Clinical Practices to Mitigate Weight Bias
 by Ruchi S. Doshi, MD, MPH, and Kimberly A. Gudzune, MD, MPH
by Ruchi S. Doshi, MD, MPH, and Kimberly A. Gudzune, MD, MPH
Dr. Doshi is with the Duke University Medical Center in Durham, North Carolina. Dr. Gudzune is with the Johns Hopkins University School of Medicine and the Welch Center for Prevention, Epidemiology, and Clinical Research at Johns Hopkins University, in Baltimore, Maryland.
Funding: Kimberly A. Gudzune was supported by grant K23HL116601.
Disclosures: The authors report no conflicts of interest relevant to the content of this manuscript.
Abstract: This article reviews the evidence for how the attitudes, communication, and behaviors of clinicians differ towards patients with obesity, and examines interventions to reduce weight bias among current and future healthcare professionals. Healthcare professionals and trainees display weight bias and negative attitudes toward patients with obesity, which might adversely impact the quality of care received and contribute to health and healthcare disparities. To date, most weight bias reduction interventions studied have targeted short-term changes among trainees rather than practicing clinicians. Successful interventions among trainees include traditional classroom lectures and multimedia interventions, such as films and role-playing that cover the multiple causes of obesity, stigma awareness, and perspectives of patient with obesity, as well as experiential learning, such as longitudinally working with patients who have undergone bariatric surgery. Future studies should examine whether practicing clinicians could benefit from these types of weight bias reduction interventions.
Keywords: Obesity, weight bias, bias reduction, health professionals
Bariatric Times. 2018;15(4):12–16.
Introduction
The quality of healthcare can be influenced by personal characteristics of the clinicians and patients, as well as the systemic organization of the clinical environment.1–3 One primary factor in providing quality healthcare, as perceived by both patients and clinicians, is the patient-clinician relationship.4,5 The perceptions and attitudes of both the clinician and patient can influence their relationship.6–9 Clinician attitudes toward patients can affect clinician behaviors, ultimately influencing the quality of healthcare.10–13 Negative clinician attitudes can affect the patient-clinician relationship, contributing to healthcare disparities.13–15 Multiple factors can affect clinician attitudes, including visible patient characteristics. Past studies have found that age and race can both affect clinician attitudes and behaviors, with physicians respecting older patients6 and exhibiting a more positive affect and patient centeredness toward white patients compared to African-American patients.7 Similarly, a patient’s weight might also impact the patient-clinician relationship and the quality of care provided.13,16
Past literature has shown that individuals with obesity are often stigmatized,17,18 and health professionals have demonstrated biases toward them.19,20 Indeed, the bias of these health professionals are both implicit20,21 and explicit.22,23 Explicit biases are attitudes or beliefs of which a person is conscious and willingly reports, while implicit biases are unconscious and might be inaccessible to control. Currently, over one-third of US adults are obese.24–26 Therefore, if patient obesity negatively impacts the patient-clinician relationship, a substantial number of patients might have negative healthcare experiences and be subject to diminished quality of care. Given that studies have found that disparities in preventive services increase with increasing severity of obesity,27,28 including mammography, pap smears, and colonoscopies,27–33 these results raise concern that weight bias among healthcare professionals might be contributing to healthcare disparities for individuals with obesity.
This article explores how the attitudes, communication, and behaviors of clinicians might influence patients. In addition, the article examines interventions to reduce weight bias among current and future healthcare professionals.
