Composition and Salaries of the Integrated Health Professional Team in Metabolic and Bariatric Surgery: Results of an ASMBS Survey
 by Michelle R. Lent, PhD
by Michelle R. Lent, PhD
Dr. Lent is with the Philadelphia College of Osteopathic Medicine in Philadelphia, Pennsylvania, and the Geisinger Medical Center in Danville, Pennsylvania.
Funding: No funding was provided for this article.
Disclosures: The author reports no conflicts of interest relevant to the content of this manuscript.
Bariatric Times. 2018;15(5):11–12.
Introduction
Incorporating an integrated health approach for the pre- and postoperative care of bariatric surgery patients is essential for appropriate evaluation, preparation, coaching, and long-term success.1 Thus, multidisciplinary care is considered the standard of care for bariatric surgery programs in the United States. The actual composition of a multidisciplinary team seems to vary significantly and can include bariatricians, endocrinologists, nursing and advance practice providers, dietitians and behavioral health providers, exercise specialists, pharmacists, and bariatric surgeons. Each integrated health team member plays a different role and provides a wide range of services for metabolic and bariatric surgery patients, with the goals of optimizing presurgical conditioning and maximizing long-term success of surgery. However, there is little knowledge about the variability in integrated care delivery structure, the roles of each team member, and the compensation provided for patient care.
The Multidisciplinary Care Committee of the American Society for Metabolic and Bariatric Surgery (ASMBS) surveyed society members regarding their roles and related compensation across membership disciplines. The 20-question online survey was distributed to 4,000 ASMBS members via email from May 2017 to January 2018.
Results
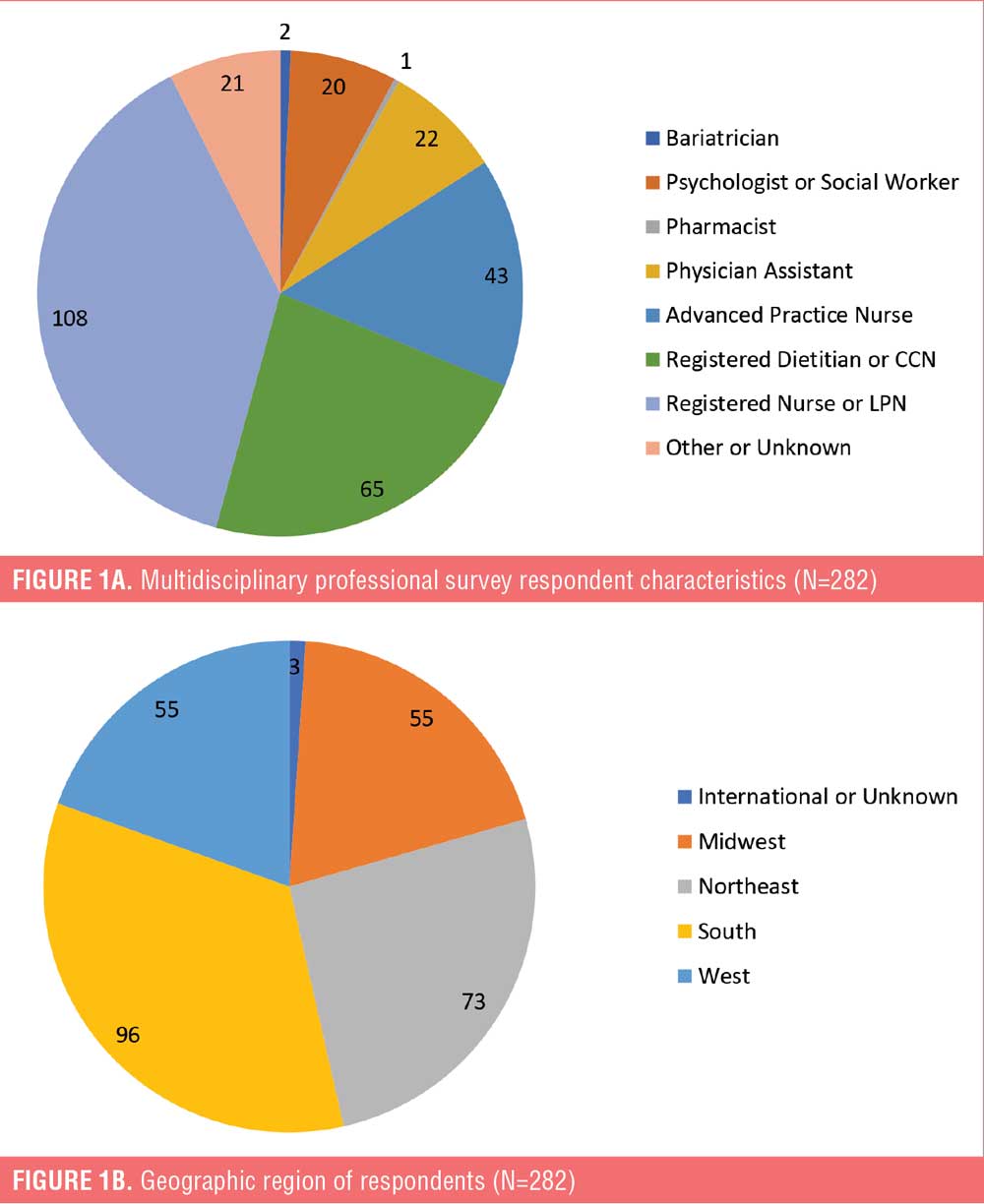
Of the 282 bariatric surgery professionals that responded, the majority were registered nurses (38.1%, Figure 1A), employed by hospitals (64.2%), worked full-time (94.6%), and in practice for longer than 10 years (65.2%). Most respondents were located in the Southern region of the United States (34%), followed by the Northeast (25.9%, Figure 1B).
