Raising the Standard: Northwell Health Bariatric Collaborative: Standardizing Glycemic Control
 by Charmaine V. Gentles, DNP, RNFA; Gustavo Vazquez Zweig, MD; and Dominick Gadaleta, MD, FACS, FASMBS
by Charmaine V. Gentles, DNP, RNFA; Gustavo Vazquez Zweig, MD; and Dominick Gadaleta, MD, FACS, FASMBS
Dr. Gentles is the Program Manager, Bariatric Surgery North Shore University Hospital, Northwell Health, and RNFA Program Coordinator & Supervising Clinical Faculty, Hofstra Northwell School of Graduate Nursing & Physician Assistant Studies in Hempstead, New York, Dr. Zweig is a General Surgery resident at the Zucker School of Medicine at Hofstra/Northwell in New York, New York. Dr. Gadaleta is Chair, Department of Surgery, South Shore University Hospital; Director, Metabolic and Bariatric Surgery, North Shore and South Shore University Hospitals, Northwell Health, Manhasset, New York; Associate Professor of Surgery, Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
Bariatric Times. 2021;18(1):18–19
Defining the Problem
In 2018 in the United States (US), 34.1 million adults (13.0% of all US adults) had diabetes, and it is estimated that of the 1.5 million new cases (6.9 per 1,000 persons) diagnosed, 45.8 percent had obesity (body mass index [BMI]>30kg/m2).1 Current indications for bariatric procedures recommend patients with obesity and diabetes should be offered the surgery.2 When considering operative management in the population described, including bariatric surgery, blood glucose elevation imparts an increased risk in the development of complications. Uncontrolled diabetes affects many aspects of postsurgical recovery due to its effects on microvasculature. These patients have increased incidence of surgical site infections, cardiac events, and total hospital length of stay.3–5 Current guidelines establish preoperative targets of glycated hemoglobin (HbA1c) of at most 6.5 to 7.0 percent for elective surgery and a perioperative glycemic glucose control between 80 and 180mg/dL.6,7
Patients who have undergone bariatric surgery have been noted to have dramatic improvements in their postoperative blood glucose management and HbA1c levels.8–10 Studies have shown that bariatric surgery consistently leads to remission of Type 2 diabetes and achieves this in a cost-effective way, compared to medical therapy alone.8–12 We propose, some patients with diabetes and HbA1c greater than seven percent despite adherence to intensive efforts should be considered for operative management, while recognizing evidence on patients with HbA1c greater than eight percent is poor and needs more investigation.7
We therefore set out to define a subset of patients planning to undergo bariatric surgery with a preoperative blood glucose greater than 180mg/dL the morning of surgery and HbA1c of 8.5 to 9.5 percent within the previous three months despite rigorous attempts at improvement, where metabolic surgery may be permitted to proceed. Indications to cancel surgery include severe dehydration, diabetic ketoacidosis (DKA), and hyperosmolar nonketotic syndrome (HHNS).
Goal
This initiative is intended to standardize the care for all adult patients with concurrent diabetes and morbid obesity undergoing bariatric surgery across all 11 bariatric surgery sites at Northwell Health system. If successfully implemented, we expect to modify and optimize guidelines for the preoperative, perioperative, and postoperative for glycemic control and therefore increase the number of candidates to undergo bariatric procedures and reduce cancellations in a safe manner. The best available evidence supporting benefits of glycemic control in the postoperative period was reported by van den Berghe et al13 in their study of mechanically ventilated patients. Many studies have shown consistent evidence that standardization of clinical processes tends to reliably improve outcomes in the healthcare setting.14,15
Process
During one of the bariatric collaborative meeting in July 2020, members of the committee identified glycemic control as a focal point for potential improvement in patients with obesity and diabetes undergoing metabolic and bariatric surgery. It was discovered that variations in practice exist among the various providers across the 11 centers, in preoperative, perioperative, and postoperative phases of care despite professional societies and health system recommendations. It is cited in the literature that variations exist among professional societies for specific patient population in the clinical setting.1,2
Since glycemic control was identified as a top priority among members of the bariatric collaborative, it was necessary to obtain senior executive and endocrine buy-in prior to undergoing the development of the protocol. Current practice across all medical and surgical specialties in the health system utilize a blood glucose target range of 80 to 140mg/dL. The MBS Director at North Shore University Hospital, his nurse practitioner, and a surgical resident assumed leadership to develop the protocol (See Figure 1). This protocol was designed on the construct and recommendations of the 2020 clinical practice guidelines from the American Diabetes Association (ADA).
