Welcome to Northeast Georgia Medical Center—Gainesville, Georgia

by Amy Smith, MSN, RN, CBN
Ms. Smith is the Bariatric Program Manager at the Bariatric Weight Loss Center, Northeast Georgia Medical Center in Gainesville, Georgia.
Funding: No funding was provided.
Disclosures: The author reports no conflicts of interest relevant to the content of this article.
Bariatric Times. 2023;20(1):16–21.
Northeast Georgia Health System (NGHS) is a four hospital, not-for-profit health system serving more than one million people across more than 19 counties in Northeast Georgia. Our Northeast Georgia Medical Center (NGMC) Gainesville campus has 557 beds and has a 32-bed inpatient surgical unit with designated bariatric beds. With these accommodations and our American College of Surgeons (ACS)-verified Level II trauma center, we are able to manage patients of all sizes and complexities.
With a rich history in bariatrics dating back to the 1970s with Dr. Ken Dixon, Sr. and Dr. Jim Leigh, the bariatrics service line was officially established in 1990 and has been an accredited center since 2006. The surgeons in our program today have a combined 60 years of experience and have performed over 10,000 bariatric surgeries. The nursing staff on our bariatric unit take great pride in taking care of this population, as many of them have been working with these surgeons most of their nursing careers and know the impact these surgeries have on the lives of their patients.
Our Staff
Our system’s bariatric center works closely with our hospital-owned physician practice, Northeast Georgia Physicians Group (NGPG), and a local primary care and multispecialty practice, Longstreet Clinic, to provide both medical and surgical treatment options to patients. The leadership of NGMC’s Bariatric Weight Loss Center is shared by Dr. Robert Richard, Metabolic and Bariatric Medical Director; Dr. Christina Nguyen, Obesity Medicine Medical Director; and Amy Smith, Bariatric Program Manager. We have four bariatric surgeons and nine providers who participate in our obesity medicine program. This team recently helped us achieve our re-accreditation as a Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) comprehensive center, with a new Obesity Medicine accreditation. 
Within the bariatric center at NGMC, the Bariatric Program Manager partners with the business development and marketing teams to promote our program and increase awareness of the treatment of obesity in the community through rounding in the primary care and specialty offices, attending health fairs, providing education, and advertising the program. Our goal is to increase awareness of the disease of obesity and ensure that healthcare providers and our patients understand that obesity is a chronic relapsing disease that is best treated with a multidisciplinary approach with an emphasis on support. She is also a certified bariatric nurse (CBN) who teaches our preoperative and discharge classes and rounds on our bariatric unit to ensure that we maintain the highest level of care for our specialty.
Our Bariatric Program Specialist runs our front office, fielding calls and internet interest in our program. She attentively listens to patient concerns, answers their questions, and helps to connect them with the best treatment option for them. She also ensures that our patients understand that we have support services available to them, no matter if they choose to start with nutritional counseling, the intragastric balloon, medical weight loss, or surgery. Having a dedicated specialist working with patients as they express interest in treatment for obesity has proven to increase referrals in our program because patients feel that they are understood and supported every step of the way.
We have a registered nurse (RN) who works part-time as our Metabolic and Bariatric Surgery (MBS) Clinical Reviewer, entering all of our case data into the MBSAQIP database and tracking our long-term follow-up data. She has also been instrumental in working with our information technology (IT) team to create several EPIC® reports to track our quality improvement (QI) projects, as well as our bariatric data registry for our Obesity Medicine accreditation.
