The Increasing Prevalence and Dangerous Association Between Obesity and Atrial Fibrillation
 This activity expired March 1, 2022.
This activity expired March 1, 2022.
Tracy Martinez, RN, BSN, CBN
Ms. Martinez is Department Editor of Integrated Health Continuing Education for Bariatric Times; and Program Director of Wittgrove Bariatric Center in Del Mar, California.
A Message from the Department Editor
Dear Colleagues:
It is with great pleasure to present this month’s continuing education article, titled “The Increasing Prevalence and Dangerous Association Between Obesity and Atrial Fibrillation,” authored by two outstanding nurses. We, as integrated health professionals, have an important responsibility in caring for our patients preoperatively and perioperatively. They are among some of the most medically complex individuals in healthcare today. This article underscores the importance of thorough preoperative medical work-up and reminds us of the multiple health risks our patients face when suffering from severe obesity. I hope you will share this series with all nurses who treat patients with obesity. Please send me your comments and ideas for future articles so we can build a collaborative platform for ongoing education.
My best to you,
Tracy Martinez, RN, BSN, CBN
by Patricia Craft, RN
Ms. Craft is AtriCure Manager, Sales Training and Education in Mason, Ohio.
by Amy Stuck, PhD, RN
Dr. Stuck is Senior Director, Value-based Acute Care and health services researcher at the West Health Institute in La Jolla, California.
Funding: This article is part of a continuing education activity financially supported by AtriCure (Mason, Ohio).
Disclosures: Patricia Craft and Amy Stuck have no conflicts of interest relevant to the content of this article.
Abstract: This article will discuss the role obesity plays in cardiovascular disease—specifically its relationship in the development of atrial fibrillation—and how a combination of obesity-related conditions, such as obstructive sleep apnea (OSA), hypertension, Type 2 diabetes, and metabolic disturbances, have profound consequences on morbidity, mortality, and medical cost to both the patients and the healthcare systems.
Keywords: Obesity, Atrial Fibrillation, cardiovascular disease
Bariatric Times. 2020;17(3):9–12.
Introduction
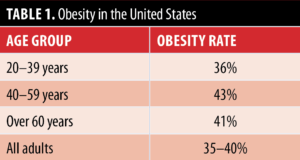
Obesity is a global pandemic. The World Health Organization (WHO) reports that about 13 percent (650 million) of the adult world population is affected by obesity and its related health risks.1 In the United States (US) alone, it is estimated that 35 to 40 percent of the adult population is living with obesity, and the risk of overweight increases with age (Table 1).2,3 Rising obesity rates align with increased incidence of cardiovascular disease (CVD), which is a known obesity-related comorbidity. CVD occurs in 48 percent (121.5 million) of adults and remains the leading cause of death in the US and worldwide.4
The deleterious effects of excess weight on the cardiovascular system are well established, thus obesity remains a significant risk factor for several types of heart and vascular problems, such as hypertension, myocardial ischemia and infarction, heart failure, and cardiac dysrhythmias.5,6 The most common cardiac arrhythmia is atrial fibrillation (AF).7 AF places patients at five times greater risk of stroke. Stroke is the fourth-leading cause of death for women and the fifth-leading cause of death for men in the US.8
AF is an abnormal heart rhythm characterized by the rapid and irregular beating of the atria, or upper chambers of the heart. Approximately one-half percent (33.5 million) of the world’s population are reportedly affected by AF,9 with an estimated 2.7 to 5.1 million cases of AF in the US.10–13 Patients with AF consume a disproportionate amount of healthcare dollars, compared to individuals without AF, and represent approximately 538,000 emergency room visits and 334,000 hospital admissions per year.14 Nationally, healthcare costs associated with AF are between $15.7 and $26 billion, annually.15 While AF is the most common cardiac dysrhythmia among all adults, it is particularly prevalent among adults with obesity, with the risk of developing AF increasing by 4.7 percent for every unit increase in body mass index (BMI).13,16 Given the parallel increases in obesity and AF, collaboration among medical specialties is essential to providing optimal prevention and treatment of patients who have or are at risk of developing both diseases.