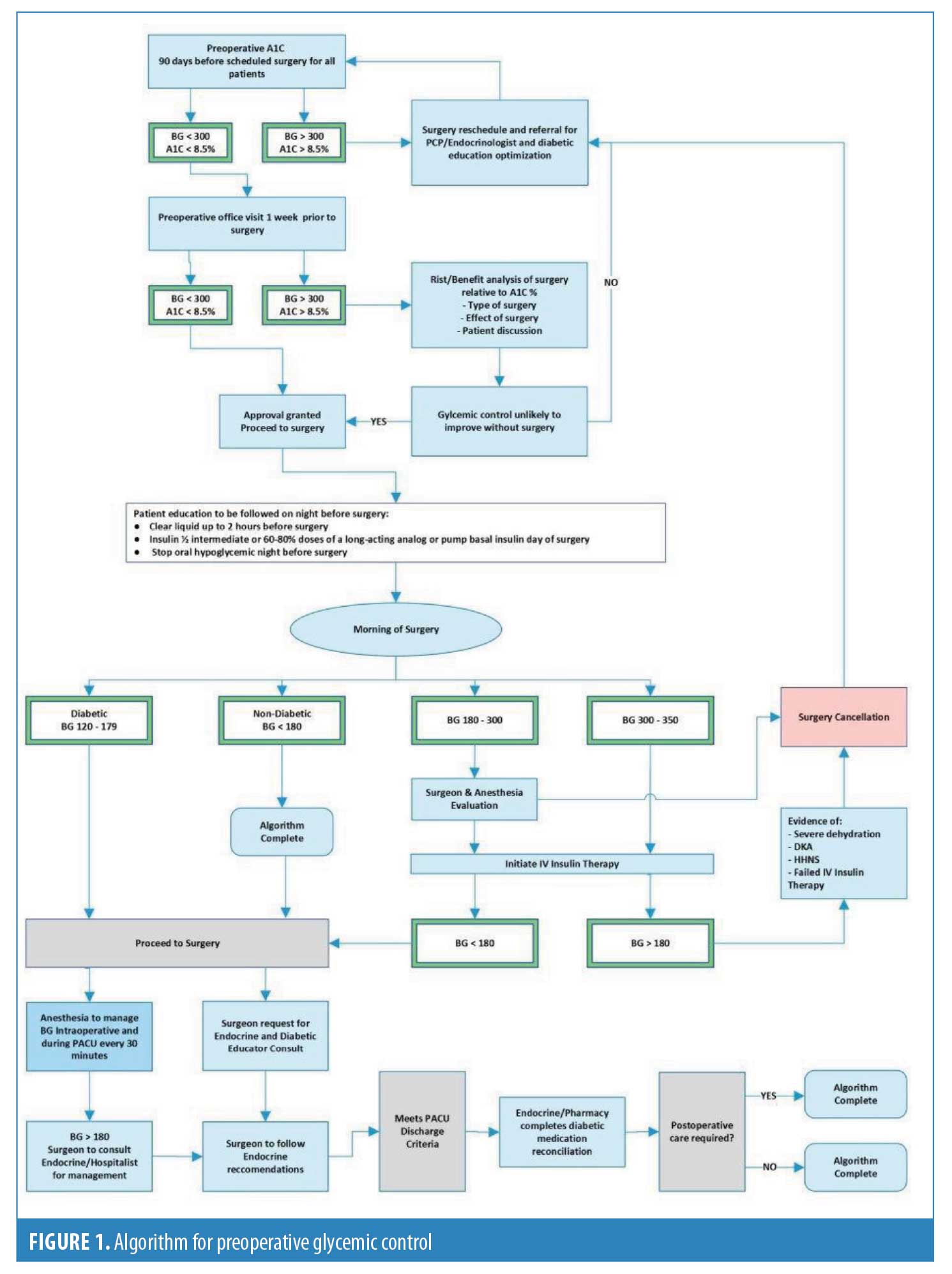
Later in July 2020, the protocol along with a simplified algorithm was developed. The protocol was subsequently reviewed and approved by the endocrinologist and NWH System vice president (VP) of Perioperative Services. The protocol along with the visual diagram was subsequently made available through printed materials and online for discussion at the next collaborative meeting in September 2020. The committee finalized and accepted the glycemic control protocol.
Proposal for Clinical Practice
We propose implementation of the preoperative glycemic control protocol and algorithm as seen in Figure 1 to screen for diabetes as well as improve care of patients with obesity and diabetes throughout all phases of care, consistent with current evidence. The use of clinical pathways and order sets will be utilized to translate these processes into clinical practice. This requires coordinating the providers assessing glycemic control preoperatively on all patients planning to undergo metabolic and bariatric surgery. The process described is outlined as a step-by-step approach for which an easy-to-follow algorithm was developed, as seen in Figure 1. The entire protocol, along with the visual diagram, will be made available through printed material and online to facilitate easy access to the guidelines for all care providers and team members.
