Robotic-assisted Laparoscopic Revision of Roux-en-Y Gastric Bypass for Recurrent Gastrogastric Fistula

by Carolyn G. Judge, MD; Kyle D. Gadbois, MD, FACS; and Gordon G. Wisbach, MD, MBA, FACS, FASMBS
Lt. Judge is with Navy Medical Research Center in Silver Spring, Maryland. CDR. Gadbois is with Navy Readiness and Training Command in San Diego, California. Capt. Wisbach is Professor of Surgery, Uniformed Services University in Bethesda, Maryland.
Funding: No funding was provided for this article.
Disclosures: Capt. Wisbach is a consultant for Intuitive Surgical. The remaining authors have no conflicts of interest relevant to this article.
Correspondence: Carolyn G. Judge, MD; Email: carolyngjudge1990@gmail.com
Bariatric Times. 2023;20(7–8). Published online July 27, 2023.
Abstract
A gastrogastric fistula (GGF) is an abnormal connection between the gastric pouch and gastric remnant. This complication is rare following Roux-en-Y gastric bypass (RYGB), but it can have grave consequences, requiring revisional surgery. Symptoms most commonly include weight recidivism, gastroesophageal reflux disease (GERD), and upper abdominal pain. Initial treatment is nonoperative; however, surgical repair may be indicated if the fistula is symptomatic, large, or complex. We present the case of a 40-year-old woman with a remote history of open RYGB for morbid obesity complicated by recurrent GGFs. Her first fistula was diagnosed 20 years after her index operation and repaired shortly thereafter. She developed recurrent postprandial epigastric pain and GERD consistent with her initial fistula four months after repair. Upper gastrointestinal contrast study (UGI) and computed tomography (CT) evaluation at that time demonstrated a recurrent GGF. A robotic-assisted, laparoscopic revision of RYGB with en bloc resection of the recurrent GGF was successfully performed, demonstrating the safety and efficacy of robotic surgery in complex revisional bariatric procedures.
Keywords: Gastrogastric fistula, gastrojejunalgastric fistula, gastric bypass, robotic revisional surgery, bariatric surgery
Gastrogastric fistula (GGF) is defined as an abnormal connection between the gastric pouch and gastric remnant, historically associated with staple-line failure in the setting of the undivided Roux-en-Y gastric bypass (RYGB).1,2 Nonoperative therapy can be effective, but large and complex fistulas often require revisional surgery.1,3 The nature of the operation is determined by the location and characteristics of the fistula, and is most commonly either a remnant gastrectomy with redo gastrojejunal anastomosis (GJA) or fistula excision in isolation.1
Rates of bariatric surgery and, in turn, revisional bariatric surgery (RBS) are increasing.2,4 RBS has been successful in treating complications and achieving continued weight loss, but it is known to have higher morbidity than index procedures.2 The robotic platform has been shown to be safe and effective in complex RBS, including in the management of GGF.4
Case Report
We present the case of a 40-year-old woman with a remote history of open RYGB in 2001 for morbid obesity, complicated by recurrent GGF. Her primary fistula was diagnosed and repaired in January 2020, 20 years after her index operation. She represented 14 months later, endorsing chronic epigastric pain and gastroesophageal reflux disease (GERD). Computed tomography (CT) and upper gastrointestinal (UGI) evaluation performed at that time demonstrated a recurrent GGF from the posterior aspect of the gastric pouch, extending to the anterosuperior segment of the remnant stomach (Figure 1). Of note, the patient was compliant with appropriate proton pump inhibitor (PPI) therapy, was not smoking, and did not have evidence of Helicobacter pylori (H. pylori) infection. Given the persistent symptoms refractory to medical management in the setting of a known, recurrent GGF, the patient underwent robotic-assisted laparoscopic revisional RYGB.

On entry into the abdomen, no injury was noted. Omental adhesions were reduced from the anterior abdominal wall at the site of the prior incision. Additional adhesions were noted as dissection proceeded medially between the gastric pouch and the left lobe of the liver. The procedure was performed using a total of five ports, including three 8mm ports placed in the left subcostal and periumbilical areas, as well as the right lower quadrant in the anterior axillary line. The fourth 8mm port, placed in the right lower quadrant midclavicular line, was upsized to 12mm. The fifth and final port was placed at the subxiphoid area, through which the Nathanson retractor was placed.