Normal heart rhythm is regular, and about 60 to 100 beats per minute (bpm) is considered normal in adults. With AF, there is disruption in the electrical impulse causing the upper chambers of the heart (atria) to beat chaotically and very fast, in the range of 350 to 600bpm. The chaotic impulses in the atria overload the part of the heart’s conduction that allows impulses to enter the bottom chambers of the heart (ventricles) and as a result, the impulses transmit irregularly to the ventricles as well. They can be fast or slow, but they’re almost always irregular.
Arrhythmias are grouped according to the location in which they originate. AF is considered a supraventricular arrhythmia because the rhythm arises above the ventricles in the atria.
The Dangers of Atrial Fibrillation
Strokes related to AF typically occur due to blood clot or thrombus formation in a structure adjacent to the left atrium (the left atrial appendage). Because there is nonmovement, or stasis, of blood in the atria with AF, it is relatively easy for a thrombus to form in this area. If the thrombus dislodges, or embolizes, it can be ejected from the heart. A common place for an embolus to lodge is in an artery that supplies blood to the brain. Ischemia from the lodged embolus can result in a stroke. AF-related strokes result in a fatal outcome more often than in non-AF-related strokes.17 Patients with AF might experience palpitations, light-headedness, chest pain, or shortness of breath. Any or all of these signs and symptoms could lead an individual with AF to seek medical attention. However, AF can occur without any signs or symptoms, yet the patient still remains at risk for stroke, despite being asymptomatic.18
In addition to obesity, there are several other risk factors for developing AF, including the following:
- Coronary artery disease
- Valvular heart disease
- Congestive heart failure
- Family history
- Uncontrolled hypertension
- Advancing age (>65 years)
- Diabetes
- Thyroid disease
- Vascular disease
Many of the above conditions are present in patients with obesity and contribute to a greater cumulative risk of AF. Although many risk factors for AF are nonmodifiable, such as age and family history, obesity is one modifiable risk factor that, if treated, can reduce the risk of developing AF.17
Role of Obesity in Developing AF
Obesity, defined by a BMI greater than 30kg/m2, does not have one single cause but rather is linked to myriad contributing factors. Substantial evidence indicates that obesity is a multifactorial and highly complex disease, comprising a combination of environmental, genetic, behavioral, socioeconomic, and physiological interactions.19
Progressive weight gain is associated with an increase in atrial size, interstitial fibrosis, fat buildup directly on the heart muscle (epicardial fat), reduced conduction speed, and even infiltration of fat into the atrial myocardium (heart muscle).20 These changes can result in atrial remodeling, which increases an individual’s risk of developing AF. AF in individuals with obesity could develop more frequently due to these changes and could be more likely to be sustained.21 Because AF is a progressive disease, without treatment, the AF might be more likely to persist and progress.22
AF Risk Increases with Age
Incidence of both obesity and AF increase with age. Every day over the next decade, 10,000 Americans will reach 65 years of age. Increased age is also associated with changes in metabolic regulation, which can lead to increased adipose tissue, inflammation, and insulin resistance, commonly seen in obesity.23,24 While 25 percent of Americans over the age of 40 years will experience AF sometime in their lives, those over the age of 65 years have an eight-percent incidence, which further increases as age advances.20 Given that the population of elderly (≥65 years) individuals continues to grow, we should expect to see the number of patients who present with obesity and comorbid AF increase, with some predictions indicating this increase will be in epidemic proportions over the next decade.
Obstructive Sleep Apnea
Obesity can be a significant determinant of obstructive sleep apnea (OSA). In turn, OSA can mediate enlargement of the left atrium and lead to AF. Breathing efforts against closed upper airways in patients with OSA can cause constant changes in pressure within the thoracic cavity. These changes create forces on the atrial heart muscle itself. Especially in the area of the posterior aspect of the left atrium, changes in atrial tissue might favor development of AF. Posterior left atrial tissue is thin and especially susceptible to stretching, enlargement, fibrosis, and electrical remodeling, all of which are conditions that can lead to the development of AF.
