A Survey on Scope of Practice Among Members of the American Society for Metabolic and Bariatric Surgery

by Abdulaziz A. Arishi, MD; Jean F. Salem, MD; Pavel Burskii, MD; Jill Stoltzfus, PhD; Anthony T. Petrick, MD; Ranjan Sudan, MD; and Maher El Chaar, MD
Drs. Arishi, Salem, Burskii, Stoltzfus, and El Chaar are with the Department of Surgery, St. Luke’s University Hospital and Health Network, Lewis Katz School of Medicine in Bethlehem, Pennsylvania. Dr. Arishi is also with Department of Surgery, Faculty of Medicine, Jazan University in Jazan, Saudi Arabia. Dr. Petrick is with the Department of Surgery, Geisinger Health System in Danville, Pennsylvania. Dr. Sudan is with Department of Surgery, Duke University Medical Center in Durham, North Carolina.
Funding: No funding was provided for this article.
Disclosures: Dr. El Chaar is faculty for Intuitive Surgical. All other authors have no conflicts of interest relevant to the contents of this article.
Bariatric Times. 2023;20(5–6):10–14.
Abstract
Background: The General Surgery and Foregut Committee of the American Society for Metabolic and Bariatric Surgery (ASMBS), established in 2016, aimed to identify the unique diagnostic and treatment strategies required in the management of general surgery and foregut diseases in patients undergoing metabolic and bariatric surgery. To achieve this, the committee believed that more data regarding the scope of practice among ASMBS members was needed.
Objective: The current study aimed to survey ASMBS members using a standardized survey to assess essential elements of practice in the fields of bariatric, foregut, and general surgery.
Methods: A subcommittee was formed to develop the survey. Questions focused on demographics and the scope and volume of members’ bariatric, foregut, and general surgical practices. The subcommittee developed and refined the survey, which was then reviewed and approved by the executive committee. In early 2019, surveys containing items on demographic information, members’ specializations and accreditations, areas and levels of expertise, volume of procedures, involvement in postgraduate education, and call coverage details were emailed to 1,778 ASMBS members.
Results: The response rate was 31.7 percent. Among the 564 ASMBS members who responded, the majority (88%) practiced in cities or suburban areas. Half of the members had performed bariatric surgery for a period of 11 to 20 years. Just over 64 percent of members had completed fellowship training, with 81 percent of these surgeons having specialized in minimally invasive and bariatric surgery. About two-thirds of survey participants (65%) devoted more than half their practice to bariatric surgery, and over half of respondents (52%) were hospital employees.
Conclusion: The ASMBS member survey was well received, with nearly one-third of members responding. Members are specialty trained; perform a wide range of bariatric, foregut, and general surgical procedures; and are highly concentrated in urban and suburban areas. The survey results are a representation of contemporary practice patterns of bariatric surgeons and set a baseline for comparison of future practice trends. They can also inform the society on developing strategies and guidelines that are meaningful to our membership based on their existing practice patterns.
Keywords: Scope of practice, survey, bariatrics, surgery, hospitals, descriptive analysis
Bariatric surgeons across the United States (US) have seen a rapid change in scope of practice, especially with new developments in technology and the emergence of new medical treatments and surgical options, providing a higher quality of care.1
In light of this reality, the American Society for Metabolic and Bariatric Surgery (ASMBS) was established with three primary mission objectives: 1) to improve the care and treatment of individuals with obesity, 2) to advance the science and understanding of metabolic and bariatric surgery, and 3) to be a highly valued specialty society that addresses the professional educational needs of its diverse membership. The Foregut and General Surgery Committee was established in 2016 with the aim of developing and disseminating evidence-based guidelines that identified unique diagnostic and treatment strategies required to manage general surgical and foregut diseases in patients undergoing metabolic and bariatric surgical procedures.2 To achieve this goal, the committee understood the need for assessing its members’ scopes of practice, leading to development of a subcommittee that created the scope of practice survey.3 The survey included questions regarding demographics and members’ scopes of practice in bariatric, foregut, and general surgery. Understanding other practice areas, including endoscopic procedures and call obligations, was also a focus of the survey. The survey was reviewed and refined by the executive committee prior to approval. It was distributed to the ASMBS membership via email in 2019.