Part 1. Evidence for Health Inequality for Patients with Obesity
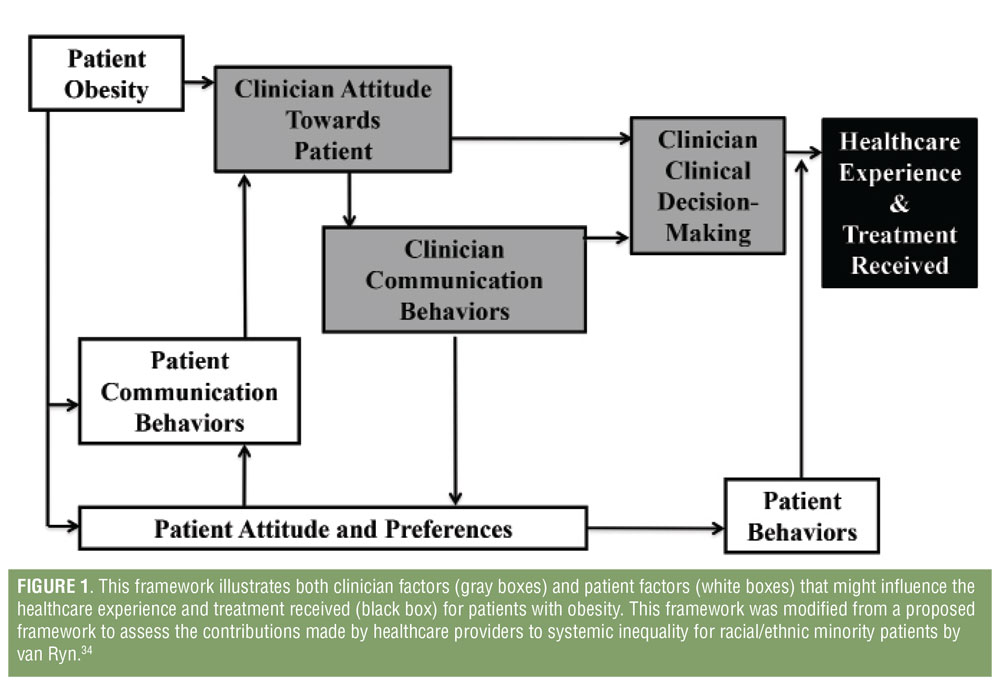
A framework to assess the contributions of healthcare providers to systemic inequality for racial/ethnic minority patients has been previously established.34 This framework can also be helpful in considering how clinician bias might contribute to lower quality care and healthcare disparities for patients with obesity (Figure 1). We review the available evidence supporting the application of this framework for patients with obesity, focusing primarily on clinician factors.
Clinician attitudes toward patients with obesity. Historically, clinicians have displayed negative attitudes toward patients with obesity, and associate obesity with traits such as poor hygiene, non-adherence, and laziness.17,18 These attitudes are pervasive across several areas, including the United States, Australia, Israel, and Europe.35–38 They also have been persistent over time, dating as far back as 1969, when physicians viewed patients with obesity as unintelligent, unsuccessful, inactive, and weak-willed.39 These negative attitudes are not limited to physicians and are found throughout the medical field, including in medical students, nurses, nutrition professionals, and fitness professionals.17,18 Notably, a recent survey found that the majority of medical students have implicit and explicit weight bias, and overall have more negative attitudes toward people with obesity than racial minorities, differing sexual orientations, and differing socioeconomic statuses.40 Over 50 percent of primary care providers (PCPs) report that their heavier patients are less likely to follow their medical advice, benefit from weight counseling, or adhere to medications.41,42 Overall, these perceptions result in clinicians feeling frustrated,37,41,43 which can be detrimental to the clinician-patient relationship.44
Clinician communication behaviors with patients with obesity. Patient overweight and obesity also affects clinician communication, in regard to both patient rapport and weight-loss counseling. One study found that physicians spent less time with patients with overweight or obesity.45 In addition, physicians built less emotional rapport with patients with overweight or obesity compared to their normal weight counterparts.46 This lack of rapport might weaken the clinician-patient relationship, diminish adherence to clinician recommendations, and overall decrease the effectiveness of behavior change counseling.