Our registered dietitian (RD) has a unique role within the program, as she provides medical nutrition therapy to patients who are referred by their primary care physician (PCP) or cardiologist to assist with better management of hypertension or high cholesterol and provides free lifetime visits to patients who have had bariatric surgery at our organization. We feel that offering these visits for free postoperatively is another way that we can remove barriers for our patients and help to maximize their success. She is also a chef who creates and demonstrates new, bariatric-friendly recipes once per month through our cooking classes, which are published to our public YouTube channel (@NGMCbariatrics). Additionally, she is a certified medical interpreter, which has allowed her to support our growing Spanish-speaking population through RD visits, educational videos, and support groups. She works closely with the other four dietitians in the practices and recently participated in a project to evaluate our postoperative diet progression, compared to others in the nation, so that our surgeons could standardize it for all patients to decrease confusion in group classes, support groups, and our private Facebook group.
We
have one behavioral health specialist who provides individualized and family therapy in-person and via telehealth. He joined our team at the beginning of the COVID-19 pandemic in March 2020 and now sees an average of 125 patients per month. He works closely with the three psychologists who conduct preoperative evaluations. He also coordinates our support groups by meeting with a multidisciplinary team quarterly to discuss common issues that are seen by the team and sets the schedule of support group topics three months in advance. Our support groups are topic-driven and moderated by either a behavioral health specialist, RN, or RD. Unique topics we have recently covered include eating healthily out of your own garden, breaking the cycle of childhood obesity, and distinguishing between head hunger and physical hunger.
Our Facility
The 32-bed designated bariatric and surgical unit boasts breakaway half doors that can be opened along with the main door to easily accommodate bariatric beds, 1,000-pound capacity ceilings lifts, 10 hospital-owned bariatric beds, and numerous shuttle chair options with high weight capacities. We have a dedicated discharge lounge with bariatric seating to accommodate our patients and their support persons for discharge education.

Program Demographics
Our surgeons perform over 400 surgeries per year, including sleeve gastrectomy, Roux-en-Y gastric bypass (RYGB), duodenal switch, and complex revisional procedures. Our surgical population is 80 percent female, with an average age of 41 years and average body mass index (BMI) of 40kg/m2. We are able to treat all patients internally and do not have a weight requirement. In addition to surgical treatment, our obesity medicine specialists have seen nearly 2,500 patients in 2022.
MBSAQIP Accreditation Process
Obtaining our reaccreditation for the MBSAQIP Comprehensive Surgical program virtually in 2022 was a different experience that required another level of preparation. However, we organized all important documents virtually in easily accessible folders, which made the whole day flow well. Surprisingly, the level of engagement and conversation was equal to that of the in-person visits from the past and made it an enjoyable experience.
 Seeking our initial Obesity Medicine accreditation was timely, as we had just finished our data collection project. This was the biggest challenge for us because we have nine providers participating in obesity medicine alongside our MBS program at several different locations, so using our existing EPIC® system made logical sense. “It took pulling our hospital IT team, bariatric center staff, and physicians from both practices together for several brainstorming sessions and having our lead IT physician build out the custom data points through SmartSets using a bariatric registry data pool to accomplish our goal in just under one year. It was a big lift, but having the support and engagement of the IT physicians made it possible for us,” said Dr. Christian Nguyen, Medical Director for Obesity Medicine at NGMC’s Bariatric Weight Loss Center.
Seeking our initial Obesity Medicine accreditation was timely, as we had just finished our data collection project. This was the biggest challenge for us because we have nine providers participating in obesity medicine alongside our MBS program at several different locations, so using our existing EPIC® system made logical sense. “It took pulling our hospital IT team, bariatric center staff, and physicians from both practices together for several brainstorming sessions and having our lead IT physician build out the custom data points through SmartSets using a bariatric registry data pool to accomplish our goal in just under one year. It was a big lift, but having the support and engagement of the IT physicians made it possible for us,” said Dr. Christian Nguyen, Medical Director for Obesity Medicine at NGMC’s Bariatric Weight Loss Center.
Long-term Follow-up
Like all accredited centers, we call our patients and send letters if they miss their follow-up appointment(s) and continue to reach out unless they have missed two consecutive follow-up periods. In addition, we encourage all new patients to join our private Facebook group to increase awareness of the need for continued long-term follow-up. This private group is monitored by CBNs, dietitians, and behavioral health specialists, so if we see that someone is struggling, we will either leave a comment suggesting that they follow-up or contact them directly.