Our study objectives were to analyze the survey results to better understand ASMBS members’ practices regarding bariatric, foregut, and general surgical procedures performed, as well as their perspectives, roles, and involvement in postgraduate training and call coverage.4
Methods
Survey development and distribution. The General Surgery and Foregut Subcommittee conducted a survey study on member scope of practice in 2019. The seven-minute questionnaire was assessed for practicability and quality and was approved by the executive committee in 2018. The majority of the questions were closed-ended, wherein respondents were asked to select either a single choice or “all that applied” from predefined choices. Some questions included the response “other (please specify)” and permitted free text answers. Categories that were surveyed included years in practice; on-call coverage; time spent in general, foregut, and bariatric surgery fields; and volume of different procedures
The web-based survey was released in 2019. Individual survey links were electronically distributed to 1,778 active members by email. Reminders were distributed every week for a total of four weeks. Respondents were not required to answer all questions. There was a four-week data collection period, which was closed on February 8, 2019.
Data analysis. Our analysis included currently practicing members of the ASMBS, with confidentiality of responses maintained. Given the nature of the survey, we reported descriptive statistics with frequencies and percentages for all responses. We categorized questions addressing the amount of performed procedures as 100 or more cases for each procedure. We categorized questions addressing the amount of time spent in specialty areas as 50 percent or more of the time for each area. We analyzed our data using Microsoft Excel and SPSS version 27 (IBM Corp.; Armonk, NY).
Results
Among the 1,778 members who received the survey, 564 (31.7%) returned the survey over the course of four weeks. Most of the responses were obtained over the first two weeks. Respondents were not required to answer all questions, and incomplete responses were counted on the analysis.
Demographic characteristics. Participants had a median age of 49.7 years (range: 33–78 years). Most participants were younger than 56 years (71.4%) and male (84.9%). Moreover, 83.6 percent of respondents were practicing within the US. The largest proportion of respondents supplying a zip code were from the Southern US (26.7%).
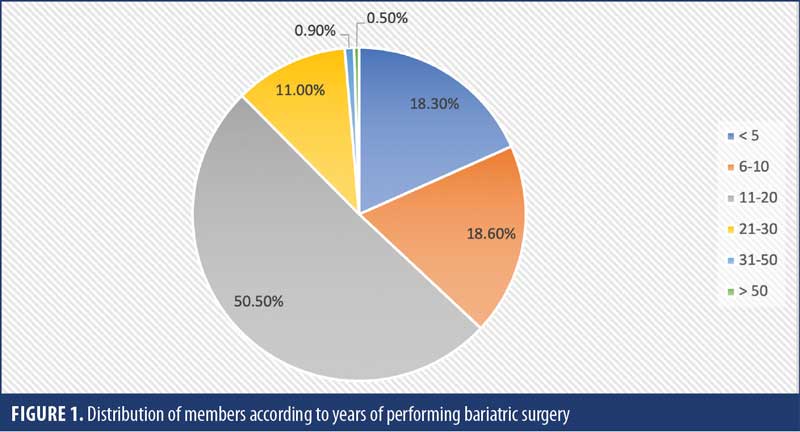
Practice characteristics. Two-thirds of respondents practiced in community (nonteaching) hospitals, and only about 10 percent practiced in hospitals with less than 100 beds. Only 12 percent of the participants practiced in rural areas, while over half practiced in urban areas. In addition, 52.2 percent of the participants were hospital/health system employees (private/university) (Table 1). Approximately one-third of the respondents (38.7%) had been in clinical practice for 11 to 20 years and, 38 percent had less than 10 years of practice experience. Over half of respondents (50.5%) had been performing bariatric surgery procedures for 11 to 20 years (Figure 1).
