Patients with Obesity Need Not Routinely Undergo Rapid Sequence Anesthetic Induction
 by Jay B. Brodsky, MD
by Jay B. Brodsky, MD
Dr. Brodsky is Professor, Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine in Stanford, California.
Funding: No funding was provided for this article.
Disclosures: The authors report no conflicts of interest relevant to the content of this manuscript.
Abstract: A “rapid sequence induction” (RSI) has been a routine part of the anesthetic management of patients with morbid obesity for over 40 years. A RSI consists of the rapid administration of a quick acting anesthetic induction agent and a paralytic in order to intubate the trachea as quickly as possible. Cricoid pressure is also applied in an attempt to reduce the risk of gastric aspiration. Recent evidence suggests that not only is RSI not needed for most patients with obesity, but it is probably ineffective in preventing aspiration and might also distort the airway making tracheal intubation more difficult.
Keywords: Rapid sequence induction, morbid obesity, pulmonary aspiration, safe apnea period, cricoid pressure
Bariatric Times. 2018;15(5):8–10.
Introduction
A “rapid sequence induction” (RSI) is a technique used by anesthesiologists to produce the rapid onset of general anesthesia and paralysis immediately prior to tracheal intubation in order to reduce the risk of pulmonary aspiration. The goal of RSI is to minimize the time between apnea with loss of protective airway reflexes and successful placement of a cuffed endotracheal tube. RSI consists of the intravenous administration in rapid succession of both a quick-onset anesthetic induction agent and a fast-acting muscle relaxant. Cricoid pressure is applied, and bag-mask ventilation is avoided. Many anesthesiologists continue to perform RSI as part of their routine management of all patients with obesity. There is increasing evidence that this practice is not only unnecessary but might actually be harmful.
RSI in Current Practice
RSI is usually used before emergency procedures on non-fasted patients and for elective surgical patients who are believed to be at increased risk for pulmonary aspiration. Pulmonary aspiration is defined as the presence of bilious secretions or particulate matter in the tracheobronchial tree and/or the presence of an infiltrate on the postoperative chest roentgenogram that was not present preoperatively. The incidence of clinically significant aspiration for all surgical patients is extremely low, occurring in less than 3 in 10,000 general anesthetics.
It is controversial as to whether RSI actually protects the airways from contamination.1 Aspiration, when it occurs, is usually associated with emergency surgery, and almost all of these patients underwent RSI. A large meta-analysis concluded that there is no evidence to support or refute the efficacy of RSI in reducing aspiration.2 Despite these findings, RSI is considered the “standard of care” for induction of anesthesia and tracheal intubation in patients believed to be at risk for aspiration.
Aspiration risk factors include the presence of significant gastro-esophageal reflux disease (GERD), ileus, acute abdomen, term pregnancy, diabetes mellitus with autonomic neuropathy, impaired levels of consciousness, and patients with neurologic conditions causing loss of gag reflexes. These patients routinely undergo RSI.
RSI and Patients with Obesity
RSI has been a part of the anesthetic management of patients with obesity for many years.3 This practice was based on a study from 1975 that reported that fasting patients with obesity had larger volumes (>25mL) of more acidotic (pH<2.5) gastric fluid than similar patients who are lean.4 Since the severity of the pneumonitis following aspiration depends on the volume and acidity of the material aspirated, obesity by itself was considered a risk factor. More recent studies have challenged these findings. The volume and pH of gastric fluid is identical in both subjects with obesity and normal weight.5 The gastric contents of unpremedicated, non-diabetic fasting patients with obesity (body mass index [BMI] >30kg/m2) without significant gastro-esophageal pathology are not different than other surgical patients.6 A subset of patients with obesity and severe GERD or Type 2 diabetes mellitus with autonomic neuropathy (gastroparesis) might be at increased risk, but evidence of significant aspiration events for even these patients does not exist.
Although some authors continue to recommend RSI for all surgical patients with morbid obesity,7 there is increasing recognition that it is unnecessary in fasted patients with obesity without other risk factors. The European Society of Anaesthesiology and the American Society of Anesthesiologists have each published guidelines on reducing the risk of perioperative aspiration.8,9 Both do not consider obesity to be a risk factor and recommend that patients with obesity who are without gastroparesis or symptomatic GERD follow the same fasting guidelines as patients of normal weight and be allowed to drink clear liquids up until two hours before elective surgery.
