geriatric population is continuously enlarging as lifespans increase uniformly, especially in the rural setting. This portion of the global population is not immune to obesity. Unfortunately, the elderly population suffers more drastically from the aftereffects of obesity-related comorbid conditions. Because of this, it is important to extend and extrapolate the benefits of bariatric surgery to this generation of the patient population.1 While there is some consensus from the American Society for Bariatric and Metabolic Surgery (ASMBS) on the rough guidelines for age qualifications for bariatric surgery, there are no widespread standards in practice. Age qualifications are program specific. Therefore, we have performed a review on the aging bariatric population over the last four years to evaluate specific guardrails and restrictions for bariatric surgery.
The setting is a rural academic university center in Southwest Virginia. It is a 750-bed quaternary care private teaching hospital equipped with a bariatric surgery center of excellence. This designation is given by the ASMBS. The criteria to become an accredited center include minimum annual case volumes, structural requirements, and multidisciplinary care including psychologists, nutritionists, medical bariatricians.
The aim of this study was to review the impact of bariatric surgery on the elderly population in a rural setting, including complications, operative weight loss results, and impact on comorbid conditions.
Methods
A retrospective review of patients older than 65 years who underwent bariatric surgery at Carilion Clinic was conducted. The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Project (MSAQIP) database was accessed to evaluate the weight loss. A chart review was implemented from 2016 through 2020 and data for patients who presented for bariatric surgery at Carilion Clinic was evaluated. Data retrospectively collected included patient demographics (i.e., age, sex, height, weight, race), body mass index (BMI), American Society of Anesthesiologists (ASA) score, medical history, surgical history, and smoking history. In addition, we investigated the complication rate, readmission rate, mortality rate, and length of hospital stay.
Selection criteria. Data was collected from patients who underwent laparoscopic sleeve gastrectomy or laparoscopic Roux-en-Y gastric bypass at Carilion Clinic from 2016 to 2020. Exclusion criteria consisted of revisional bariatric surgery and laparoscopic gastric band placement and patients with less than six months of follow up. Inclusion criteria consisted of all patients undergoing bariatric surgery at Carilion Roanoke Memorial Hospital who were aged 65 years or older. All patients underwent preoperative multidisciplinary clearances by our nutritionist, bariatric psychologist, and medical bariatricians prior to surgical intervention.
All patients met the criteria for bariatric surgery using the guidelines published by the ASMBS, consisting of a BMI greater than 40kg/m2 or a BMI greater than 35kg/m2 with obesity-related comorbid conditions.
Objectives
Our study aims to evaluate the efficacy of bariatric surgery in the geriatric population. Primary endpoints were to evaluate bariatric surgery outcomes in the geriatric population, evaluate the safety of bariatric surgery in this patient population, and analyze resolutions of comorbid conditions in the elderly population after bariatric surgery.
Results
Thirty-six patients who underwent bariatric surgery were identified. One patient with lap band repositioning was excluded. We were unable to follow up with one patient for at least 30 days, and therefore, the patient was excluded from the study.
The group comprised of 25 female patients and nine male patients (Figure 1). Fifty-eight percent of patients (20 patients) underwent laparoscopic sleeve gastrectomy and 42 percent (14 patients) underwent laparoscopic gastric bypass (Figure 2). All patients underwent intraoperative leak testing. The average age of the cohort was 67.8 years. The average height was 65.3 inches. The average preoperative BMI was 48.8kg/m2. The average preoperative weight was 271.8lbs (Table 1).
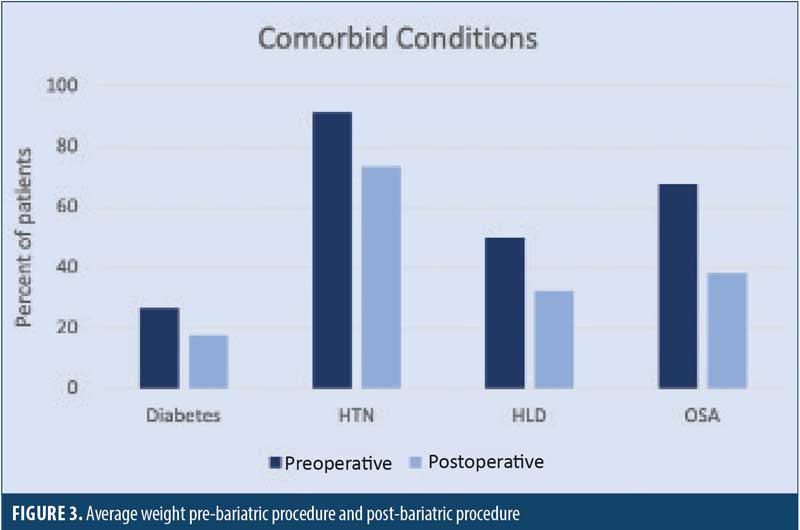
Comorbid conditions were also analyzed. The following preoperative comorbid conditions were identified: 26.5 percent of patients (9 patients) preoperatively had a diagnosis of Type 2 diabetes mellitus; one patient had Type 1 diabetes; the average preoperative glycated hemoglobin (HbA1c) was 7.01 percent; 14.7 percent of patients (5 patients) had chronic obstructive pulmonary disease (COPD); 63.8 percent of patients (23 patients) had obstructive sleep apnea (OSA); 91.4 percent of patients (31 patients) had hypertension requiring medication; and 50 percent of patients (17 patients) had hyperlipidemia. The average ASA Classification was 2.94 (Table 2).