Tilepro (Intuitive Surgical; Sunnyvale, California) is a multi-input display software that is used to provide simultaneous visualization of robotic and endoscopic views during complex gastrointestinal operations. This technology was used, in conjunction with Firefly technology (Intuitive Surgical; Sunnyvale, California), to visualize endoscopic passage into the gastric pouch, through the GJA and into the roux limb (Figure 2). It also clearly demonstrated the known, large fistula from the posterior aspect of the roux limb, immediately past the normal GJA, to the remnant stomach.

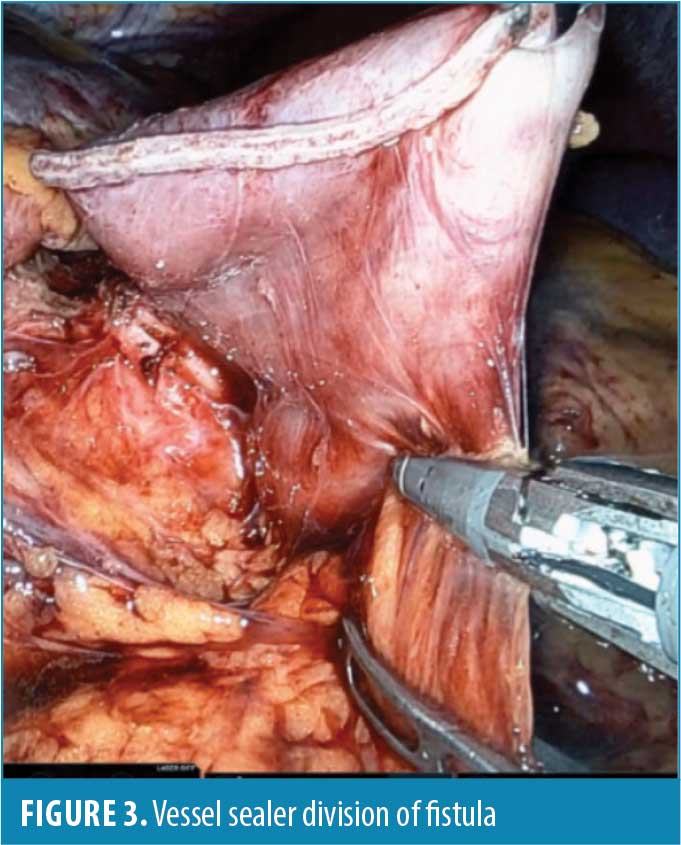
Once the anatomy was fully visualized, the roux limb was divided distal to the anastomosis, followed by division of the fistula. An advanced bipolar vessel sealing device was used, which delivered both pressure and energy to coagulate and divide the mesentery, creating a seal using only the patient’s own tissue (Figure 3). Using a combination of blunt and electrocautery, the old anastomosis and fistula were then removed from the surface of the remnant stomach.