Implementation will begin once the patient has met the full criteria for undergoing surgical intervention. Following the proposed protocol, the timeline for evaluation and preoperative preparation would be outlined and explained to the patient and all pertinent scheduling arranged during the same patient encounter for a surgical date at least 90 days in anticipation. Frequent and consistent direct communication with the patient will be maintained during this period to allow for optimization and timeline corrections as needed. Corrective measures would include nutritionist evaluation, endocrine and coordination with the patient’s primary care provider (PCP) for optimization of glycemic control medication, counseling options, and discussions of barriers to improvement.
The key inflection point would arrive during the preoperative visit one week before the scheduled date for surgery. This visit is critical to avoid surgical complications due to incomplete patient preparation, as well as to avoid the administrative issues associated with surgery cancellation. Constant monitoring of the medical, administrative, and operational reasons for operative date changes or deviations from established clinical pathway is essential for the continuous improvement expected from this protocol.
Once the patient is approved to proceed to surgery, the appropriate preparations would be initiated, as well as all postoperative follow up appointments. The rate of cancellation and its justification from the final preoperative visit to the actual operation will be under constant surveillance because this represents the critical time to avoid inefficiency in changes to the operative schedule.
On the surgical date, it is the purpose of this proposal that all members of the healthcare providers in the pre-, peri-, and postoperative teams to be appropriately instructed on the goals of care and awareness of points of contact for addressing any concerns, complications, or deviations from the established protocol.
As outlined in the protocol, patients who do not meet the necessary parameters for surgery based on blood glucose levels or HbA1c may be allowed to proceed with surgery if compliance is confirmed. This will be at the discretion of the surgical and anesthesia teams and will be decided on a case-by-case basis.
During the postoperative follow-up appointments, patients who received surgery despite elevated HbA1c and blood glucose levels will be closely monitored, and results will be reviewed and compared to the results of patients who did meet standard parameters. This process is expected to provide information to better predict outcomes, improve preoperative criteria, and supplement operative justification.
Conclusion
Following implementation, close monitoring of primary and secondary endpoints will allow for continuous quality improvement in aspects of patient safety, improving outcomes, research opportunities and efficiency improvements across all bariatric programs in the health system.
This proposal specifically addresses the justification and monitoring of preoperative glycemic control and allows surgery to proceed in a defined group of patients in need of metabolic surgery, who otherwise might have been denied.
References
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2020.
- Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21 Suppl 1(0 1):S1–S27.
- van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–1367.
- Malone DL, Genuit T, Tracy JK, et al. Surgical site infections: reanalysis of risk factors. J Surg Res. 2002;103(1):89–95.
- Duggan EW, Carlson K, Umpierrez GE. Perioperative hyperglycemia management: an update. Anesthesiology. 2017;126:547–560.
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043–1049.
- Akhtar S, Barash PG, Inzucchi SE. Scientific principles and clinical implications of perioperative glucose regulation and control. Anesth Analg. 2010;110:478–497.
- Mechanick JI, Apovian C, Brethauer S, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric procedures—2019 update. Endocr Pract. 2019;25(12):1346–1359.
- Warren JA, Ewing JA, Hale AL, et al. Cost-effectiveness of bariatric surgery: increasing the economic viability of the most effective treatment for Type II diabetes mellitus. Am Surg. 2015;81(8):807–811.
- Akhtar S, Barash PG, Inzucchi SE. Scientific principles and clinical implications of perioperative glucose regulation and control. Anesth Analg. 2010;110:478–497.
- Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f5934
- Duggan EW, Carlson K, Umpierrez GE. Perioperative hyperglycemia management: an update. Anesthesiology. 2017;126:547–560.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–1367.
- de la Cruz-Muñoz N, Messiah SE, Arheart KL, et al. Bariatric surgery significantly decreases the prevalence of Type 2 diabetes mellitus and pre-diabetes among morbidly obese multiethnic adults: long-term results. J Am Coll Surg. 2011;212(4):505–513.
- Rouse AD, Tripp BL, Shipley S, Pories W, Cunningham P, MacDonald K Jr. Meeting the challenge of managed care through clinical pathways for bariatric surgery. Obes Surg. 1998 Oct;8(5):530-4.
Category: Past Articles, Raising the Standard