Clinician decision-making for patients with obesity. Clinician behaviors also differ depending on patient weight status. For example, physicians might order more tests for patients who are overweight or obese, while spending less time with them.45 Other studies have found clinicians might have technical difficulties when performing physical exams, or might not have the appropriately sized equipment to accommodate all patients, which can result in limited physical examinations.29,30
With respect to weight-loss counseling, some studies have demonstrated that physicians currently feel unequipped to treat patients with obesity,47,48 and that their treatments are ineffective.41 In addition, clinicians reported limited time and lack of reimbursement for weight-loss counseling.49–52 They also perceived weight management to be unrewarding or futile,17,37,41,53 which might result in avoiding discussions with weight or weight loss with patients with overweight and obesity entirely.54,55 Moreover, clinicians do not regularly discuss or refer patients to weight loss programs.56–58
Patient factors influencing patient-clinician relationships for patients with obesity. Little is known regarding attitudes, preferences, and communication among patients with obesity; however, research has examined patient behaviors. Studies have shown that patients with overweight or obesity are aware of clinician attitudes toward them, including weight-related bias.13,59,60 Patients with overweight and obesity who perceive that their primary care providers judge them due to their weight have reported having lower trust in these providers.59 Patients with obesity are more likely to doctor shop, defined as three or more PCPs in two years, than patients with normal weight.61 This doctor shopping, which is motivated for some patients by weight-stigmatizing experiences in the healthcare setting,61,62 results in increased utilization of emergency services without increased hospitalization.61 Patients who doctor shop also were more likely to report shorter durations of their current relationships with their healthcare providers.61,62
In addition, patients with obesity might delay care because of perceived barriers due to their weight. Specifically, patients who receive appropriate referrals for cancer screening are concerned about disrespectful treatment, embarrassment at being weighed, negative clinician attitudes, unsolicited weight loss advice, and inadequate medical equipment.30,63 These same factors also led over half of patients with obesity to report canceling a healthcare appointment.63,64
With regard to weight loss, patients that perceive weight-related judgment by providers are more likely to try to lose weight, but not more likely to achieve a clinically significant weight loss.65 Only patients who had a provider discuss weight loss where no judgment was perceived or where the clinician was helpful in the weight loss process achieved clinically significant weight loss.65,66
Part 2. Review of Interventions Mitigating Weight Bias
Few studies have tested interventions that mitigate weight bias among healthcare professionals; a recent systematic review identified only 17 trials.67 Of these trials, only two were delivered to practicing healthcare professionals.68,69 Most interventions addressed only short-term outcomes, and ultimately the review concluded that weight bias might persist in the face of bias-reduction interventions.67 A second meta-analysis on weight-bias interventions in all settings included 30 studies, and concluded that weight bias interventions have had a small, but significant ameliorating effect on anti-fat attitudes and beliefs.70 Interventions studied in these two reviews include traditional classroom and web-based instruction on causes of obesity, weight bias awareness, and bariatric sensitivity training; media-based obesity instruction including videos, audio recordings, and role-play; and experiential learning, including exposure to adult and pediatric patients with obesity.
Traditional instruction regarding obesity. Traditional classroom and web-based educational curricula have focused primarily on healthcare professional students. Few studies were conducted among practicing healthcare professionals. These curricula include formal instruction about the causes of obesity, as well as awareness of how weight bias can impact patients with obesity.
One study specifically examined curricula on causes of obesity, with students randomized to one of three four-week long curricula: uncontrollable causes of obesity, controllable causes of obesity, and a control arm. The authors found a decrease in implicit anti-fat bias among the uncontrollable causes arm and an increase in bias among the controllable causes arm as compared to the control.71 Another study found similar results using single lectures rather than a prolonged curriculum in which a lecture on the uncontrollable causes of obesity resulted in decreased explicit weight bias.72 A third study examined whether reading about genetic or behavioral causes of obesity would affect a virtual encounter with a standardized patient with obesity.73 The investigators found that the group who read about genetic causes of obesity displayed less negative weight stereotyping, but also were less likely to provide screening and counseling for weight loss, exercise, and diet for patients with obesity. These results might suggest that this form of intervention alone is insufficient. A fourth study assessed students who were instructed to read and discuss two articles on communication challenges regarding weight and obesity stigma with a preceptor. Investigators evaluated the effects of the intervention with a standardized patient encounter.74 Immediately post-intervention, students displayed reduced negative stereotyping and increased empathy and confidence when treating patients with obesity. After one year, students maintained improved empathy and confidence; however, they returned to their baseline negative stereotypes.
Two studies examined bariatric sensitivity training for weight bias reduction in which practicing health professionals completed educational modules or training on bariatric sensitivity.68,69 While this strategy increased awareness of how attitudes can impact bariatric patients, it did not improve weight-based attitudes or beliefs toward patients with obesity.
Together, these studies suggest that traditional classroom instruction and educational modules might be effective in the short-term for improving the explicit and implicit attitudes of students, but there is insufficient evidence to determine the effect these modalities have on practicing professionals. Limited evidence demonstrates traditional instruction might have positive long-term effects in some dimensions for students; therefore, it might be prudent to introduce traditional instruction regarding obesity during training for healthcare professionals.
Media-based instruction regarding obesity. Although interventions traditionally involve classroom instruction, researchers have studied the use of media-based weight-bias reduction interventions since the early 1990s. Specifically, use of videos, audio recordings, role-playing, and plays as tools to reduce weight bias in the healthcare setting have been studied.