The survey identified several notable patterns regarding the practice of multidisciplinary care in bariatric surgery programs:
For most respondents (80.5%), greater than 80 percent of their occupational time is dedicated to bariatrics.
Of the professional time allocated to bariatric surgery care, most professionals reported that their roles included both clinical and administrative duties (65.5%).
Only 18 percent reported that their position required taking call; of those, only four percent reported specific compensation for taking call.
Opportunities for incentives or productivity bonuses from employers were rare (14.3%). For employees offered incentives or bonuses, the majority of respondents indicated that these were based on group, individual, or system-wide productivity metrics or if budget goals were achieved.
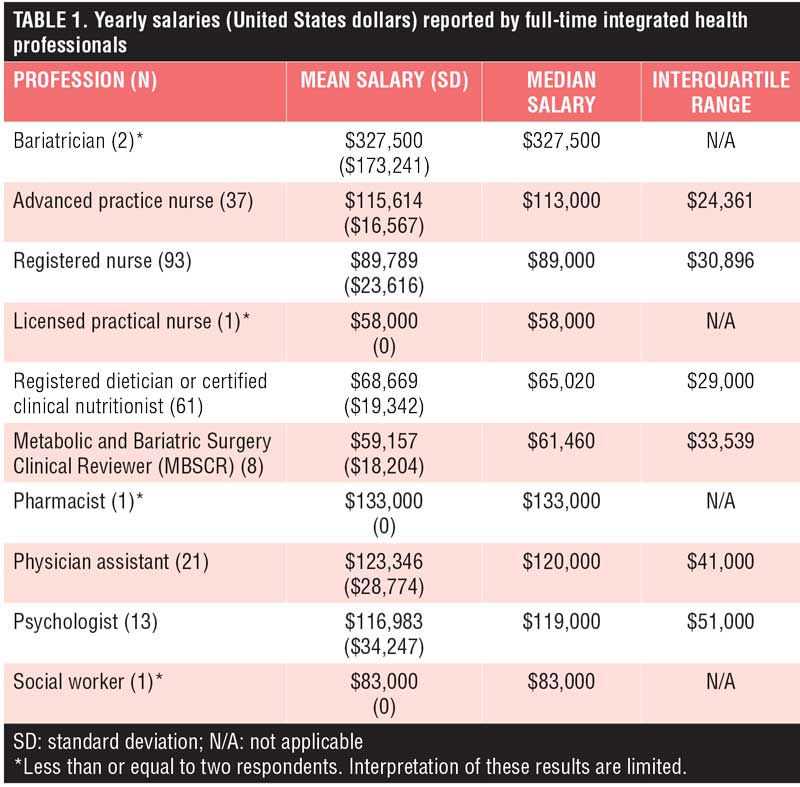
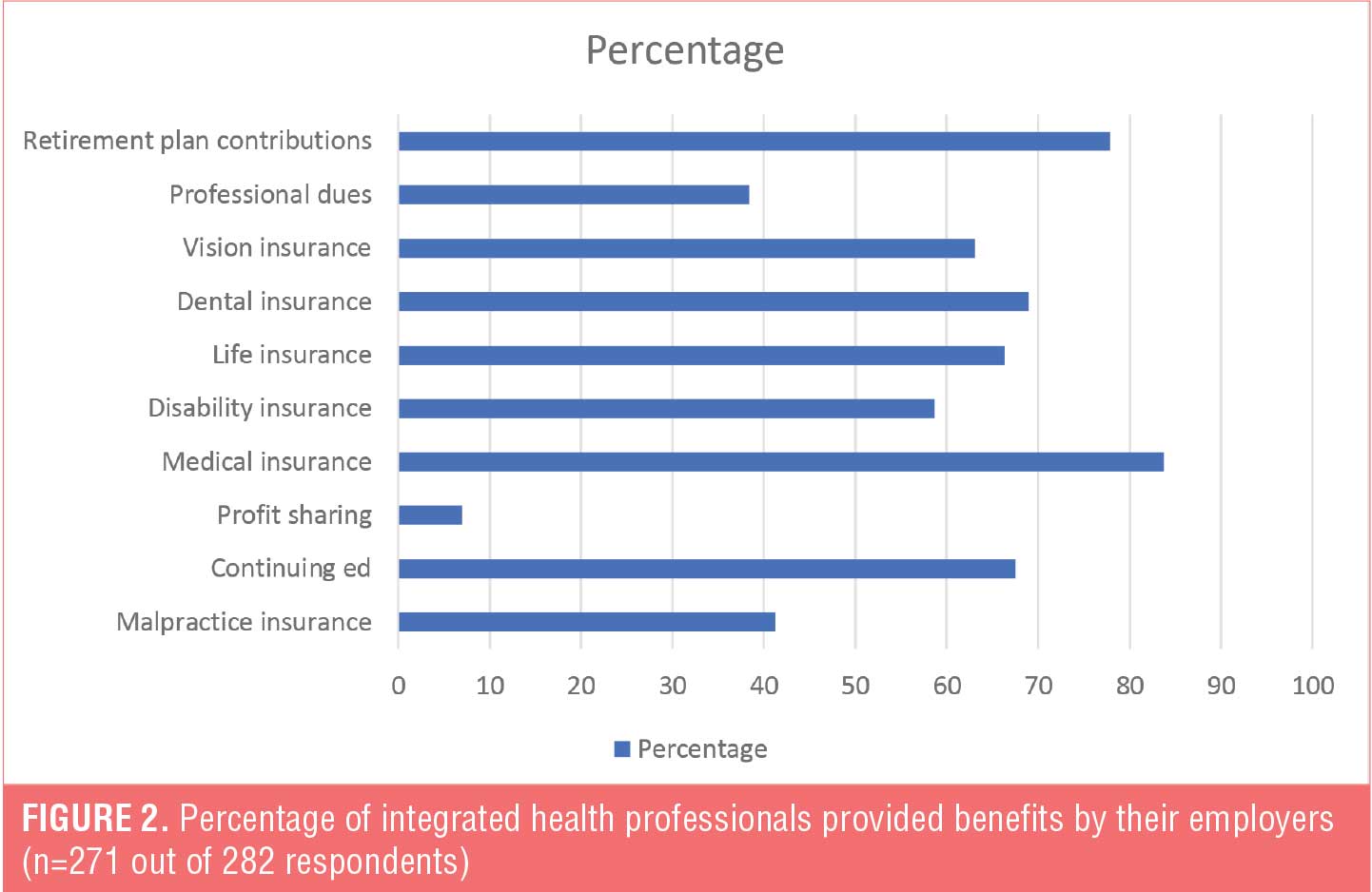
The survey also inquired about the yearly compensation and benefits provided by their employers. The median salary reported by registered dietitians and certified clinical nutritionists working in bariatrics was $65,000, and the median salary for registered nurses was $89,000. Additional integrated health professional salaries are in Table 1. Benefits most frequently offered by their employers are medical insurance (83.8%), retirement plan contributions (77.9%), dental insurance (69.0%), and continuing education coverage (67.5%) (Figure 2).
Conclusion
“The care of weight-loss surgery patients can be complex and multifaceted,” said Amber Saucier, MS, RD, at Lafayette General Health in Lafayette, Louisiana, and member of the ASMBS Multidisciplinary Care Committee. “Greater understanding of how integrated health professionals are utilized and compensated for bariatric patient care across the United States can help programs select the multidisciplinary services that are best suited for their patients’ needs.”
Limitations of the survey results include the low response rate and the over-representation of nurses compared to other integrated health disciplines (46.5%) and female respondents (92.2%).
References
- Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013;9(2):159–191.
Category: Brief Report, Past Articles