AF: a Serious, Progressive, and Potentially Fatal Condition
Palpitations is the most common presenting symptom in patients with AF. Importantly, the second-most common presenting symptom of patients with AF is stroke.2,25 In addition to feeling a rapid heartbeat, individuals with obesity and AF can experience the inability to complete activities of daily life, confusion, forgetfulness, shortness of breath, and chest pain. Sometimes patients have no noticeable symptoms at all.18
Dangers of untreated AF. Though AF by itself is typically not life-threatening, if left untreated, it can lead to increased risk of stroke, morbidity, mortality, and sudden death.20 Patients with AF have a greater than five-fold increased risk of stroke, and in one out of 14 events, AF-related strokes result in death.18 The incidence of sudden cardiac death is higher in patients with AF, and AF is strongly associated with incidence of congestive heart failure, a condition in which the heart fails as a muscular pump.7,21 Recently, research indicates that patients with AF have lower scores on cognitive and memory testing, reduced exercise capacity, and an overall lower quality of life.20 With regard to the increase in morbidity and mortality, individuals diagnosed with AF fare worse than those with many invasive cancers when evaluating five-year survivability, which is currently only about 51 percent.26,27 Approximately 15 to 20 percent of all strokes are related to AF.4 AF contributes to heart failure due to the reduction in cardiac output caused by ineffectual atrial contractions that result in a low volume of blood being ejected from the heart (ejection fraction or EF).4 Under normal conditions, adult cardiac output is 4.7 liters of blood per minute [L/min]) When a patient experiences loss of one-quarter to one-third of his or her cardiac output, there are important consequences related to perfusion of the vital organs, leading to multi-organ dysfunction (e.g., kidneys, liver, brain). However, most AF-related strokes and deaths could be prevented by diagnosis of AF and adherence to accepted treatment protocols.
Prevention and Early Treatment
Treatment. In recent years, treatment strategies for AF in individuals with obesity have focused on mitigating its incidence through weight loss, creating an opportunity for specialists in cardiology and obesity to collaborate. A comprehensive, team-based approach should include strategies for improving lifestyle-based risk factors for both heart disease and obesity, such as regular exercise, consuming healthy foods, limiting alcohol, and managing stress. While prevention and treatment strategies focus on modifiable risk factors, medical and surgical treatment can also be beneficial.29
Traditional management of AF consists of anticoagulation for stroke risk reduction, anti- arrhythmic medication to attempt conversion of AF to sinus rhythm, and rate control medicine to maintain resting ventricular rates within a range of 60 to 100bpm. Rate control is an important treatment goal according to the RACE trial, which demonstrated that a rate over 110 in AF is when patients are at greater risk for heart failure.28
Additional treatment strategies include elective cardioversion and ablation therapies, such as endocardial administration via catheter-based approaches, and surgery using a variety of open and minimally invasive approaches, tools, and energy sources. Many physicians feel that now is the time to include lifestyle modification as part of their prescriptions for the prevention and treatment of AF. Since close to 40 percent of American adults have overweight or obesity, it is imperative to increase public awareness on the importance of weight management to avoid cardiac disease, especially AF.