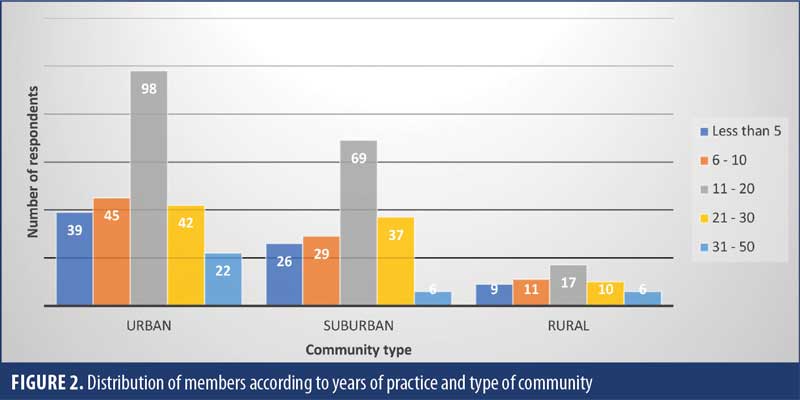
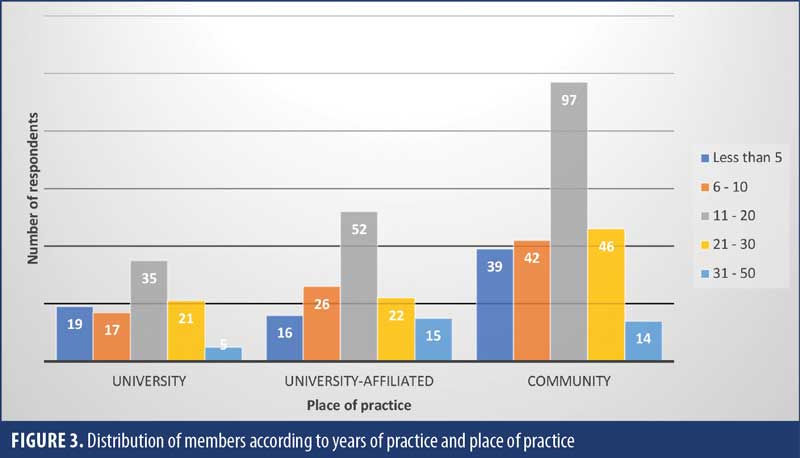
After comparing the distribution of members according to community type, years of experience, and place of practice, our results showed that the majority of members were concentrated in urban and suburban areas (Figure 2) and practiced in community hospitals, with varying years of experience (Figure 3).
Our results showed that about two-thirds of the participants had completed fellowship training. There was no apparent association between completion of fellowship training and location or type of practice. The majority of fellowship-trained respondents indicated that their program had Fellowship Council accreditation or predated training.6 Our findings showed that about nearly three times as many respondents (41%) reported performing 100 or more laparoscopic sleeve gastrectomies (SGs) annually as respondents reporting performing over 100 laparoscopic Roux-en-Y gastric bypasses (RYGBs) annually (15%). Less than one percent of respondents indicated that they performed 100 or more laparoscopic biliopancreatic diversion/duodenal switch procedures (0.6%) or endoscopic bariatric procedures (e.g., intragastric balloon and gastric plication; 0.8%) annually.
Scope of teaching. More than half of the respondents (n=301/557, 54%) taught surgical residents, whereas only 136 out of 557 (24.4%) taught minimally invasive surgery (MIS) and bariatric surgical fellows. Most providers involved in postgraduate education practiced as hospital/health system employees (private/university) and had received fellowship training.
Role of endoscopy. After exploring the endoscopic practice of ASMBS members, our results showed that 428 out of 495 (86.5%) performed routine endoscopies, 264 out of 359 (73.6%) performed bariatric endoscopies, and only 153 out of 487 (31.4%) performed colonoscopies. Despite the widespread practice of endoscopy, only 2.7 percent of respondents reported training in advanced endoscopy. Table 2 summarizes the endoscopy interventions and annual case numbers.