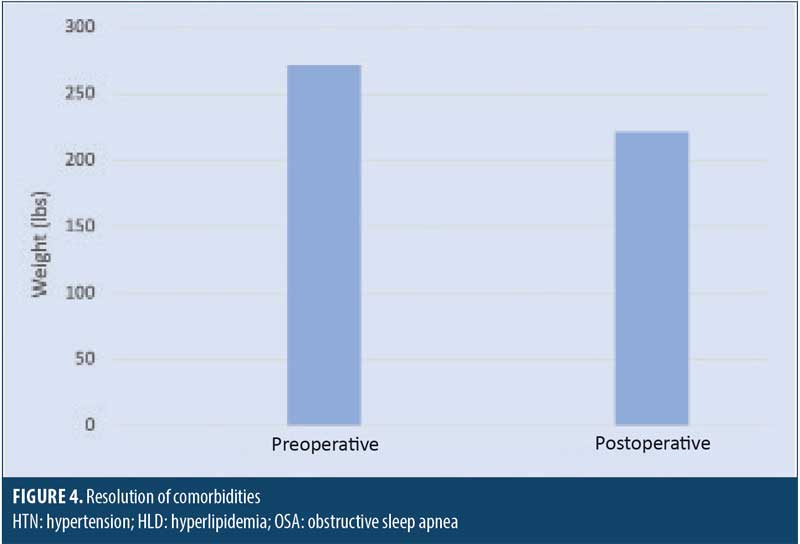
Patients were followed for 12 months. The average postoperative weight was 221.8lbs. The average postoperative BMI was 36.8kg/m2 (Table 3a). A comparison of pre- and postoperative weight is shown in Figure 3. Total change in BMI was 11.4 points. Total percent body weight loss was 18.4 percent. The percentage of BMI reduction was 23.6 percent. The percentage of excess BMI lost was 48.9 percent (Table 3b). The average duration of operation was 122 minutes. The average total length of stay was 2.5 days. All patients were discharged home with self-care.
Resolution of comorbidities were analyzed at the one year follow-up. OSA was present in 63.8 percent of patients preoperation and 38.2 percent postoperation. Hypertension was present in 91.4 percent of patients preoperation and 73.5 percent postoperation, with 81.6 percent of patients requiring a medication for hypertension, compared to 91.2 percent preoperation. Hyperlipidemia was present in 50 percent of patients preoperation and 32.4 percent postoperation (Table 4 and Figure 4).
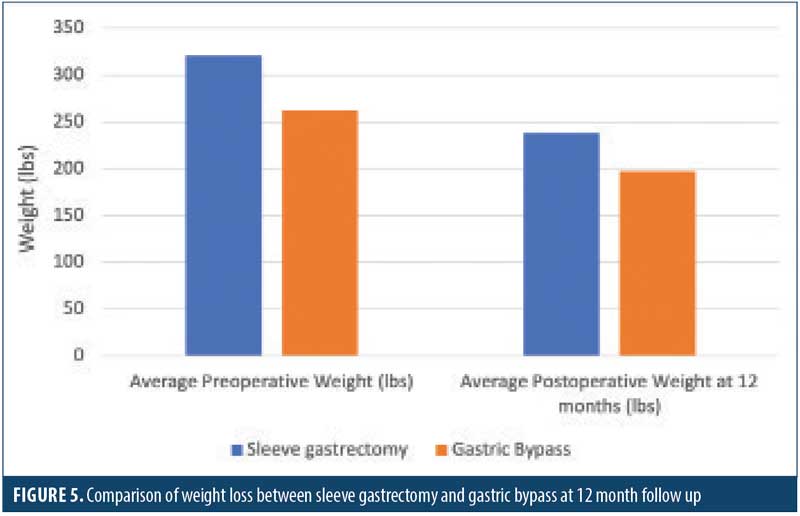
Further analysis was conducted to evaluate sleeve gastrectomy versus gastric bypass. The average preoperative weight for the sleeve gastrectomy cohort was 320.9lbs, with an average preoperative BMI of 50.8kg/m2. The average preoperative weight for patients who underwent gastric bypass was 262.5lbs, with an average preoperative BMI of 45.8kg/m2. The average postoperative weight for patients who underwent sleeve gastrectomy was 238.0lbs, with an average BMI of 38.1kg/m2
(Table 5). This equates to an average weight loss of 82.9lbs for patients who underwent sleeve gastrectomy (Figure 5). The average postoperative weight for patients who underwent gastric bypass was 197.3lbs, with an average postoperative BMI of 34.4kg/m2 (Table 5).This equates to an average weight loss 65.5lbs in patients who underwent gastric bypass (Figure 5).
