The Guidelines—They Are A-changin’!

by Adrian G. Dan, MD, FACS, FASMBS
Dr. Dan is Medical Director, Weight Management Institute at Summa Health in Akron, Ohio, and Associate Professor of Surgery at Northeastern Ohio Medical University (NEOMED) in Rootstown, Ohio
Funding: No funding was provided.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Bariatric Times. 2022;19(10):8–9.
We have all heard that familiar joke: “1991 just called…it wants its guidelines back.” For those who remember 1991, the world was a very different place. A gallon of gasoline cost about $1, the Dow Jones Industrial Average reached 3,000, and “1991” would have called because texting was not yet “a thing.” Noteworthy events included the Gulf War and the dissolution of the Soviet Union. That year, important to the history of metabolic and bariatric surgery (MBS), the National Institutes of Health (NIH) organized the third and last major consensus conference focused on obesity and its treatment. This meeting produced the guidelines that would be referenced for the next three decades on the indications for gastrointestinal surgery to combat obesity and its associated conditions.

Much has changed since then, in our world and in our discipline. The prevalence of obesity has exploded, resulting in an epidemic of global proportions. The chronic nature, etiology, and pathophysiology of this disease, as well as its associations with hundreds of other conditions, have been better defined. The metabolic mechanisms that cause obesity and the impact of MBS are now better understood. Operations have been changed and refined time and again to build upon the shortcomings of previous techniques, and the utilization of laparoscopic and robotic approaches has become the standard of care. Patients with this chronic disease are now cared for by multidisciplinary teams in comprehensive and accredited centers of excellence. Contemporary MBS operations are now some of the best studied procedures, with safety profiles that are similar to commonly performed operations, such as cholecystectomy.
In 1991, Dr. Walter Pories’ seminal article delineating the potential of bariatric surgery for the treatment of Type 2 diabetes mellitus was still five years away. The increased need and utilization of bariatric procedures spurred an avalanche of literature, including a dozen randomized, controlled trials proving the capabilities of bariatric surgery as the most effective treatment for obesity and Type 2 diabetes. Other high-quality studies were published, showing the effectiveness of MBS to resolve a myriad of obesity-associated conditions, increase longevity, improve quality of life, and decrease the incidence of malignancy and cardiovascular events. New pharmaceutical agents have been developed to work in synergy with surgical therapy. In patients with a lower body mass index (BMI), the concept of metabolic surgery has been solidified for the treatment of Type 2 diabetes.
Over the past three decades, our discipline has been transformed in countless ways. In light of all these notable changes, the sorely outdated guidelines from 1991 are no longer in line with the new understanding of obesity and its treatments. These indications are not supported by the current scientific evidence or favorable risk-to-benefit ratio of contemporary operations. Unfortunately, they have remained the predominant reference among authors, insurance carriers, healthcare policy makers, and primary care providers. As a result, patients with obesity might be discouraged to seek treatment, denied insurance coverage, or even refused consideration for a surgical referral.
Changing such established principles and ideologies is not an easy undertaking. Strong headwinds include correcting old habits for medical professionals and eradicating the misguided public perception of obesity and surgical treatment. The NIH is no longer involved in making such guidelines, and the responsibility to officially update them rests with our professional societies. A movement to produce this change was one of the principle objectives in the American Society for Metabolic Surgery (ASMBS) presidency of Dr. Shanu Kothari. In this edition of Perspectives, he joins us to describe the essential steps we must take collectively and individually as we transition to the newly unveiled ASMBS/International Federation Surgery of Obesity and Metabolic Disorders (IFSO) indication. These guidelines, rooted in scientific evidence, may consequently better serve the needs of patients with obesity and associated conditions.
Guest Perspective
by Shanu N. Kothari, MD, FACS, FASMBS
Immediate Past President of the American Society for Metabolic and Bariatric Surgery (ASMBS), Chair of Surgery – Prisma Health, Professor of Surgery – University of South Carolina, Greenville, South Carolina
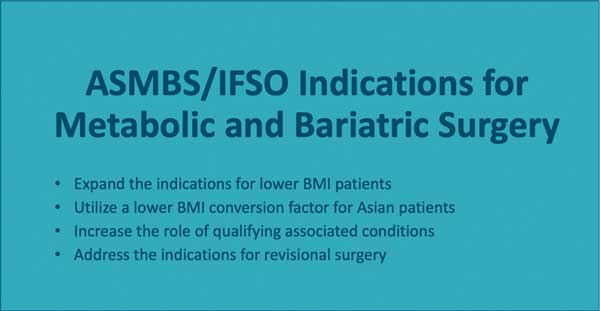
It is hard to believe that we, as a society, still quote a 31-year-old document as our guiding principle for indications for metabolic and bariatric surgery (MBS). It is time to abolish and update these outdated indications. Last summer, at our annual American Society for Metabolic and Bariatric Surgery (ASMBS) Executive Council retreat, I asked the council to approve the commissioning of updated guidelines. Under the guidance of Dan Eisenberg and our clinical issues committee, I am happy to announce that the document is now complete. It has expanded indications for MBS for patients with a lower body mass index (BMI). It will have a lower BMI conversion factor for those of Asian ethnicity, as well as a more comprehensive and expanded role of qualifying comorbid conditions and revisional surgery. However, this document in and of itself is not enough to turn the tide against the discriminatory practices of our payors. It will be up to our ASMBS members to see it successfully transform the way we care for patients in the United States (US) and around the world. We will need those of you on the front lines to challenge those who are quoting a 31-year-old document for denial of our life-changing and life-saving surgery. Ask your peers if they use 31-year-old documents for indications regarding stroke care or cardiology care. My guess is that is not the case. Therefore, we must do away with abiding by the 1991 statement and use contemporary, evidence-based guidelines, as outlined in this document, moving forward. It will take this kind of grassroots effort to change the tide and perception of payors, as well as providers, with our updated, contemporary, evidence-based indication for the care that we provide.

Knowing our international colleagues face similar struggles with access to care and evidence-based indications for MBS, we worked in conjunction with the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) leadership, including current president Scott Shikora and immediate past president Lillian Kow, to get board approval from IFSO as well. I have approval from both senior editors of Surgery for Obesity and Related Diseases (SOARD) and Obesity Surgery, Raul Rosenthal and Scott Shikora, respectively, that a day will come when our papers will not be accepted in either of our leading journals if we reference the 1991 guidelines. We will need to reference the ASMBS/IFSO guidelines for Metabolic and Bariatric Surgery 2022. This will allow us to spread a powerful, worldwide message that is unified around one agreed-upon, contemporary, evidence-based set of guidelines. I wish our members the best of luck in improving access to care for our patients, as they will now be armed with the most powerful guidelines in over three decades.
Category: Past Articles, Perspectives