The 4th National Audit Project (NAP4) reviewed airway management complications in the United Kingdom. Mortality from all causes was extremely rare—approximately one death in 180,000 general anesthetics. Gastric aspiration, the most frequent cause of anesthesia-related mortality, was reported to occur in a “disproportionate” number of patients with obesity.10 However, NAP4 did not identify obesity as the aspiration risk, but rather found that complications occurred because of unfamiliarity by some anesthesiologists with the appropriate airway management of obese patients, including poor clinical judgment, failure to protect the airway by the inappropriate use of supraglottic airways, and not being properly prepared when difficulty with tracheal intubation occurred.
Should RSI be performed on patients with obesity who have previously undergone bariatric procedures? There have been no reports of aspiration in patients who have had a gastric bypass or sleeve gastrectomy. Some studies do report development of new symptoms of GERD after sleeve gastrectomy,14 while others report resolution of pre-existing reflux symptoms after the same operation.15 Gastric bypass consistently results in long-lasting improvement in GERD,16 and presumably a decrease in the risk of aspiration during subsequent anesthetics. There have been isolated case reports and one small series of patients who had a gastric banding who, despite preoperative fasting and an RSI, aspirated on induction of general anesthesia before subsequent operations.11–13 This suggests that only those former bariatric patients who have had a gastric banding should undergo RSI.
Risks of RSI Among General Population
Since pulmonary aspiration during general anesthesia is extremely rare, concerns have been raised as to whether the potential risks of RSI are greater than its presumed benefits.
The 5th National Audit Project (NAP5) in the United Kingdom found that awareness under anesthesia occurred most often during the induction of anesthesia, usually during urgent or emergent procedures involving RSI.17 During RSI bolus, doses of induction and paralyzing drugs are given in quick succession. NAP5 reported that titration of the anesthetic induction agent until loss of consciousness is achieved would reduce awareness events. NAP5 suggested a “fundamental reassessment” of the indications for RSI.
Cricoid pressure is an integral part of RSI. Applying too low a force can lead to incomplete occlusion of the esophagus, while excessive force can compress the trachea and deform the airway anatomy making tracheal intubation more difficult.18 The incidence of failed intubations is increased when cricoid pressure is applied.19 Cricoid pressure also decreases lower esophageal sphincter tone, and this might explain the occurrence of aspiration during RSI.20 Cricoid pressure is difficult to perform correctly, is potentially dangerous, and probably offers no protection.
Optimal Anesthetic Induction in Patients with Obesity
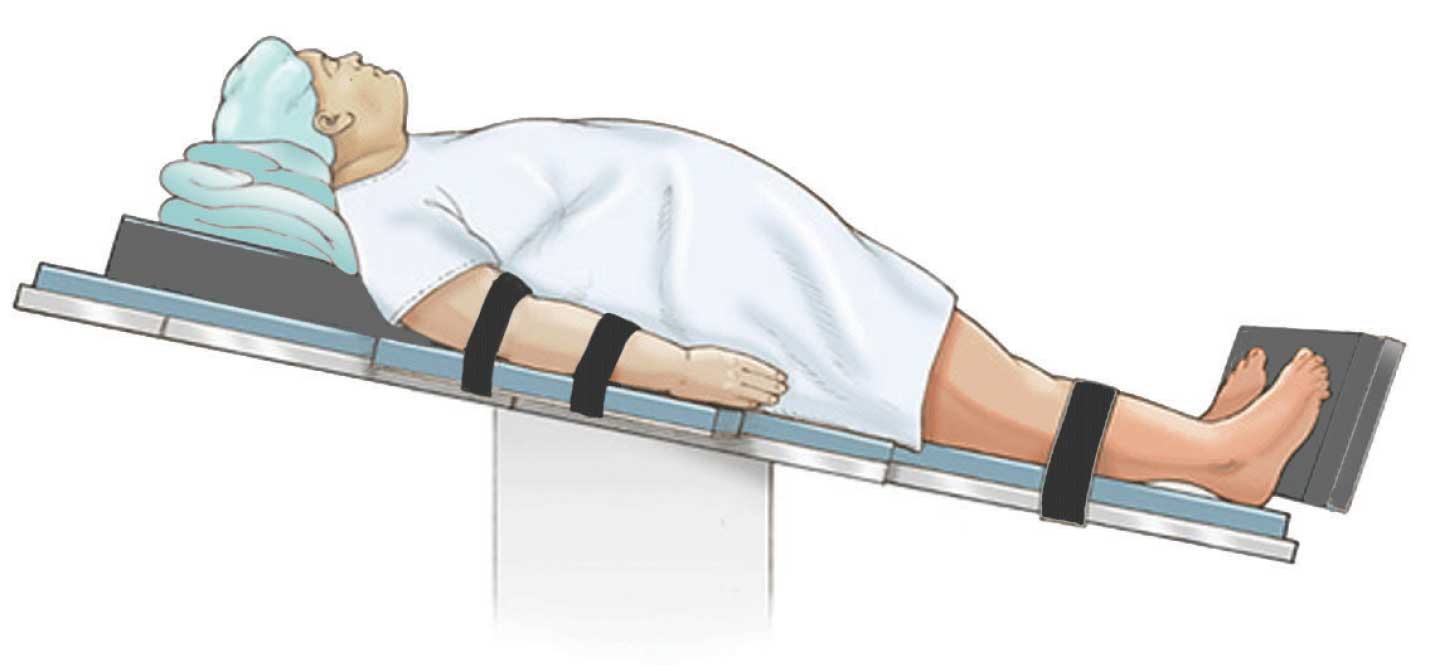
The anesthetic management of a patient with morbid obesity does differ from that of other patients. For induction, the standard supine position must be avoided since a patient with obesity lying flat will experience a marked decrease in lung volume. This will result in a marked reduction of oxygen reserves following preoxygenation. The “safe apnea period” (SAP), that is, the length of time following paralysis and apnea until the onset of hypoxemia, is very short. Unless tracheal intubation is achieved quickly and/or the duration of SAP is increased, patients with obesity can experience hypoxemia following paralysis. A patient with obesity should be placed in a “ramped” or “head-elevated laryngoscopy position” (HELP).21 This improves the view during direct laryngoscopy so that successful tracheal intubation can be accomplished more rapidly.22 If the patient is hemodynamically stable, the operating table should also be tilted in a reverse-Trendelenburg position to “unload” the diaphragm. This will increase lung volume and oxygen reserves, lengthening the duration of the SAP and allowing more time to intubate the trachea.