Complications Related to Patient Nonadherence
Follow-up and support are key to keeping patients engaged with others who can hold them accountable and keep them motivated to maintain healthy lifestyle habits and avoid certain behaviors that can be detrimental to them postoperatively. For instance, patients returning to smoking or use of nonsteroidal anti-inflammatory drugs (NSAIDs) after surgery is a concern, especially if they come back with a marginal ulcer requiring intervention. We have increased our focus on preoperative education in this area to highlight awareness of this risk.
Patient-centered Care
Our patients can come to us confident that we will treat them with respect, knowing that obesity is a disease, and we treat it as such with several treatment options. Our patients are educated through an initial, online seminar; nurse and dietitian counseling in the office setting; preoperative classes to prepare for the preoperative diet and hospital experience; and weekly support groups, in-person or virtually through Zoom®, with links provided through our private Facebook group or monthly emails. We also offer free monthly weight lifting, yoga, and cooking classes for our patients.

Technological Advances
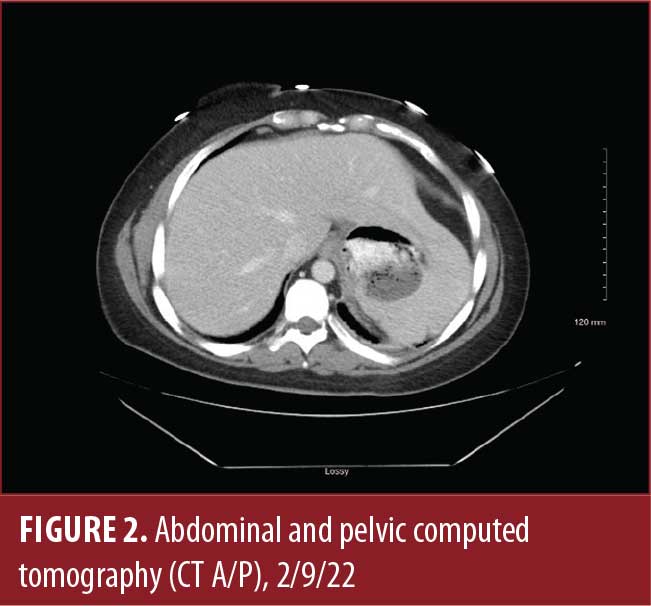
Our program was an early adopter of robotic surgery, with Dr. Alex Nguyen using the da Vinci surgical system to perform the first robotic RYGB in the state of Georgia in 2008. Since then, both Dr. Robert Richard and Dr. Alex Nguyen have become Surgical Review Corporation (SRC) robotic surgeons of excellence.
“Our institution has always embraced early adoptions of innovative technology to better provide care for our bariatric patients,” said Dr. Alex Nguyen. “Prior to being a mainstay presence in bariatric surgery, we implemented robotic surgery back in 2008. In addition to primary routine cases, this platform has revolutionized the tackling of all our complicated bariatric patients from difficult revisions, duodenal switches, and conversions from other general surgical foregut surgeries. While doing so, we have provided outcomes with very low complication rates, quicker return to daily life activities, and increased patient satisfaction in some of the most challenging cases. Our mastery of robotic bariatric surgery has positioned our hospital to be not only a teaching center for our general surgery residency program, but also a center to provide case observations and education to surgeons throughout the country and internationally. We are always attempting to be progressive in instilling contemporary techniques and novel equipment to continue to meet the demands of what our patient population needs.”
Surgical Scheduling
Both our hospital-based program and surgeons’ offices use the EPIC® electronic medical record (EMR), which allows for transparent and consistent access throughout the continuum of care for all providers. Our experts in insurance verification and surgical scheduling in the practice setting schedule the surgeries by collaborating with our hospital scheduling team.
