Roux-en-O after Duodenal Switch: A Case Report
 by Daniel Prior, DO; Thomas Magnuson, MD; Gina Adrales, MD; Hien Nguyen, MD; Alisa Coker, MD; and Michael Schweitzer, MD
by Daniel Prior, DO; Thomas Magnuson, MD; Gina Adrales, MD; Hien Nguyen, MD; Alisa Coker, MD; and Michael Schweitzer, MD
Drs. Prior, Magnuson, Adrales, Nguyen, Coker, and Schweitzer are with the Johns Hopkins University, Department of Bariatric Surgery, Baltimore, Maryland.
Funding: No funding was provided.
Disclosures: The authors report no conflicts of interest relevant to the content of this manuscript.
Bariatric Times. 2019;16(5):14–15.
Abstract: We present a case of a patient who presented to our facility in Baltimore, Maryland, with emergent complications following revisional bariatric surgery (sleeve gastrectomy to biliopancreatic diversion with duodenal switch), which was performed outside of the United States. Upon further investigation, we discovered Roux-en-O, a rare surgical complication in which the Roux-en-Y is misconfigured and results in improper connection of the biliopancreatic limb to the gastric pouch. We suspected that the surgical errors were probably initiated by a misperception of the ends of the Roux and biliopancreatic limbs, which cascaded into further confusion of the common channel and Roux limb channel. Here, we discuss signs and symptoms, diagnosis, and treatment of a Roux-en-O misconfiguration and make recommendations for developing a routine to consistently track the proximal Roux limb.
Keywords: Roux-en-O, bariatric complications, medical tourism
A Roux-en-O is a rare surgical complication in which the Roux-en-Y is misconfigured This improper connection of the biliopancreatic limb to the gastric pouch can cause oral intolerance and severe bile reflux.1 The following describes the case of a patient who presented to our emergency department at Johns Hopkins University, Baltimore, Maryland, with complications from a BDP-DS that was performed during a medical tourism trip. Upon laparoscopic exploration, we diagnosed a Roux-en-O and proceeded with treatment.
Case Vignette
A 44-year-old woman arrived in our emergency department after a medical tourism trip where she had undergone a revision of a previous LSG to BPD-DS. The reason given for revision was unsuccessful weight loss experienced after the primary procedure. Postoperatively, at the international hospital, the patient was never able to tolerate a diet and, shortly thereafter, developed a leak that presented at the site of her previous drain. This matured into an enterocutaneous fistula from the duodenoileal anastomosis with no apparent free peritoneal leak. The patient had a nasoenteric feeding tube placed, but tube feeds immediately emptied through her enterocutanous fistula. According to the patient, clinicians at the international hospital instructed her to return to the United States and go to an emergency department. Surprisingly, the patient flew on a commercial airline with her nasoenteric tube and presented at our center.
Upon our initial evaluation, she appeared well and had normal vital signs. She was nondistended, and there were no signs of peritonitis on abdominal exam. Her workup comprised a computed tomography (CT) scan and upper gastrointestinal (GI) swallow study, which demonstrated the fistula and a dilated Roux limb. We performed an upper endoscopy and removed a suture with a knot from the small fistula opening along with incompletely formed staples. Additionally, we found a significant amount of bile in the stomach and proximal small bowel. We inserted fibrin glue into the fistula tract and a nasogastric tube placed on suction. After a few days of nasogastric decompression and total parenteral nutrition (TPN), the fistula closed. A repeat upper GI (Figure 1) showed pooling of contrast proximally after two hours and no further evidence of a fistula. We suspected a Roux-en-O configuration.

The patient was taken to the operating room for a laparoscopic exploration. Because of severe adhesions and unclear anatomy, this was converted to an open procedure. She was found to have a duodenoenterostomy to the biliopancreatic limb; however, the proximal Roux limb was not connected to the middle of the biliopancreatic channel (Figure 2b), as is seen with most Roux-en-O complications (Figure 2a shows the normal anatomy of BPD-DS). Instead, she had a completely disconnected Roux-en-O where the proximal Roux limb was anastomosed in a circle with the common channel, and there was no drainage of the biliopancreatic limb (Figure 2c).