In 1992, Wiese and colleagues5 worked to reduce weight stigma in medical students through a multimedia course with video, audio, and written components. The course was effective at reducing the explicit negative attitudes and stereotypes of medical students regarding patients with obesity for at least five weeks, and the intervention group was less likely to blame patients with obesity for their condition one year later.In an attempt to replicate these findings and expand upon this study, Rukavina and colleagues76 exposed pre-professional kinesiology students to an audiotape and role-playing activities to increase their awareness of bias and stigma. The investigators reported results consistent with the prior study, in that participants displayed reduced explicit weight bias. Implicit weight bias was not affected.76
Researchers have also studied the effectiveness of videos in reducing weight bias. In one study, participants watched a 17-minute video that promoted stigma reduction by addressing attributions of weight controllability, inducing empathy, and debunking weight-based stereotypes. Participants displayed increased beliefs that genetic and environmental factors had critical roles in causing obesity and demonstrated a decrease in negative stereotypes and negative attitudes.77 Another study found that brief, anti-stigma videos improved explicit, but not implicit, attitudes and beliefs regarding patients with obesity among dietetic and medical students immediately after viewing. These results were not sustained at six weeks.78
Finally, a study by Martharu et al79 examined the effects of reading a dramatic play about obesity to determine its effectiveness in reducing prejudice as compared to a traditional lecture. The authors found that while both the lecture and the play reduced explicit anti-fat bias and increased empathy, those who read the play had a higher decrease in explicit anti-fat bias. Implicit attitudes were not affected by either intervention.
Overall, media-based interventions show promise in reducing explicit bias against patients with obesity, but do not appear to affect implicit bias. There is mixed and insufficient evidence to conclude whether media-based interventions are effective long-term. These findings suggest it might be helpful to incorporate multimedia into a traditional curriculum to further combat weight bias, especially in today’s technological age.
Experiential learning regarding obesity. More recently, researchers have examined the effects of experiential learning on weight stigma. Experiential learning includes witnessing the treatments recommended for patients with obesity, interacting with patients with obesity, and working with senior healthcare professionals who treat patients with obesity. A longitudinal survey of medical students by Phelan et al80 found that limited positive contact with patients with obesity, as well as higher exposure to negative faculty role modeling and comments regarding patients who have obesity, was associated with increasing implicit and explicit anti-fat bias from the Year 1 to Year 4 of medical school.
Cotunga and Mallick81 found that students who followed a calorie-restricted diet for one week had decreased negative attitudes toward patients with obesity. Moreover, students displayed increased respect for patients struggling to lose weight. A study of kinesiology pre-professionals had students participate in a service-learning project in which the intervention group worked with patients who were overweight or obese.76 They found that students in the intervention group had reduced explicit bias, but implicit bias was unchanged. Similarly, another study paired medical students with patients preparing to undergo bariatric surgery and found that students had reduced negative attitudes toward patients with obesity. In addition, the students were more able to recognize weight-related bias and stigma among their senior professionals.82
Together, these studies provide preliminary evidence that experiential learning can be a critical intervention in reducing weight stigma. Exposing students personally to obesity treatments, including dieting and bariatric surgery, might decrease negative attitudes toward patients with obesity. Moreover, limited contact and negative role modeling appear to increase weight bias. Therefore, it might be beneficial for healthcare students to have thorough, prolonged, positive exposure to both patients with and treatments for obesity.
Future bias reduction interventions. Although there are several interventions for bias reduction, most remain untested among practicing clinicians. However, when examining interventions that have been successful in students, programs with multiple components (i.e., traditional classroom instruction, media-based instruction, and experiential learning) and multi-faceted content seem most effective in reducing weight bias. As demonstrated above, education on the causes of weight loss and gain should include genetic, environmental, biological, psychological, and social contributors.71–73,77 Moreover, clinicians might benefit from training weight bias awareness and from the opportunity to examine their own explicit and implicit attitudes.68,69,74,78 Perspective-taking exercises might also help increase clinicians’ empathy and positive affect among clinicians, improving attitudes and reducing stigma toward patients with obesity.75-77,79–82
In addition to educational interventions, clinicians should work to alter the clinic environment to be less stigmatizing by providing chairs and medical equipment that accommodate patients of any size.29,30 Furthermore, when providing obesity care, clinicians should focus on improved health and well-being, rather than solely on body weight.59,65,66
Conclusion
Obesity might make individuals vulnerable to unfair treatment and an impaired quality of care due to weight bias. Specifically, weight bias negatively impacts the attitudes, communication, and behaviors of healthcare professionals. These biases have been pervasive globally for several decades, affecting both practicing clinicians and medical students. Patients with obesity perceive the bias of healthcare professionals, and as a result, are less likely to experience continuity of care or pursue preventive services. This suggests patients with obesity might be receiving lower quality care and suffering from healthcare disparities.