Purchasing
We have an organizational purchasing department who oversees pricing contracts, and we take any equipment and supply requests to that group to be vetted and approved.
Patient Selection
We follow our inclusion clinical pathways to determine who is a candidate for the intragastric balloon or MBS.
Access to Care
Our MBS Medical Director, Dr. Robert Richard, is a member of the Georgia state American Society for Metabolic and Bariatric Surgery (ASMBS) chapter. During the COVID-19 pandemic, this group advocated for increased access to care for our state health employees. Through these efforts, the Georgia State Health Benefit Plan began covering MBS in January 2022. The state covers over 500,000 people, so these efforts could impact many in our state. Our center also has competitive self-pay pricing for patients who do not have bariatric coverage, with the option to take advantage of our one-year interest free payment plan.
“We know that obesity affects nearly every aspect of our health, and losing weight not only improves quality of life now, but can lead to less health problems down the road,” said Dr. Robert Richard, Medical Director for the Bariatric Weight Loss Center at NGMC and surgeon at Longstreet Clinic. “This change in coverage will mean more people having access to our services so they can improve their health long-term.”
Cost and Efficiency
Our program has participated in QI projects to improve efficiency and decrease our length of stay to reduce cost. We identified that we were not efficiently walking our patients after surgery; with only 62 percent of them walking within our goal of six hours after surgery, our patients were at an increased risk of developing blood clots. Through staff education, sharing our data, and increasing the awareness of the patient safety risk associated with it, we have increased the compliance to 95 to 100 percent, with patients typically walking immediately after arrival to the bariatric unit. We have also decreased the length of stay of our inpatients from 33 to 26 hours by instituting a group discharge class and focusing on early discharge orders for those who meet criteria to safely go home.
We perform an annual evaluation of case cost by surgeon that can be drilled down to supply cost for further evaluation and comparison. Having the surgeons openly discuss their techniques and preferences has allowed them to consider cheaper options, leading to a cost savings.
Patient Safety

At the beginning of the COVID-19 pandemic, our organization stopped all elective cases and cases that were nonemergent that needed to stay overnight, making access to care difficult for our patient population. To address this, we began educating our same-day surgery unit on bariatric cases and had the surgeons meet to determine the best criteria for outpatient bariatric cases. To have same-day bariatric surgery, the patient had to be selected by their surgeon. Our Bariatric Program Manager rounded on the patients to ensure they were safe and supported the staff to make sure that our quality outcomes were not compromised. We successfully completed 34 bariatric cases, including sleeve gastrectomies and gastric bypasses, during that time without seeing an increase in emergency department (ED) visits or complications related to the early discharge. We learned that patient selection was key and that patients with a BMI between 35 and 50kg/m2, aged less than 60 years, and with fewer comorbidities did very well in this setting. We excluded patients from same-day surgery if they had chronic pain issues, and only chose patients that the surgeons felt were going to be motivated to go home.
To safely care for patients of all sizes, our hospital is well equipped with 1,000-pound Arjo Huntleigh® ceiling lifts in select rooms and 1,000-pound SizeWise® shuttle chairs, stretchers, and several hospital owned HillRom Compella® bariatric beds. We also have Prevalon® mobile air transfer systems and have had several ambulances furnished with the Stryker TranSafe Powerload® wench systems.
Staff Education
All employees in our organization are educated at orientation and annually on bariatric sensitivity. Staff caring for the bariatric surgical patients complete additional education on safe patient handling and complication recognition. Additional education is provided through staff meetings quarterly for our staff in the designated bariatric unit.
Emerging Technology
Our behavioral health specialist reported seeing several patients who struggled with anxiety and depression. Guided meditation can help with these issues, as well as withdrawal.1 We recently invested in an Oculus Quest 2, which is a wireless all-in-one virtual reality (VR) headset. When our therapist identifies a patient he feels would be a good candidate for guided meditation, he places them in a room with the device set to their VR environment of choosing. Some of the most popular apps for this device are TRIPP, Nature Treks VR, Guided Meditation VR, and Oculus Move.