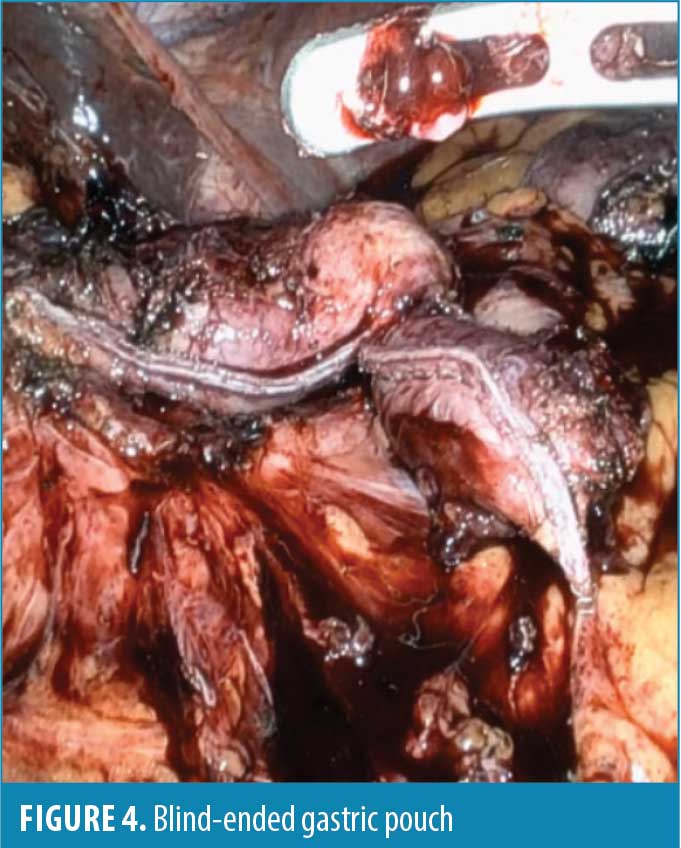
The green 60mm robotic endostapler was used to divide the gastric pouch proximal to the old GJA and GJ fistula, thereby creating a blind-ended gastric pouch and excluding the two openings, which were inspected endoscopically (Figure 4). The resultant remnant stomach gastrostomy was then repaired with a two-layered, hand-sewn closure using two 3-0 V-loc suture. Once the remnant stomach repair was complete, a new GJA was created in two layers, using a hand-sewn 3-0 absorbable V-loc suture. The V-loc barbed suture creates a strong anchor using a unique dual-angle cut and barbing pattern. It has been shown to reduce suture time and evenly distribute tension along the wound. It also eliminates the need to tie a knot and therefore the risk of knot-related complications.
A leak test was performed with clamping of the roux limb to allow for endoscopic inspection under intraperitoneal saline submersion without evidence of leak. There were no complications, and the patient went on to have complete resolution of her symptoms.
Discussion
A low threshold for comprehensive evaluation, including UGI, CT, and esophagogastroduodenoscopy (EGD) should be employed in symptomatic postoperative bariatric patients.5 GGF may present with weight recidivism and pain or vague symptoms, such as nausea, emesis, and dysphagia.1
Conservative treatment is recommended for asymptomatic patients.1 The goal is to reduce gastric acid secretion to allow small fistulas to close spontaneously.3 Treatment consists of H. pylori eradication, if present, as well as sucralfate and high dose PPI therapy and nonsteroidal anti-inflammatory drug (NSAID) and smoking cessation.3,6 Gumbs et al3 observed a 20-percent success rate of conservative management in their patients with small caliber fistulas. Endoscopic repair can be attempted but is largely dependent on the size of the fistula and has been associated with failure rates up to 81 percent, despite high success in initial closure.6
RBS is often more technically challenging than the index operation due to scarring, adhesions, and inflammation.2 This might make dissection around the angle of His, in particular, especially difficult and increase the risk for residual posterior stomach.7 Larger pouches due to inadequate dissection and incomplete division may predispose to GGF due to the retention of greater amounts of fundal cells and the associated increased acid production.8 RBS is also associated with increased rates of postoperative adverse events, such as leaks, readmissions, and reoperations, compared to primary bariatric surgery.2 Nevertheless, RBS is indicated for pain, ulcers, and weight regain refractory to medical management,5 and correction of GGF is associated with weight loss, satiety, and normalization of orexigenic gut hormones.1,9
The most commonly described operative interventions include remnant gastrectomy with fistula excision,5,8,10 with or without revisional GJA.8 The operation of choice may be guided by surgeon preference, with anastomotic revision favored in the setting of weight regain, enlarged pouch, GJ stenosis, or intractable ulcers.8 Chahine et al1 describe two types of GGF: high GGF ( >1cm above GJA), and low gastrojejunalgastric fistula (<1cm from GJA). The high GGF can be excised by reinforced stapling at either end of the fistula, with preservation of the GJA, followed by tissue interposition to maintain separation of the pouch and remnant.1,3,11 The low fistula, commonly associated with marginal ulceration or anastomotic stenosis, may require an en bloc resection of the GJ, followed by side-to-side redo GJ and gastrostomy closure.1,8
The robotic platform is safe and effective in complex revisional bariatric procedures.4 Previous studies have demonstrated fewer leaks with robotic versus laparoscopic anastomosis in index procedures.12,13 In a retrospective review of robotic RBS, Cheng et al4 demonstrated zero anastomotic leaks, which they credit to enhanced suture quality due to the increased dexterity and range of motion of the robot. Increased operative time has been observed with robotic surgery, likely due to docking time, instrument changing, learning curve, and unfamiliarity of the operating room staff with the platform.14 Operative time is an independent predictor of increased morbidity in bariatric surgery, but it has been shown to resolve with time, suggesting there is a learning curve associated with robotic surgery.15
Conclusion
GGFs are rare complications of RYGB. Their pathophysiology is unknown, but there are strong correlations with staple-line failure, marginal ulcers, and leaks. All patients presenting with vague symptoms, and especially those with pain and weight recidivism, should be evaluated by CT, UGI, and EGD. Large and complex fistulas might not respond to conservative management, thus requiring operative intervention. The robotic platform is safe and effective in the management of GGF and should be considered in complex RBS.