Given the prevalence of overweight and obesity, there is an urgent need to design and test interventions that minimize the effects of weight bias in the healthcare setting, particularly among practicing clinicians. Interventions among trainees that resulted in a sustained increase in empathy and decrease in stereotyping included education on the causes of obesity, increased awareness of weight bias and stigma, and enhanced perspectives on obesity treatments. Other interventions to consider include altering the clinic environment to be more weight-inclusive and changing counseling to promote improved health and well-being rather than focusing on weight.
References
- Mosadeghrad AM. Factors influencing healthcare service quality. Int J Health Policy Manag. 2014;3(2):77–89.
- Napoles-Springer AM, Santoyo J, Houston K, et al. Patients’ perceptions of cultural factors affecting the quality of their medical encounters. Health Expect. 2005;8(1):4–17.
- Naidu A. Factors affecting patient satisfaction and healthcare quality. Int J Health Care Qual Assur. 2009;22(4):366–81.
- Kelley JM, Kraft-Todd G, Schapira L, et al. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207.
- Beach MC, Inui T, Relationship-Centered Care Research N. Relationship-centered care. A constructive reframing. J Gen Intern Med. 2006;21 Suppl 1:S3–8.
- Beach MC, Roter DL, Wang NY, et al. Are physicians’ attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Educ Couns. 2006;62(3):347–54.
- Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94(12):2084–90.
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–9.
- Thornton RL, Powe NR, Roter D, Cooper LA. Patient-physician social concordance, medical visit communication and patients’ perceptions of health care quality. Patient Educ Couns. 2011;85(3):e201–8.
- Beach MC, Rosner M, Cooper LA, et al. Can patient-centered attitudes reduce racial and ethnic disparities in care? Acad Med. 2007;82(2):193–8.
- Gardner T, Refshauge K, Smith L, et al. Physiotherapists’ beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother. 2017;63(3):132–43.
- Browne C, Kehoe M, Salmon N. How beliefs about bladder dysfunction among healthcare professionals influence clinical practice development: perspectives of allied health professionals, nurses, and managers. Int J MS Care. 2017;19(4):191–8.
- Phelan SM, Burgess DJ, Yeazel MW, et al. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–26.
- Dovidio JF, Penner LA, Albrecht TL, et al. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67(3):478–86.
- Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102(5):979–87.
- Huizinga MM, Cooper LA, Bleich SN, et al. Physician respect for patients with obesity. J Gen Intern Med. 2009;24(11):1236–9.
- Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788–805.
- Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring). 2009;17(5):941–64.
- Puhl R, Wharton C, Heuer C. Weight bias among dietetics students: implications for treatment practices. J Am Diet Assoc. 2009;109(3):438–44.
- Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes Relat Metab Disord. 2001;25(10):1525–31.
- Schwartz MB, Chambliss HO, Brownell KD, et al. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11(9):1033–9.
- Sabin JA, Marini M, Nosek BA. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS One. 2012;7(11):e48448.
- Tomiyama AJ, Finch LE, Belsky AC, et al. Weight bias in 2001 versus 2013: contradictory attitudes among obesity researchers and health professionals. Obesity (Silver Spring). 2015;23(1):46–53.
- Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–91.
- Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015(219):1–8.
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–14.
- Maruthur NM, Bolen SD, Brancati FL, Clark JM. The association of obesity and cervical cancer screening: a systematic review and meta-analysis. Obesity (Silver Spring). 2009;17(2):375–81.
- Maruthur NM, Bolen S, Brancati FL, Clark JM. Obesity and mammography: a systematic review and meta-analysis. J Gen Intern Med. 2009;24(5):665–77.
- Ferrante JM, Fyffe DC, Vega ML, et al. Family physicians’ barriers to cancer screening in extremely obese patients. Obesity (Silver Spring). 2010;18(6):1153–9.
- Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for white and African-American obese women. Int J Obes (Lond). 2006;30(1):147–55.