Gastroparesis treatment. Participants were asked what procedures they performed for gastroparesis treatment. A little less than half of all respondents, (n=252, 44.7%) performed surgical procedures specifically for the treatment of gastroparesis. Of those who treated gastroparesis, RYGB without gastrectomy was the procedure most used by respondents (77.4%). About half of respondents would consider using SG (52.4%) or RYGB with gastrectomy (50.8%). Pyloroplasty was used by 61.5 percent of respondents and Botox by 17.5 percent, and 19 percent of respondents reported placing gastric stimulators for gastroparesis.
General surgery practice and call coverage. The survey asked about the general surgery practice experience of ASMBS members. About 26 percent of members performed 100 or more procedures annually to treat gallbladder/biliary disease. About half (50.7%) indicated that they performed laparoscopic common bile duct (CBD) surgeries. When asked about their preferred method for managing CBD stones after RYGB, 82.3 percent preferred laparoscopic remnant gastrostomy and endoscopic retrograde cholangiopancreatography (ERCP), while 17.7 percent of the respondents preferred surgical CBD exploration. Only 7.5 percent of ASMBS members reported performing 100 or more abdominal wall hernia repairs annually, with about twice as many members (13.5%) performing 100 or more inguinal hernia repairs.
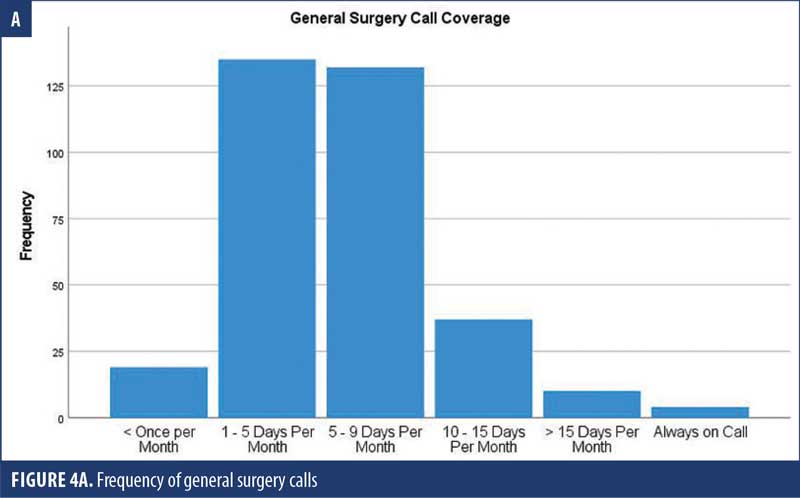
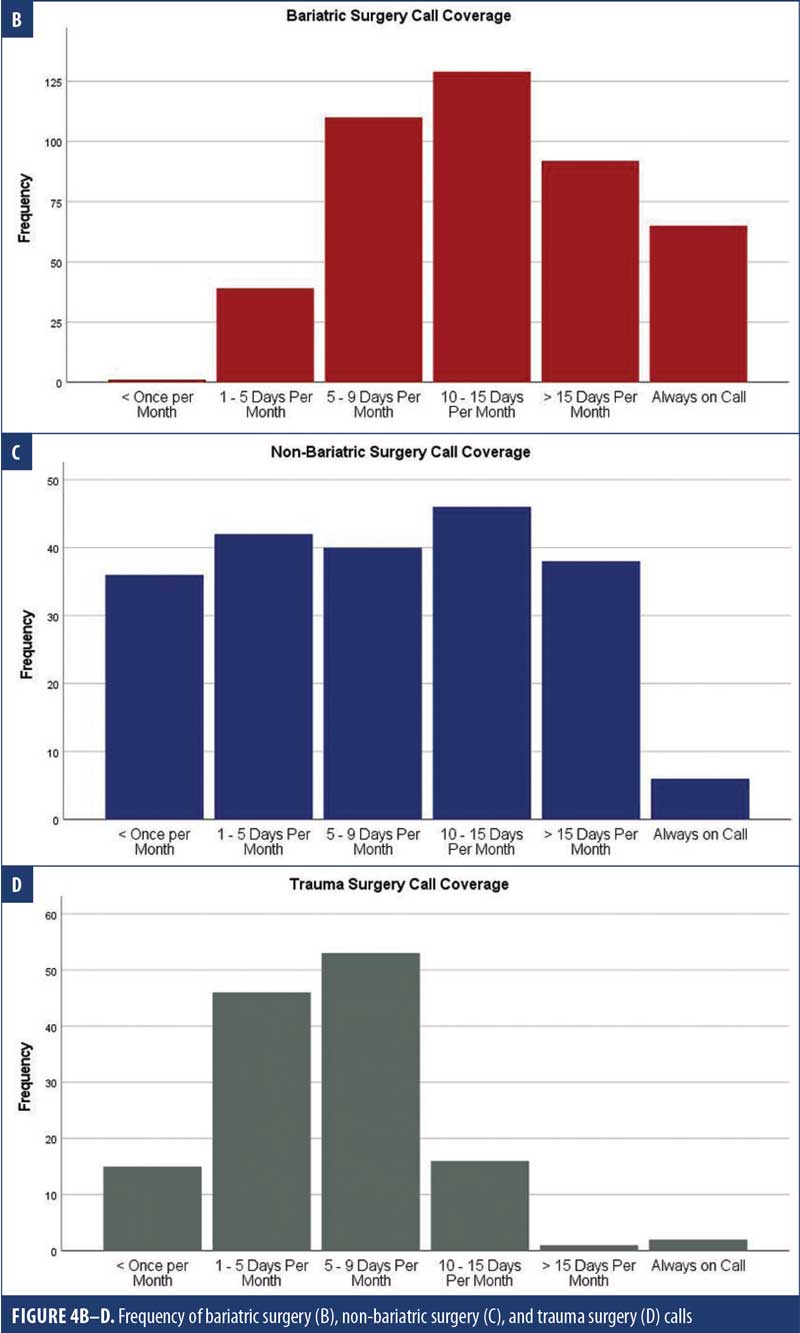
More than two-thirds of respondents (70.6%) were responsible for general surgery call coverage, and about one-quarter took trauma call. Nearly all respondents provided bariatric specialty coverage; however, 39.2 percent indicated that nonbariatric surgeons covered bariatric specialty calls during practice (Figure 4).
Discussion