We have been using a virtual approach for support groups for years due to our large population from rural and mountainous areas and those who come to us from out of state. During the COVID-19 pandemic, we began using Zoom® to allow for easier access to virtual support groups. We now share the recorded videos to our private Facebook group, so that if a patient misses a topic they were anticipating, they can watch it later.
We have a surgeon who is passionate about outreach to our Spanish-speaking population. In order to offer them the same level of support as our English-speaking population, we are exploring the use of Wordly™, a software program that integrates with Zoom® to allow for instantaneous translation through artificial intelligence and closed captioning. This will allow the patient to read the translation of the discussion and interject and ask questions at will with the moderator receiving their verbal communication in their primary language via chat.
Role of Support Services
One of our most memorable patients highlights the importance of patient follow-up and aftercare support. A 54-year-old female patient came to us with congestive heart failure (CHF), gastroesophageal reflux disease (GERD), and hypertension (HTN), with her highest weight at 431 pounds (BMI: 71.7kg/m2). She was able to lose weight by working with her surgeon and RD during her supervised diet phase and weighed in at 294 pounds the day of surgery. She underwent a robotic laparoscopic RYGB to treat her obesity. This patient was on a limited income and had Medicare Disability and Medicaid as a payor source. She did not have a vehicle and had to rely on a nonemergency medical transportation service provided by Medicaid to get to our center. This patient took full advantage of every supportive resource we offer, from weekly support groups, visits with our RD, cooking classes, yoga, weight lifting, and free clothes from our Bari Boutique. She even began to see our behavioral health specialist, whose fees are waived for Medicaid patients. The virtual aftercare options were especially important to her when she suffered the loss of her mother and had to move out of state. Because of our virtual options, she was still able to have the same continuity of care with telehealth visits, Zoom® support groups, and our private Facebook group. Two years after her surgery, she weighs 218.8 pounds (BMI: 35.2kg/m2). Although this patient did not have much support at home, she thrived in our center by taking full advantage of the aftercare program that our center provided.

A Unique Program
In addition to weekly support groups, our center encourages virtual interaction via social media through our private Facebook group, with over 1,500 members, where they can get support any time from members of our team or other patients in the group.
In addition to support groups, our patients can participate in our yoga or weight lifting classes taught by certified trainers and are always welcome to bring a friend. These classes are also free, and our center provides all the equipment.
We also have a beautiful space called the Bari Boutique where our patients can shop for gently used clothes for free as they go through their weight loss journey. These clothes are donated by our patients and employees of our hospital. We found that during the COVID-19 pandemic, our patients struggled to find stores that would allow them to try on clothes, and they were often not comfortable shopping at stores because they didn’t know what size would fit them as they rapidly lost weight. Our center provided them with a safe and private space to shop at their own pace, with a private dressing area created with them in mind. While our patients do not have to donate to shop, many of them do. For some, they want to clean out their closet because they don’t want to go back to larger sizes, so we now have a bin in our parking lot from the Kidney Fund that allows them to donate large quantities of clothes and get a tax donation credit at the same time.
Many times, patients with obesity suffer from depression and anxiety. While seeing our therapist has made a big impact on our patients, our center decided to follow the lead of our Employee Assistance Program and add a therapy dog to our program to sit in with patients during counseling sessions, make rounds with a nurse in the hospital, and greet patients at the support group. Our puppy has completed the beginner’s obedience training and is currently in the advanced off-leash training at Rucker Dog Training Center here in Gainesville. She will complete her American Kennel Club (AKC) Canine Good Citizen certificate by the beginning of the year. Bringing her to the support group completely changes the atmosphere, as you can feel the tension in the room lessen, and patients feel the unconditional love of an animal that accepts them just as they are.