- Maruthur NM, Bolen S, Gudzune K, et al. Body mass index and colon cancer screening: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2012;21(5):737–46.
- Fischer R, Collet TH, Zeller A, et al. Obesity and overweight associated with lower rates of colorectal cancer screening in Switzerland. Eur J Cancer Prev. 2013;22(5):425–30.
- Rosen AB, Schneider EC. Colorectal cancer screening disparities related to obesity and gender. J Gen Intern Med. 2004;19(4):332–8.
- van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(1 Suppl):I140–51.
- Harvey EL, Hill AJ. Health professionals’ views of overweight people and smokers. Int J Obes Relat Metab Disord. 2001;25(8):1253–61.
- Thuan JF, Avignon A. Obesity management: attitudes and practices of French general practitioners in a region of France. Int J Obes (Lond). 2005;29(9):1100–6.
- Campbell K, Engel H, Timperio A, et al. Obesity management: Australian general practitioners’ attitudes and practices. Obes Res. 2000;8(6):459–66.
- Fogelman Y, Vinker S, Lachter J, et al. Managing obesity: a survey of attitudes and practices among Israeli primary care physicians. Int J Obes Relat Metab Disord. 2002;26(10):1393–7.
- Maddox GL, Liederman V. Overweight as a social disability with medical implications. J Med Educ. 1969;44(3):214–20.
- Phelan SM, Dovidio JF, Puhl RM, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity (Silver Spring). 2014;22(4):1201–8.
- Foster GD, Wadden TA, Makris AP, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11(10):1168–77.
- Huizinga MM, Bleich SN, Beach MC, et al. Disparity in physician perception of patients’ adherence to medications by obesity status. Obesity (Silver Spring). 2010;18(10):1932–7.
- Ruelaz AR, Diefenbach P, Simon B, et al. Perceived barriers to weight management in primary care—perspectives of patients and providers. J Gen Intern Med. 2007;22(4):518–22.
- Malterud K, Ulriksen K. Obesity, stigma, and responsibility in health care: A synthesis of qualitative studies. Int J Qual Stud Health Well-being. 2011;6(4).
- Hebl MR, Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001;25(8):1246–52.
- Gudzune KA, Beach MC, Roter DL, Cooper LA. Physicians build less rapport with obese patients. Obesity (Silver Spring). 2013;21(10):2146–52.
- Forman-Hoffman V, Little A, Wahls T. Barriers to obesity management: a pilot study of primary care clinicians. BMC Fam Pract. 2006;7:35.
- Block JP, DeSalvo KB, Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Prev Med. 2003;36(6):669–75.
- Gunther S, Guo F, Sinfield P, et al. Barriers and enablers to managing obesity in general practice: a practical approach for use in implementation activities. Qual Prim Care. 2012;20(2):93–103.
- Jansen S, Desbrow B, Ball L. Obesity management by general practitioners: the unavoidable necessity. Aust J Prim Health. 2015;21(4):366–8.
- Findholt NE, Davis MM, Michael YL. Perceived barriers, resources, and training needs of rural primary care providers relevant to the management of childhood obesity. J Rural Health. 2013;29 Suppl 1:s17–24.
- Lee JS, Sheer JL, Lopez N, Rosenbaum S. Coverage of obesity treatment: a state-by-state analysis of Medicaid and state insurance laws. Public Health Rep. 2010;125(4):596–604.
- Havrankova J. Is the treatment of obesity futile?: YES. Can Fam Physician. 2012;58(5):508, 10.
- Nolan C, Deehan A, Wylie A, Jones R. Practice nurses and obesity: professional and practice-based factors affecting role adequacy and role legitimacy. Prim Health Care Res Dev. 2012;13(4):353–63.
- Gudzune KA, Clark JM, Appel LJ, Bennett WL. Primary care providers’ communication with patients during weight counseling: a focus group study. Patient Educ Couns. 2012;89(1):152–7.
- Sebiany AM. Primary care physicians’ knowledge and perceived barriers in the management of overweight and obesity. J Family Community Med. 2013;20(3):147–52.
- Ferrante JM, Piasecki AK, Ohman-Strickland PA, Crabtree BF. Family physicians’ practices and attitudes regarding care of extremely obese patients. Obesity (Silver Spring). 2009;17(9):1710–6.
- Kristeller JL, Hoerr RA. Physician attitudes toward managing obesity: differences among six specialty groups. Prev Med. 1997;26(4):542–9.
