Raising the Standard: Enhanced Recovery Goals in Bariatric Surgery (ENERGY): The Second MBSAQIP National Quality Improvement Project
 by Anthony T. Petrick, MD, FACS, FASMBS, and Dominick Gadaleta, MD, FACS, FASMBS
by Anthony T. Petrick, MD, FACS, FASMBS, and Dominick Gadaleta, MD, FACS, FASMBS
Dr. Petrick is the Quality Director at Geisinger Surgical Institute and Director of Bariatric and Foregut Surgery for Geisinger Health System in Danville, Pennsylvania. Dr. Gadaleta is Chair of the Department of Surgery at Southside Hospital and Director of Metabolic and Bariatric Surgery at North Shore University Hospital, Northwell Health in Manhasset, New York; and Associate Professor of Surgery at Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York.
Funding: No funding was provided for this article.
Disclosures: The authors reports no conflicts of interest relevant to the content of this article.
Bariatric Times. 2019;16(5):12.
“It is not the strongest of the species that survives, nor the most intelligent, but the one most responsive to change.”
-Charles Darwin
Over the past several months, team-based care has been a recurrent focus of our column. We have reviewed the multidisciplinary team-approach to patient selection, planning, and perioperative care of patients undergoing bariatric surgery. We reviewed the implementation and outcomes of ProvenCare® Bariatric as an example of this approach. Last month, we reviewed the fundamental elements of enhanced recovery, focusing on key elements in each phase of care. This month, we will review the design, implementation, and outcomes of the second national quality improvement project of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) called Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY).1 ENERGY, which was launched in November 2016 and led by then president of the American Society for Metabolic and Bariatric Surgery (ASMBS) Stacy Brethauer, MD, implemented an enhanced recovery protocol in patients undergoing bariatric surgery. The MBSAQIP Data Registry was used to identify those centers that were high outliers for extended length of stay (XLOS), defined as four or more days. Seventy-four MBSAQIP centers with XLOS were invited to participate, and 36 sites were enrolled. Patients undergoing primary laparoscopic gastric bypass, sleeve gastrectomy, and gastric band were included in the study.
The project was administered using center mentors and monthly webinars. Implementation began with a “run-up” period from January through June 2017. This gave centers an opportunity to embed process elements into their practice and electronic health records, as well as training the Metabolic and Bariatric Surgical Clinical Reviewer Requirements (MBSCRs) in the use of custom data fields in the registry. Time was also needed for engagement of the anesthesia services responsible for many of the intraoperative protocol elements.
A total of 26 elements were developed and implemented. The elements created care pathways for all enhanced recovery phases of care. These included prehabilitation and skin prep prior to surgery as well as tight glucose control and minimizing fluids, tubes, and drains intraoperatively with the limitation or elimination of postoperative radiologic studies. Pain protocols to reduce opioid use included regional blocks (transversus abdominus plane) and scheduled dosing of nonopioid analgesics before and after surgery. Elements were scored as optimal or nonoptimal.
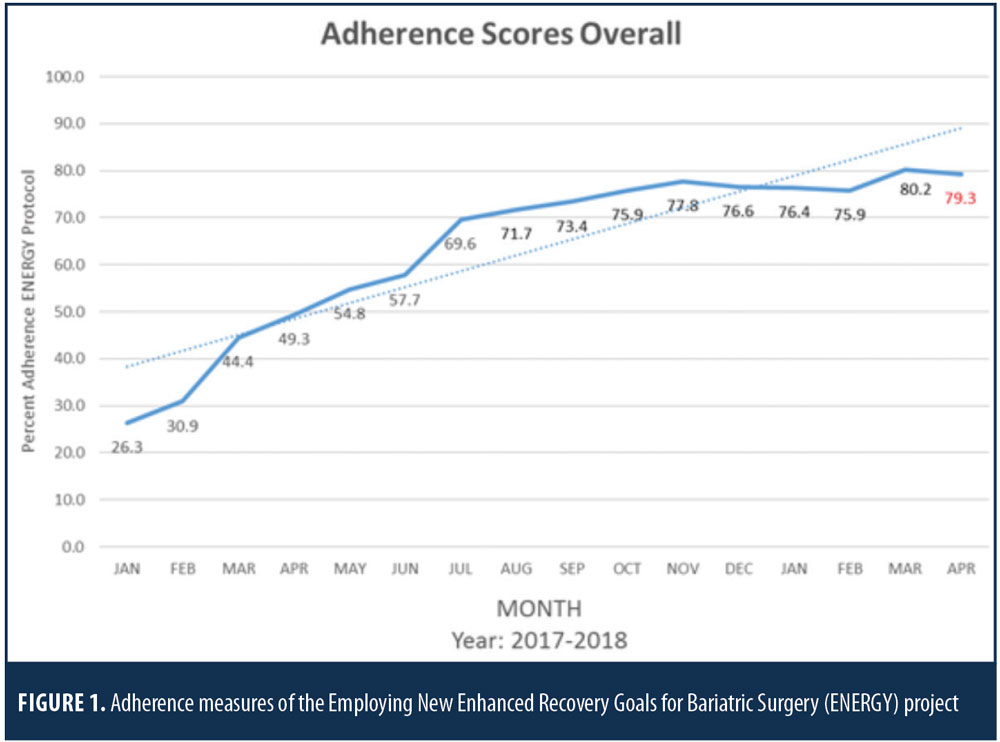
Dr. Brethauer reported ENERGY results at ObesityWeek 2018 in Nashville, Tennessee. Overall adherence to protocol elements improved during the six-month run-up phase. Adherence reached the target of 70 percent in July 2017 just as the project reached the “Go Live” phase (Figure 1). The Go Live phase was from July 2017 through June 2018. To evaluate the impact of the ENERGY protocol, extended length of stay (LOS) was selected as the primary endpoint. The overall rates of XLOS for pre- and postintervention were 8.1 and 4.5 percent, respectively. Higher levels of adherence to the protocol were associated with improvement in XLOS. A reduction in extended LOS was seen overall in centers participating in ENERGY compared to nonparticipating MBSAQIP centers.
The American College of Surgeons (ACS) Quality Programs continue to prioritize the development of tools to help surgeons implement enhanced recovery for its patients. In collaboration with the Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality, the ACS has launched the Agency for Healthcare Research and Quality (AHRQ) Safety Program for Improving Surgical Care and Recovery (ISCR). Clinical programs in colorectal surgery, orthopedics, and gynecology are currently enrolling with a planned launch of the emergency general surgery pathway in January 2020.
MBSAQIP plans to launch the third National Quality Improvement Project this year called Bariatric Surgery Targeting Opioids Postoperatively (BSTOP). The project will focus on the reduction of opioid use and prescribing after bariatric surgery. The ISCR team will host the two-part event, titled “Enhanced Recovery: Partnering to Improve Surgical Care and Recovery,” on July 18, 2019, prior to the ACS Quality and Safety conference in Washington, DC. This event will include a review of evidence-based perioperative care and advanced principles in enhanced recovery, highlighting that successful implementation of an enhanced recovery program can be achieved.
Next month’s Raising the Standard topic—Utilization of the EMR to facilitate quality improvement
References
- Brethauer, SA, Petrick A, Grieco A, et al. Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY): A Metabolic and Bariatric Surgery Accreditation and Quality Improvement (MBSAQIP) National Quality Improvement Project. Surg Obes Relat Dis. 2018;14(Suppl 11):S6).
Category: Past Articles, Raising the Standard