Prior to induction, a patient with obesity is preoxygenated until his or her oxygen saturation (SpO2) is 100 percent and end-tidal O2 is greater than 90 perecnt. The application of some form of “apneic oxygenation” (THRIVE, nasal cannulae or buccal O2) can also be applied. In RSI, bag-mask ventilation is avoided because of concerns that positive-pressure ventilation will inflate the stomach, increasing the risk of aspiration. It has been demonstrated that clinically significant gastric insufflation does not occur during normal bag-mask ventilation, even when cricoid pressure is applied.23 The incidence of oxygen desaturation (SpO2 < 95%) is as high as 35 percent in patients undergoing RSI without bag-mask ventilation.24 For a patient with obesity and a markedly shortened SAP, the risk of hypoxemia could be even greater, especially if an initial attempt at tracheal intubation fails. Unlike RSI, the anesthetic induction of a patient with obesity should include positive-pressure bag-mask ventilation following paralysis and prior to intubation.25–26
Giving fixed doses of drugs in rapid succession during RSI can lead to under-dosing and patient awareness, or over-dosing with potentially serious hemodynamic consequences. Administration of the induction agent in a patient with obesity should titrated to loss of consciousness. The initial dose should be based on lean body weight and not total body weight. Following administration of the induction agent, assessment of adequate depth of anesthesia should be performed before administering a neuromuscular blocking agent for tracheal intubation. The addition of an opioid before RSI can also improve conditions. A short-acting opioid (fentanyl, sufentanil, remifentanil, alfentanil) should be given to supplement the induction agent and decrease the incidence of awareness.
Bag-mask ventilation is applied before a muscle relaxant is administered. Although fast-acting succinylcholine has historically been the relaxant of choice for RSI, there is some evidence that the fasciculations from succinylcholine increase oxygen consumption and shorten SAP. With the availability of the reversal agent suggammadex, rocuronium is now recommended before tracheal intubation. Bag-mask positive pressure ventilation should be continued until the patient is completely paralyzed and optimal conditions for tracheal intubation are achieved. Conventional direct laryngoscopy is usually successful in most patients with obesity. The use of video-laryngoscopy might further increase the success rate for tracheal intubation in patients with morbid obesity. Application of cricoid pressure is avoided since it can increase the degree of difficulty and time required for intubation, potentially increasing the risk of hypoxemia.
Conclusion
In conclusion, for many bariatric surgical patients, RSI continues to be a routine part of their management because of the misperception by some anesthesiologists that patients with obesity are at increased risk for gastric aspiration and pulmonary injury. However, RSI is not without its own risks (e.g., awareness, under-and overdosing of drugs, impaired visualization during laryngoscopy, hypoxia). These risks are probably greater than the potential risk of aspiration. Therefore, unless the patient with obesity has significant aspiration risk factors, RSI is unnecessary, potentially dangerous, and should not be performed.