- Gudzune KA, Bennett WL, Cooper LA, Bleich SN. Patients who feel judged about their weight have lower trust in their primary care providers. Patient Educ Couns. 2014;97(1):128–31.
- Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity (Silver Spring). 2006;14(10):1802–15.
- Gudzune KA, Bleich SN, Richards TM, et al. Doctor shopping by overweight and obese patients is associated with increased healthcare utilization. Obesity (Silver Spring). 2013;21(7):1328–34.
- Gudzune KA, Bennett WL, Cooper LA, et al. Prior doctor shopping resulting from differential treatment correlates with differences in current patient-provider relationships. Obesity (Silver Spring). 2014;22(9):1952–5.
- Drury CA, Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. J Am Acad Nurse Pract. 2002;14(12):554–61.
- Olson CL, Schumaker HD, Yawn BP. Overweight women delay medical care. Arch Fam Med. 1994;3(10):888–92.
- Gudzune KA, Bennett WL, Cooper LA, Bleich SN. Perceived judgment about weight can negatively influence weight loss: a cross-sectional study of overweight and obese patients. Prev Med. 2014;62:103–7.
- Bennett WL, Wang NY, Gudzune KA, et al. Satisfaction with primary care provider involvement is associated with greater weight loss: Results from the practice-based POWER trial. Patient Educ Couns. 2015;98(9):1099–105.
- Alberga AS, Pickering BJ, Alix Hayden K, et al. Weight bias reduction in health professionals: a systematic review. Clin Obes. 2016;6(3):175–88.
- Gujral H, Tea C, Sheridan M. Evaluation of nurse’s attitudes toward adult patients of size. Surg Obes Relat Dis. 2011;7(4):536–40.
- Falker AJ, Sledge JA. Utilizing a bariatric sensitivity educational module to decrease bariatric stigmatization by healthcare professionals. Bariatr Nurs Surg Patient Care. 2011;6:73–8.
- Lee M, Ata RN, Brannick MT. Malleability of weight-biased attitudes and beliefs: a meta-analysis of weight bias reduction interventions. Body Image. 2014;11(3):251–9.
- O’Brien KS, Puhl RM, Latner JD, et al. Reducing anti-fat prejudice in preservice health students: a randomized trial. Obesity (Silver Spring). 2010;18(11):2138–44.
- Diedrichs PC, Barlow FK. How to lose weight bias fast! Evaluating a brief anti-weight bias intervention. Br J Health Psychol. 2011;16(4):846–61.
- Persky S, Eccleston CP. Impact of genetic causal information on medical students’ clinical encounters with an obese virtual patient: health promotion and social stigma. Ann Behav Med. 2011;41(3):363–72.
- Kushner RF, Zeiss DM, Feinglass JM, Yelen M. An obesity educational intervention for medical students addressing weight bias and communication skills using standardized patients. BMC Med Educ. 2014;14:53.
- Wiese HJ, Wilson JF, Jones RA, Neises M. Obesity stigma reduction in medical students. Int J Obes Relat Metab Disord. 1992;16(11):859–68.
- Rukavina PB, Li W, Shen B, Sun H. A service learning based project to change implicit and explicit bias toward obese individuals in kinesiology pre-professionals. Obes Facts. 2010;3(2):117–26.
- Poustchi Y, Saks NS, Piasecki AK, et al. Brief intervention effective in reducing weight bias in medical students. Fam Med. 2013;45(5):345–8.
- Swift JA, Tischler V, Markham S, et al. Are anti-stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized control trial. Obes Facts. 2013;6(1):91–102.
- Matharu K, Shapiro JF, Hammer RR, et al. Reducing obesity prejudice in medical education. Educ Health (Abingdon). 2014;27(3):231–7.
- Phelan SM, Puhl RM, Burke SE, et al. The mixed impact of medical school on medical students’ implicit and explicit weight bias. Med Educ. 2015;49(10):983–92.
- Cotugna N, Mallick A. Following a calorie-restricted diet may help in reducing healthcare students’ fat-phobia. J Community Health. 2010;35(3):321–4.
- Roberts DH, Kane EM, Jones DB, et al. Teaching medical students about obesity: a pilot program to address an unmet need through longitudinal relationships with bariatric surgery patients. Surg Innov. 2011;18(2):176–83.
Category: Past Articles, Review