The current study aimed to survey ASMBS members using a standardized questionnaire to assess essential elements of practice in the fields of bariatric, foregut, and general surgery. The response rate of 31.7 percent provides a glimpse of ASMBS members’ scopes of practice, which can be helpful for fellows looking to start a practice or join an existing practice. Only 15.1 percent of the respondents were female, whereas estimates show that 12 percent of general surgeons are female.5 Additional efforts aimed at increasing diversity and recruiting more female residents into bariatric and MIS fellowship programs are still needed. After comparing female and male surgeons with similar characteristics who treated similar patients at the same hospital, Sharoky et al6 found similar postoperative outcomes, mortality rates, and length of hospital stay between both groups.
Among the participants included herein, only 9.7 percent were younger than 40 years of age. Although this could have been due to younger members’ lack of interest in survey participation, it is possible that this could actually reflect the true percentage. As such, efforts geared toward encouraging new and younger surgeons to become members of the ASMBS and participate in committees are needed. Moreover, committees aimed at attracting new bariatric fellows and led by younger surgeons could potentially be established to help improve participation in ASMBS activities.
According to the Centers for Disease Control and Prevention (CDC) reports for 2019, the Midwestern and Southern US had the highest prevalence of obesity (33.9% and 33.3%, respectively), followed by the Northeastern and Western US (29% and 27.4%, respectively).7 This data could explain the predominant distribution of ASMBS members in the South seen in our study (n=119, 26.7%).