References
- El-Orbany M, Connolly LA. Rapid sequence induction and intubation: current controversy. Anesth Analg. 2010;110:1318–25.
- Neilipovitz DT, Crosby ET. No evidence for decreased incidence of aspiration after rapid sequence induction. Can J Anaesth. 2007;54:748–54.
- Freid EB. The rapid sequence induction revisited: obesity and sleep apnea syndrome. Anesthesiol Clin North Am. 2005;23:551–64.
- Vaughan RW, Bauer S, Wise L. Volume and pH of gastric juice in obese patients. Anesthesiology. 1975;43:686–8.
- Juvin PH, Fevre G, Merouche M, et al. Gastric residue is not more copious in obese patients. Anesth Analg. 2001;93:1621–2.
- Harter RL, Kelly WB, Kramer MG, et al. A comparison of the volume and pH of gastric contents of obese and lean surgical patients. Anesth Analg. 1998;86:147–52.
- Gaszynski TM, Szewczyk T. Rocuronium for rapid sequence induction in morbidly obese patients: a prospective study for evaluation of intubation conditions after administration 1.2 mg kg2 ideal body weight of rocuronium. Eur J Anaesthesiol. 2011;28:609–10.
- Smith I, Kranke P, Murat I, et al. Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anesthesiol. 2011;l28:556–69.
- American Society of Anesthesiologists Committee. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology. 2011;114:495–511.
- Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: Anaesthesia. Brit J Anesth. 2011;106:617–31.
- Kocian R, Spahn DR. Bronchial aspiration in patients after weight loss due to gastric banding. Anesth Analg. 2005;100:1856–7.
- Thekkethodika A. The risk of regurgitation and pulmonary aspiration in a patient after gastric banding. Case Rep Anesthesiol. 2012; doi: 10.1155/2012/18610.
- Jean J, Compere V, Foundrinier V, et al. The risk of pulmonary aspiration in patients after weight loss due to bariatric surgery. Anesth Analg. 2008;107:1257–9.
- Abdemur A, Han SM, Lo Menzo E, et al. Reasons and outcomes of conversion of laparoscopic sleeve gastrectomy to Roux-en-Y gastric bypass for nonresponders. Surg Obes Relat Dis. 2016;12:113–8.
- Sucandy I, Chrestiana D, Bonanni F, Antanavicius G. Gastroesophageal reflux symptoms after laparoscopic sleeve gastrectomy for morbid obesity. The importance of preoperative evaluation and selection. N Am J Med Sci. 2015;7:189–93.
- Fressa EE, Ikramuddin S, Gourash W, et al. Symptomatic improvement in gastroesophageal reflux disease (GERD) following Roux-en-Y gastric bypass. Surg Endosc. 2002;16:1027–31.
- Pandit JJ, Andrade J, Bogod DG, et al. 5th National Audit Project (NAP5) on accidental awareness during general anaesthesia: summary of main findings and risk factors. Brit J Anaesth. 2014;113:549–59.
- Smith KJ, Dobranowski J, Yip G, et al. Cricoid pressure displaces the esophagus: an observational study using magnetic resonance imaging. Anesthesiology. 2003;99:60–4.
- Brimacombe JR, Berry AM. Cricoid pressure. Can J Anaesth. 1997;44:414–25.
- Tournadre JP, Chassard D, Berrada KR, Bouletreau P. Cricoid cartilage pressure decreases lower esophageal sphincter tone. Anesthesiology. 1997;86:7–9.
- Collins JS, Lemmens HJ, Brodsky JB, et al. Laryngoscopy and morbid obesity: a comparison of the “sniff” and “ramped” positions. Obes Surg. 2004;14:1171–5.
- Brodsky JB, Lemmens HJ, Brock-Utne JG, et al. Morbid obesity and tracheal intubation. Anesth Analg. 2002;94:732–6.
- Lawes EG, Campbell I, Mercer D. Inflation pressure, gastric insufflation and rapid sequence induction. Brit J Anaesth. 1987;59:315–8.
- Gebremedhn EG, Mesele D, Aemero D, Alemu E. The incidence of oxygen desaturation during rapid sequence induction and intubation. World J Emerg Med. 2014;5:279–85.
- Harbut P, Gozdik W, Stjernfalt E, et al. Continuous positive airway pressure/pressure support pre-oxygenation of morbidly obese patients. Acta Anaesthesiol Scand. 2014;58:675–80.
- Gander S, Frascarolo P, Suter M, et al. Positive end-expiratory pressure during induction of general anesthesia increases duration of nonhypoxic apnea in morbidly obese patients. Anesth Analg. 2005;100:580–4.
Category: Past Articles, Review