Prevention. Obesity is the leading global modifiable risk factor for AF.20 Although the association between obesity and AF is strong, there is good news for patients who are able to achieve and sustain weight reduction. In 2015, Australian researchers found that individuals with AF with overweight or obesity who demonstrated long-term weight loss experienced significant improvements in AF burden (percent of time spent in AF), AF symptoms, and severity.30 The Long-Term Effect of Goal-directed Weight Management in an Atrial Fibrillation Cohort: A 5 Year Follow-up (LEGACY) study included 355 patients, all of whom received counseling on risk factor management and weight loss. Patients were invited to participate in physician-directed weight management or self-management. Those who lost at least 10 percent of their body weight, regardless of which arm of the study, experienced a six-fold likeliness to remain arrhythmia free without additional rhythm control strategies, compared to patients who either did not lose weight or lost a smaller percentage of weight. Additionally, researchers reported that of the patients who reduced at least 10 percent of their body weight, 84 percent were in the physician-directed weight management arm of the study, compared to the 30 percent of those who experienced less than two percent body weight loss had participated in physician-guided weight management clinics.29 Patients had to keep the weight off to experience the best benefit. Weight fluctuations of more than five percent were associated with twice the risk of AF recurrence compared to patients whose weight fluctuations did not exceed two percent.30
Healthy weight loss can be achieved through one or a combination of the following treatment modalities: behavior modifications (e.g., changes in diet composition, physical activity level), pharmacological intervention with anti-obesity medications, and nonsurgical (e.g., intragastric balloon systems) and surgical (e.g., Roux-en-Y gastric bypass [RYGB], laparoscopic sleeve gastrectomy [LSG]) procedures. Emerging evidence has shown that even modest weight loss (i.e., 5% total body weight) can reverse the type and natural progression of AF.31
Because the risk of AF is higher in individuals with obesity, diabetes, hypercholesterolemia, and hypertension, compared to those without these disorders, research evidence supports that bariatric surgery would reduce the risk. Benotti et al31 conducted a study (of 2,420 patients and matched controls) concluding that patients who underwent RYGB had a significant reduction in CVD risk factors and major cardiovascular events.
Conclusion
Awareness within the medical community of the health risks, prevention strategies, and established treatment modalities for obesity-related AF will be key to preparing for this influx of patients who will be presenting with both diseases. In addition to traditional treatments provided by the multidisciplinary care team, technology such as fitness trackers, smartwatches, and mobile apps can help support healthy behaviors. At the basic level, these allow users to track daily caloric intake, physical activity level, and pulse. More advanced features of wearable devices include single-channel electrocardiogram readings and irregular heart rate notifications, which might help identify AF.
Weight loss to improve health status is at the core of AF prevention. According to the American Heart Association,32 the first line of defense against AF is adopting a “healthy lifestyle,” defined as one that includes regular physical activity, consumption of a heart-healthy diet (i.e., low in salt, saturated fats, trans fats, cholesterol), and maintaining a healthy weight as measured by BMI. Though the message is clear that healthy lifestyle translates to overall improved health status, individual adherence to behavior modification remains a challenge. As the epidemic of obesity and its related comorbidities expands, so too will the incidence of AF. Any means of sustained healthy weight reduction is an effective strategy in reducing the most significant modifiable risk factor for AF.
References
- World Health Organization. Obesity and Overweight Fact Sheet, February 16, 2018. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed January 25, 2020.
- Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief. 2017;(288):1–8.
- Centers for Disease Control and Prevention. Adult Obesity Facts, August 13, 2018. https://www.cdc.gov/obesity/data/adult.html. Accessed January 25, 2020.
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492.
- Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond). 2011;35(7):891–898.
- Hruby A, Manson JE, Qi L, et al. Determinants and consequences of obesity. Am J Public Health. 2016;106(9):1656–1662.
- U.S. Department of Health and Human Services. National Heart, Lung and Blood Institute. Atrial Fibrillation. National Institute of Health, March 2019. https://www.nhlbi.nih.gov/health-topics/atrial-fibrillation. Accessed January 25, 2020.
- U.S. Centers for Disease Control and Prevention. Deaths, percent of total deaths, and death rates for the 15 leading causes of death in 5-year age groups, by race and sex: United States, 2015. https://www.cdc.gov/nchs/data/dvs/LCWK1_2015.pdf. Accessed January 25, 2020.
- Chugh SS, Havmoeller R, Narayanan K. Worldwide epidemiology of atrial fibrillation a global burden of disease 2010 study. Circulation. 2014;25;128:837–847.
- Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114(2):199–125.
- Ohlmeier C, Mikolajczyk R, Haverkamp W, Garbe E. Incidence, prevalence, and antithrombotic management of atrial fibrillation in elderly Germans. Europace. 2013;15:1436–1444.
- Heeringa J, van der Kuip DA, Hofman A, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006;27:949–953.
- Lloyd-Jones DM, Wang TJ, Leip EP, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110:1042–1046
- Rozan G, Hosseini SM, Kaadan MI, et al. Emergency department visits for atrial fibrillation in the United States: trends in admission rates and economic burden from 2007 to 2014. J Am Heart Assoc. 2018;7:e009024.
- Kim MH, Johnston SS, Chu BC, et al. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4:313–320.
- Nalliah CJ, Sanders P, Kottkamp H, Kalman JM. The role of obesity in atrial fibrillation. Eur Heart J. 2016; 37(20):1565–1572.
- U.S. Department of Health and Human Services. National Heart, Lung and Blood Institute. Arrythmias. National Institute of Health. https://www.nhlbi.nih.gov/health-topics/arrhythmia. Accessed February 1, 2019.
- Kaarisalo MM, Immonen-Riaha P, Marrrila RJ, et al. Atrial fibrillation and stroke. Mortality and causes of death after the first acute ischemic stroke. Stroke. 1997;28(2):311–315.
- Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33(7):673–689.
- Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275–e444. Epub 2017 May 12.
- Wang TJ, Parise H, Levy D, et al. Obesity and the risk of new onset atrial fibrillation. JAMA. 2004;292(20):2471–2477.
- Nystrom PK, Carlsson AC, Leander K, et al. Obesity, metabolic syndrome and risk of atrial fibrillation: a Swedish, prospective cohort study. PLOS. 2015;10(5):e0127111.
- National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. Atrial Fibrillation Fact Sheet. https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_atrial_fibrillation.htm. Accessed February 1, 2019.
- Jura M, Kozak LP. Obesity and related consequences to ageing. Age (Dordr). 2016;38(1):23.
- Morillo CA, Banerjee A, Perel P, et al. Atrial fibrillation: the current epidemic. J Geriatr Cardiol. 2017;14(3):195–203.
- Piccini JP, Hammill BG, Sinner MF, et al. Clinical course of atrial fibrillation in older adults: the importance of cardiovascular events beyond stroke. Eur Heart J. 2014;35:250–256.
- Howlader N. Cancer Statistics Review, 1975-2010, National Cancer Institute. Bethesda, MD. http://seer.cancer.gov/csr/1975_2010/. Accessed February 10, 2020.
- van Gelder IC, Hagens VE, Bosker HA, et al. Rate control versus electrical cardioversion for atrial fibrillation. A randomized comparison of two treatment strategies concerning morbidity, mortality, quality of life and cost-benefit – the RACE study design. Neth Heart J. 2002;10(3):118–124.
- Pathak, RK, Middeldorp ME, Meridith M. Long-term effect of goal-directed weight management in an atrial fibrillation cohort: a long-term follow-up study (LEGACY). J Am Coll Cardiol. 2015;65(20):2159–2169.
- Middeldorp ME, Pathak RK, Meredith M, et al. Prevention and regressive effect of weight-loss and risk factor modification on atrial fibrillation: the REVERSE-AF study. EP Europace. 2018;20(12):1929–1935.
- Benotti PN, Wood GC, Carey DJ, et al. Gastric bypass surgery produces a durable reduction in cardiovascular disease risk factors and reduces the long‐term risks of congestive heart failure. J Am Heart Assoc. 2017;6(5). pii: e005126.
- American Heart Association https://www.heart.org/en/health-topics/atrial-fibrillation/treatment-and-prevention-of-atrial-fibrillation/prevention-strategies-for-atrial-fibrillation-afib-or-af. Updated July 31, 2016. Accessed February 25, 2020.
Category: Past Articles, Review