Our center also offers an annual patient celebration event, which includes a bariatric-friendly menu, dancing, and pictures with their favorite surgeon on the red carpet, as they celebrate their transformation together.
New patients come to us through physician referral or self-referral. Patients can get started by watching our online seminar or requesting an appointment through our website at
www.nghs.com/bariatrics or by calling our office at (770)-219-0446.
Reference
- National Center for Complementary and Integrative Health. Meditation and mindfulness: what you need to know. Updated Jun 2022. https://nccih.nih.gov/health/meditation/overview.htm. Accessed 16 Dec 2022.
Interesting Case #1
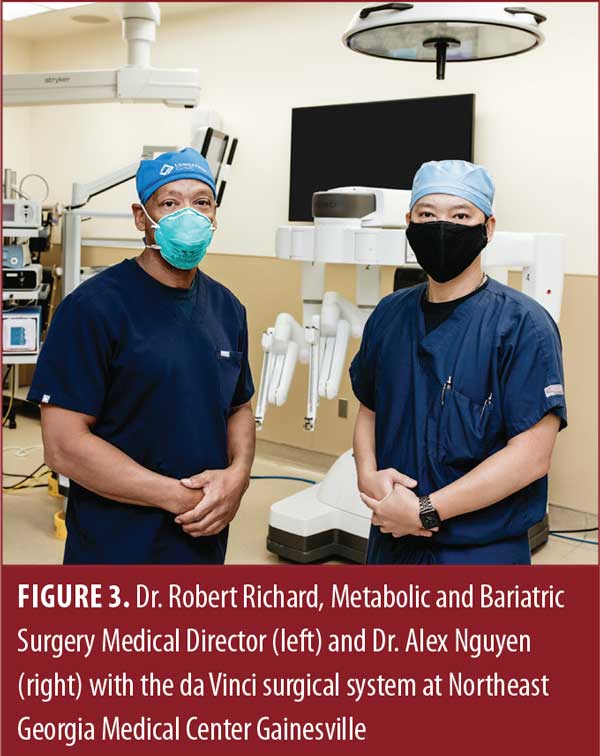
This case concerns a 37-year-old female patient with history of a sleeve gastrectomy performed in Mexico on January 21, 2021. Two weeks later, she presented to an emergency department (ED) with complaints of hematemesis. She denied abdominal pain or nausea. An abdominal and pelvic computed tomography (CT A/P) was performed that revealed evidence of a peritoneal fluid collection adjacent to the stomach.
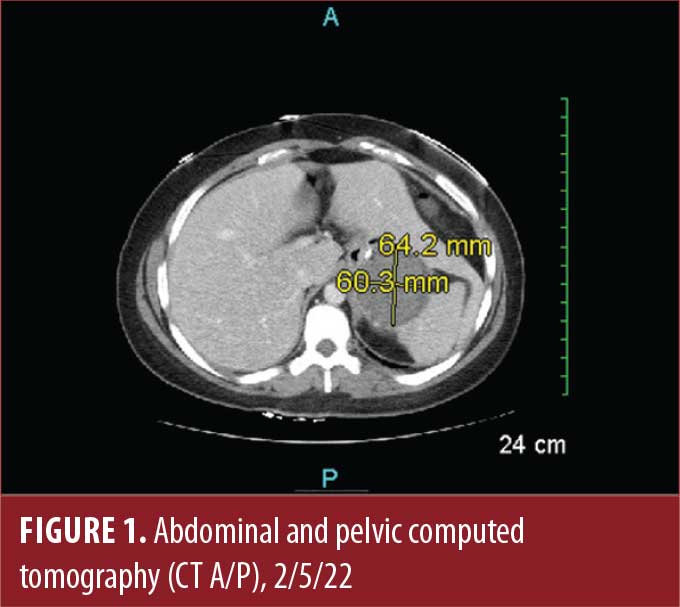
The CT was read as a hematoma. She was treated with intravenous fluids (IVF) and antiemetics and, given her stable hemoglobin and hematrocrit, she was discharged. Seventy-two hours later, she visited the same ED again due to continued hematemesis. This time, a CT A/P was performed with oral contrast. The contrast was identified to be extraluminal going into the perigastric fluid collection.