Only 32 percent of members practiced in university-affiliated hospitals, which might explain the low number of members involved in teaching MIS/bariatric fellows (24.4%). With more SGs being performed nationally and internationally, compared to gastric bypasses, only 15 percent of participants reported performing over 100 laparoscopic RYGBs each year. This might explain a growing fear among new fellows of not satisfying ASMBS fellowship certification requirements, especially during the COVID-19 pandemic.
Wen et al,8 who studied the disparities in obesity prevalence between urban and rural areas, found a higher prevalence of obesity in rural areas (41%), compared to urban areas (32%). This might explain, in part, the low number of surgeons practicing in rural areas found in our study.8 Other factors could be infrastructure and case volume requirements that might be harder for rural centers to achieve.
One important objective of the current survey was to uncover trends in the treatment of foregut disorders. According to our study, most ASMBS members practiced other advanced laparoscopic procedures, such as CBD exploration, and provided ERCP to treat CBD stones. Another common area of practice was inguinal hernias. Many bariatric surgeons also provided RYGB or SG as treatment options for gastroparesis. The majority of bariatric surgeons actively practiced endoscopy, though a very small number had training in advanced endoscopy. Our study also showed that many ASMBS members (70.6%) provided coverage for general surgery.
Moreover, with the recent COVID-19 pandemic, a relative increase in general surgery procedures performed by the participants can be expected, given the decreased volume of bariatric cases, which could continue for the next few years.9 Furthermore, with the increase in the number of fellowship-trained bariatric surgeons, bariatric surgeons might be required to provide more general surgery coverage and perform general surgery procedures, in addition to bariatric procedures. Also, among the surveyed members, 39.2 percent reported that nonbariatric surgeons covered bariatric calls. Therefore, nonbariatric surgeons should be familiar with the diagnoses and management of acute bariatric emergencies.
Limitations. The current study has limitations worth noting. First, this was a descriptive study with a low response rate, and the incomplete responses were counted on analysis. Second, some of the questions were open-ended and difficult to analyze. Third, given that our study focused on assessing essential elements of practice in the fields of bariatric, foregut, and general surgery, we did not investigate the bariatric volumes of the participants to see if there was any correlation between volume and general surgery scope of practice.
Conclusion
This study is the first study of its nature to assess the essential practice elements of AMSBS members, particularly scope of practice, demographics, and experience. We believe that the results of this survey could help improve the quality of care and help achieve the committee’s future goals.
References
- Mostaedi R, Ali MR, Pierce JL, et al. Bariatric surgery and the changing current scope of general surgery practice: implications for general surgery residency training. JAMA Surg. 2015;150(2):144–151.
- Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Surg Obes Relat Dis. 2008;4(5):S109–S184.
- Schwarz N, Groves RM, Schuman H. Survey methods. In: Gilbert DT, Fiske ST, Lindzey G, eds. The Handbook of Social Psychology. McGraw-Hill; 1998:143–179.
- Bonrath EM, Weiner S, Birk D, Hasenberg T. Training in bariatric surgery: a national survey of German bariatric surgeons. Obes Surg. 2020;30(1):56–62.
- Valentine RJ, Jones A, Biester TW, et al. General surgery workloads and practice patterns in the United States, 2007 to 2009: a 10-year update from the American Board of Surgery. Ann Surg. 2011;254(3):520–525.
- Sharoky CE, Sellers MM, Keele LJ, et al. Does surgeon sex matter? Ann Surg. 2018;267(6):1069–1076.
- Centers for Disease Control and Prevention. Adult obesity prevalence maps. https://www.cdc.gov/obesity/data/prevalence-maps.html. Accessed 27 Sep 2022.
- Wen M, Fan JX, Kowaleski-Jones L, Wan N. Rural-urban disparities in obesity prevalence among working age adults in the United States: exploring the mechanisms. Am J Health Promot. 2018;32(2):400–408.
- Lu Y, Juo YY, Martin MJ, et al. Analysis of early job market experiences and perceptions among bariatric surgery fellowship graduates and bariatric surgery program directors. Obes Surg. 2021;31(4):1561–1571.
Category: Current Issue, Original Research