References
- Chahine E, Kassir R, Dirani M, et al. Surgical management of gastrogastric fistula after Roux-en-Y gastric bypass: 10-year experience. Obes Surg. 2018;28(4):939–944.
- Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis. 2014;10(5):952–972.
- Gumbs AA, Duffy AJ, Bell RL. Management of gastrogastric fistula after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2006;2(2):117–121.
- Cheng YL, Elli EF. Role of robotic surgery in complex revisional bariatric procedures. Obes Surg. 2021;31(6):2583–2589.
- Carrodeguas L, Szomstein S, Soto F, et al. Management of gastrogastric fistulas after divided Roux-en-Y gastric bypass surgery for morbid obesity: analysis of 1,292 consecutive patients and review of literature. Surg Obes Relat Dis. 2005;1(5):467–474.
- Fernandez-Esparrach G, Lautz DB, Thompson CC. Endoscopic repair of gastrogastric fistula after Roux-en-Y gastric bypass: a less-invasive approach. Surg Obes Relat Dis. 2010;6(3):282–288.
- Filho AJ, Kondo W, Nassif LS, et al. Gastrogastric fistula: a possible complication of Roux-en-Y gastric bypass. JSLS. 2006;10(3):326–331.
- Corcelles R, Jamal MH, Daigle CR, et al. Surgical management of gastrogastric fistula. Surg Obes Relat Dis. 2015;11(6):1227–1232.
- O’Brien CS, Wang G, McGinty J, et al. Effects of gastrogastric fistula repair on weight loss and gut hormone levels. Obes Surg. 2013;23(8):1294–1301.
- Cho M, Kaidar-Person O, Szomstein S, Rosenthal RJ. Laparoscopic remnant gastrectomy: a novel approach to gastrogastric fistula after Roux-en-Y gastric bypass for morbid obesity. J Am Coll Surg. 2007;204(4):617–624.
- Capella JF, Capella RF. Gastro-gastric fistulas and marginal ulcers in gastric bypass procedures for weight reduction. Obes Surg. 1999;9(1):22–27; discussion 28.
- Hagen ME, Pugin F, Chassot G, et al. Reducing cost of surgery by avoiding complications: the model of robotic Roux-en-Y gastric bypass. Obes Surg. 2012;22(1):52–61.
- Economopoulos KP, Theocharidis V, McKenzie TJ, et al. Robotic vs. laparoscopic Roux-En-Y gastric bypass: a systematic review and meta-analysis. Obes Surg. 2015;25(11):2180–2189.
- Buchs NC, Pugin F, Azagury DE, et al. Robotic revisional bariatric surgery: a comparative study with laparoscopic and open surgery. Int J Med Robot. 2014;10(2):213–217.
- Buchs NC, Morel P, Azagury DE, et al. Laparoscopic versus robotic Roux-en-Y gastric bypass: lessons and long-term follow-up learned from a large prospective monocentric study. Obes Surg. 2014;24(12):2031–2039.
Category: Case Report, Current Issue