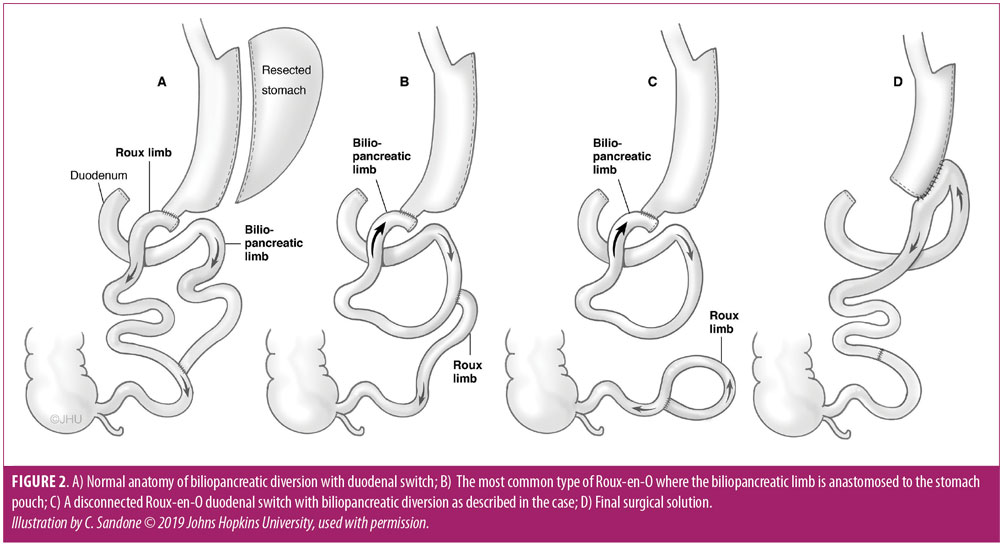
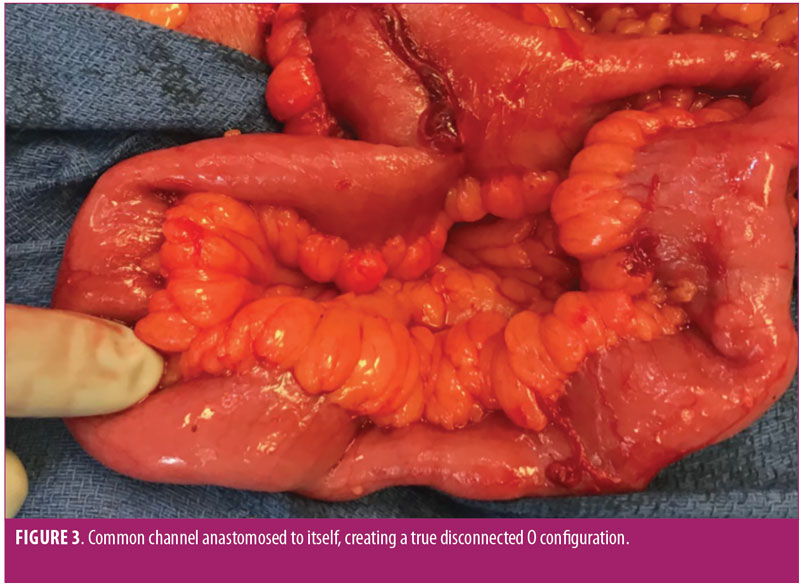
We proceeded to resect both the duodenoenterostomy with the pylorus/antrum and the O-shaped Roux/common channel (Figure 3). After correcting the anatomic orientation of the small bowel using the mesentery as a guide, we performed an enteroenterostomy where we reconnected the common channel to the biliopancreatic limb. We then performed a retrocolic loop gastrojejunostomy. Figure 2d depicts the final surgical solution. We considered performing a Roux-en-Y to prevent bile reflux, but the patient had a limited amount of small bowel, and we felt it was safest to preserve as much length of small bowel as possible. It appears that she might have had a significant amount of small bowel resected at the international hospital since we only resected approximately 35cm.
She recovered appropriately and by Postoperative Day 4, she was able to tolerate an oral liquid diet for the first time in three weeks since her original BPD-DS operation.
Discussion
In this particular patient case, we suspect that the errors were probably initiated by a misperception of the ends of the Roux and biliopancreatic limbs, which cascaded into further confusion of the common channel and Roux limb channel. Many other Roux-en-O configurations have been described in the literature.1,3–4 The simplest and likely most common form is an antiperistaltic Roux limb caused by mistakenly anastomosing the proximal Roux limb to the middle of the biliopancreatic limb and then taking the distal end of the biliopancreatic limb and connecting it to the gastric pouch (Figure 2b). In this configuration, the biliopancreatic limb still has a way to drain so that some of the enteric contents will enter the common channel. The case described here is a less common but more severe configuration.
Diagnosis of a Roux-en-O can be difficult. Fluoroscopic upper GI can be of assistance by demonstrating a reversal of the normal peristalsis and dilation of the Roux limb.1–4 Hepatobiliary iminodiacetic acid (HIDA) scan evaluation has also been proposed in case reports.2,3 As the radiotracer exits the biliopancreatic limb, it can sometimes be seen traveling into the stomach and esophagus. Despite radiographic hints, the gold standard of diagnosis will always be operative exploration1,3 where the surgeon should evaluate for Roux-en-O by carefully inspecting the mesentery to the biliopancreatic limb and the mesentery to the proximal Roux limb.
Conclusion
When investigating postoperative complications of RYGB or BPD-DS, the presence of significant amounts of bile within the Roux limb, along with chronic nausea, vomiting, and intolerance of meals should raise suspicion. While in most cases the bile reflux might be due to a distal bowel obstruction of the common channel, a Roux-en-O should be a consideration. This complication is devastating, but preventable,1,4 and a routine should be developed to consistently track the proximal Roux limb.
We recommend immediately marking the proximal Roux limb with a simple suture after dividing the jejunum. If at any point there is doubt about the limbs, then the biliopancreatic limb should be double checked by running it back to the ligament of Treitz. The suture in the Roux limb not only eliminates confusing the two ends of small bowel, but also assists later in retraction during creation of the upper anastomosis.
References
- Mitchell MT, Gasparaitis AE, Alverdy JC. Imaging findings in Roux-en-O and other miscontructions: rare but serious complications of Roux-en-Y gastric bypass surgery. AJR Am J Roentgenol. 2008;190:368–373.
- Sherman V, Dan AG, Lord JM, et al. Complications of gastric bypass: avoiding the Roux-en-O configuration. Obes Surg. 2009;19(8):1190–1194.
- Rebiai R, Destinval C, Benchabane M. Roux-en-O gastric bypass: about one case report and literature review. Surg Obes Relat Dis. 2017;13(10):1796–1800.
- Schrope BA, Daud A, Bessler M. Unintentional creation of reverse peristaltic alimentary limb during Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis. 2006;2(4):478–482.
Category: Case Report, Past Articles