Specifically looking at complications, there were no anastomotic or staple line leaks. There were no conversions from a laparoscopic or laparoscopic-assisted robotic operation to an open procedure. There were no unplanned postoperative intubations. There were no postoperative superficial infections. There was one deep space infection, which was a perisplenic abscess treated conservatively with drain placement; the patient was readmitted and interventional radiologic drain placement was performed on the perisplenic abscess. There was one reoperation in 30 days for an incisional hernia. There were no postoperative incidents of urinary tract infection. There were no postoperative myocardial infections or pulmonary embolism. There was a zero percent mortality rate (Table 6). The overall readmission rate was 2.9 percent. The overall reoperation rate was 2.9 percent. The overall complication rate was two out of 34 patients, or 5.9 percent.
Discussion
With the advent of laparoscopic techniques, the safety and outcomes profile of bariatric surgery has met a steady state, allowing for resolution of comorbidities in otherwise complex patients. Reviewing our data, the risk and safety profile
advantages of minimally invasive bariatric surgery translates to the geriatric cohort.2 Comorbid conditions have similar average rates of resolution as younger patients, even though the average duration of comorbidity is ostensibly longer in the geriatric group. When reviewing the literature, our complication and readmission rates were similar to those previously published.3–5 The elderly population oftentimes has more comorbid conditions, and therefore, we need to strongly consider extending surgery to this cohort. In terms of which operation to offer, our study showed improved outcomes in weight loss in both cohorts—those receiving a sleeve gastrectomy and those receiving a gastric bypass. Each patient should be offered an individualized approach to determine which surgery would serve their weight loss needs, as well as bring improvement or resolution of their comorbid conditions. Both operations had no mortality rate and a low complication profile of 5.9 percent. In our study, geriatric patients benefitted from bariatric surgery with improvement in comorbid conditions and substantial weight loss.
Limitations
The limitation of this study is preoperative weight for first initial visit was used. Due to the process of bariatric surgery, which can take up to 1.5 years to complete, certain individual weights can be ambiguous, as patients might have a higher recorded weight on the day of surgery or during the preoperative process.
Conclusion
Bariatric surgery has evolved drastically over the past two decades due to the introduction of laparoscopic surgery. This translates into shorter hospital lengths of stay and quicker return to baseline activities. Our outcomes show positive results in the rural geriatric population.
Given the safety profiles of modern bariatric surgery, there should not be a hard age cut-off for bariatric surgery in the rural setting; instead, elderly patients interested in bariatric surgery have a discussion at a multidisciplinary meeting involving a bariatrician, surgical team, psychologist, and nutritionist. Each case’s risks and benefits should be weighed on an individual setting, focusing on the patient’s functional status rather than chronological age.
Our future directions include comparing the resolution of comorbid conditions between the elderly population and the general population. We aim to collaborate with Obesity Internal Medicine Department at our facility to eventually develop a screening protocol for choosing geriatric patients who would serve as suitable candidates for bariatric surgery. We will continue to track outcomes in this population to further delineate improvement in comorbidities at the 3- and 5-year time periods.
Statement of Ethics
This study was approved by the Virginia Institutional Review Board.
References
- Gloy VL, Briel M, Bhatt D, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomized controlled trials. BMJ. 2013;347:f5934.
- Susmallian S, Raziel A, Barnea R, Paran H. Bariatric surgery in older adults: should there be an age limit? Medicine (Baltimore). 2019;98(3):e13824.
- Moon RC, Kreimer F, Teixeira AF, et al. Morbidity rates and weight loss after Roux-en-Y gastric bypass, sleeve gastrectomy, and adjustable gastric banding in patients older than 60 years old: which procedure to choose? Obes Surg. 2016;26(4):730–736.
- Abbas M, Cumella L, Zhang Y, et al. Outcomes of laparoscopic Sleeve gastrectomy and Roux-en-Y gastric bypass in patients older than 60. Obes Surg. 2015;25(12):2251–2256.
- O’Keefe K, Kemmeter P, Kemmeter K. Bariatric surgery outcomes in patients aged 65 years and older at an American Society for Metabolic and Bariatric Surgery Center of Excellence. Obes Surg. 2010;20:1199–205.
Category: Past Articles, Review