One of our bariatric surgeons was consulted, and the patient was transferred to our accredited center and admitted under the diagnosis of gastric leak post-sleeve gastrectomy. The patient was placed on nothing by mouth (NPO), and started on IV antibiotics (ABX); a peripherally inserted central catheter (PICC) line was placed, and she was started on total parenteral nutrition (TPN). Interventional radiology (IR) was consulted for percutaneous drainage of peritoneal abscess, but prior to that happening, the patient’s clinical status deteriorated. She developed an acute abdomen with septic shock. She was immediately brought to the operating room for exploratory laparotomy, drainage of peritoneal abscess, peritoneal washout, and placement of feeding jejunostomy tube and drains. Postoperatively, she was kept in the surgical intensive care unit (ICU).
In the following days, she developed another peritoneal collection that required IR drainage. When she became stable and was transferred out of the surgical ICU, an esophagogastroduodenoscopy (EGD) was performed, and two overlapping stents were placed. She complained of severe reflux after stent placement. This was managed with proton pump inhibitor (PPI), sucralfate, and calcium carbonate.

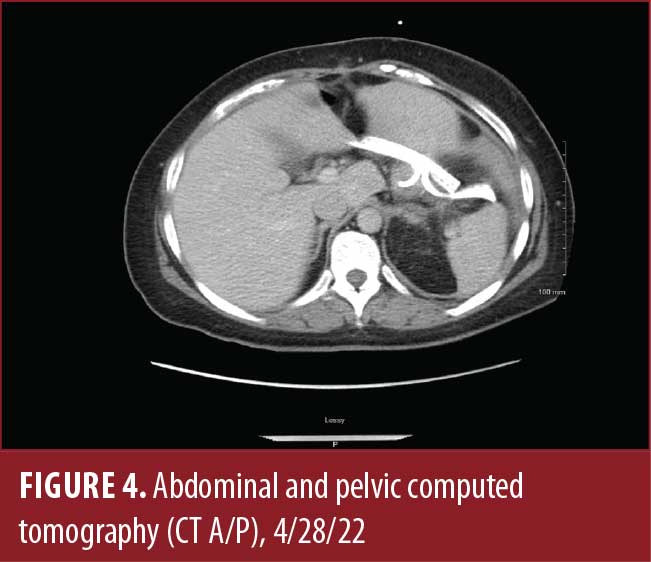
She was hospitalized for six weeks. During this time, she required IR drainage on two more occasions and EGDs for repositioning of migrating stents two more times. After discharge, her stents were removed, and endoscopic placement of a double pig tail catheter was placed via EGD. She was started on a bariatric Stage II diet.
On follow up, a CT A/P with positive oral contrast revealed no evidence of leak. Her drain output had diminished considerably due to the diet. The drains and feeding jejunostomy tube were removed. The patient is currently tolerating bariatric Stage II diet and doing well. She is scheduled to follow up with a gastroenterologist for EGD and removal of double pig tail catheter.
This case highlights:
- The risks of surgical tourism. A great number of patients seeking bariatric surgery travel every year to Mexico, South America, and the Caribbean because of the lower costs. They underestimate the risk of complications and postsurgery management. When weighing their decision, they pay attention only to the transactional cost of the surgery without considering the preoperative education, postoperative care, and long-term commitment to follow ups, which they would get with surgery in the United States (US).
- The importance of multidisciplinary care in the management of the bariatric patient, which is a key aspect of being Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) accredited. The management of this patient required not only a bariatric surgeon, but it involved an interventional gastroenterologist, RDs, an interventional radiologist, case managers, mental health providers, and an infectious disease specialist.
Category: Bariatric Center Spotlight, Past Articles



