Intuitive Eating is Associated with a Healthier Relationship with Food in Postsurgical Bariatric Patients
 by Narmin Virani, RDN, CSOWM; Kasey P.S. Goodpaster, PhD; and Richard Perugini, MD, FACS
by Narmin Virani, RDN, CSOWM; Kasey P.S. Goodpaster, PhD; and Richard Perugini, MD, FACS
Ms. Virani and Dr. Perugini are with the University of Massachusetts Memorial Bariatric Center in Worcester, Massachusetts. Dr. Goodpaster is with the Cleveland Clinic Bariatric and Metabolic Institute in Cleveland, Ohio.
FUNDING: No funding was provided.
DISCLOSURES: The authors have no disclosures relevant to the content of this article.
ABSTRACT: Objective. The objective was to study the association between intuitive eating (IE) and mindful eating (ME), and their relationship with eating, emotional eating, and self-efficacy in patients who undergo bariatric surgery.
Design. This correlational study analyzed using linear regression.
Setting. The study was completed at University of Massachusetts Memorial Bariatric Center.
Participants. In total, 90 participants involved in an online support group associated with the bariatric program (77.8% female, 90.0% Caucasian, aged 27–74 years, body mass index [BMI] 23–52kg/m2) were included. Time since surgery ranged from three months to more than five years, with most patients (40.7%) in the 3-to-11 month postsurgery range.
Measurements. The study utilized the Intuitive Eating Scale-2, Emotional Overeating Questionnaire, and a questionnaire designed for this study.
Results. Higher IE scores were significantly positively associated with satisfaction from meals (p=0.03), mindful eating (p=0.02), self-efficacy with maintaining eating behaviors long-term (p<0.0001), feeling in control of eating (p<0.0001), having a positive relationship with eating (p<0.0001), making time for relaxation (p=0.04), and regular physical activity (p=0.002). IE was negatively associated with emotional eating (p<0.0001), fear of weight regain (p<0.0001), perceived stress (p=0.01), and tendency to prioritize others’ needs before one’s own (p=0.002). Unexpectedly, IE was not significantly associated with diet variety nor determining portions based on hunger/fullness levels.
Conclusion. Patients who undergo bariatric surgery who embody IE principles are less likely to have challenges with emotional overeating. They feel more in control with eating and confident about maintaining behaviors long-term. IE principles can be adapted for bariatric populations and integrated into pre- and postsurgical counseling.
KEYWORDS: bariatric surgery, obesity, nutrition, psychology, behavioral health, integrated health, eating disorders
Bariatric Times. 2020;17(9):10–15.
The prevalence of obesity (body mass index [BMI] of 30kg/m2 and above) was 39.8 percent among adults and 18.5 percent among youth in the United States (US) in 2016.1 Higher weight is associated with chronic diseases, such as Type 2 diabetes mellitus (T2DM) and cardiovascular disease (CVD). Even modest weight loss of 5 to 10 percent can produce clinically meaningful health improvements,2 yet patients with severe obesity might require more significant intervention than lifestyle change alone is likely to produce. Metabolic and bariatric surgery (MBS) has emerged as the most successful long-term weight loss intervention for those with severe obesity (BMI>40kg/m2, or >35kg/m2 with weight-related comorbidities).3 MBS is a powerful intervention that can bring about the resolution of medical comorbidities and drastically improve quality of life. However, there is variability in outcomes, with a minority (3.4%) of patients experiencing nearly total weight regain within 10 years of the Roux-en-Y gastric bypass (RYGB),⁴ and 15.4 percent of patients experiencing loss-of-control eating 13 to 15 years post-RYGB.⁵ These challenges are more likely to emerge after the “honeymoon period” (first two years) after surgery has passed.⁶ Questions remain about how best to pair surgical intervention with effective, sustainable nutritional and behavioral tools that can facilitate long-term weight loss and a healthier relationship with food.
Limitations of Calorie/Macronutrient Restrictive Diets in MBS Patients
From a nutrition perspective, calorie restriction has long been the gold standard for achieving weight loss in nonsurgical weight management. However, long-term outcomes of these diets reveal that 95 percent of individuals who lose weight through calorie/macronutrient restriction regain the weight within 1 to 2 years, with two-thirds regaining more.2,7,8 Low-fat diets do not lead to long-lasting weight loss,2,9–11 and the evidence for long-term weight loss benefits of low-carbohydrate diets is even weaker than for calorie-restricted diets.12–18
In addition to the likelihood of weight regain, there are significant concerns about the relationship between restrictive diets and eating disorders.20–25 The seminal 1944 semi-starvation study by Ancel Keys demonstrated that food restriction in healthy participants led to preoccupation with food and overeating.19 More recent large-scale studies with long-term follow-up over the last 20 years reveal that restricted eating might lead to short-term weight loss but long-term weight gain,20,21 psychological distress,22 and eating disorder (ED) symptoms, such as skipping meals, purging, taking laxatives/diuretics for weight control, starving, and binge eating.23–25
Chronic dieting is also associated with body dissatisfaction and overvaluation of weight, which are risk factors for lower physical activity and unhealthy eating behaviors,26,27 including binge eating disorder (BED) and loss-of-control-eating, specifically in patients who undergo MBS.28–31 Furthermore, weight cycling associated with dieting is associated with negative health effects.32–37 Most patients seeking MBS have an extensive history of dieting and weight cycling, and high levels of body dissatisfaction.38 On average, patients who undergo MBS have tried an average of 15 diets, and, after a frustrating course of losing and regaining weight, consider surgery to be a “last resort.”39
Indeed, prior to surgery, many patients report a difficult relationship with food manifested as guilt and experiencing a loss of control with eating.40 Therefore, there are concerns that pairing restrictive diets with MBS might put patients at risk of disordered eating or weight regain.
In 2008, the American Society for Metabolic and Bariatric Surgery (ASMBS) Nutrition Committee published the Allied Health Nutritional Guidelines for the Surgical Weight Loss Patient.41 Though these guidelines are comprehensive, they do not include calorie recommendations for patients following MBS, and neither does the 2019 American Dietetic Association Systematic Review of Nutrition in Bariatric Surgery.42 The Academy of Nutrition and Dietetics Pocket Guide to Bariatric Surgery states that patients who have a history of weight cycling might gravitate toward caloric restriction after surgery, but suggests that registered dietitians discourage this practice and instead counsel patients on mindful eating (ME) strategies to foster a healthy relationship with food.43
Mindful and Intuitive Eating
In the last two decades, ME and intiutive eating (IE) have emerged as alternative approaches for stabilizing weight, preventing weight gain, and reducing compulsive eating. ME integrates principles of mindfulness meditation with eating, including curiosity, nonjudgment, and self-compassion. Whereas diets tend to promote “black-and-white thinking” regarding eating, including categorizing foods as “good” and “bad,” and the need for perfect adherence to restrictions to achieve weight loss, ME is a gentler approach that encourages self-compassion for not following rules perfectly, curiosity for less-than-perfect meals, and resilience to assist with long-term maintenance.
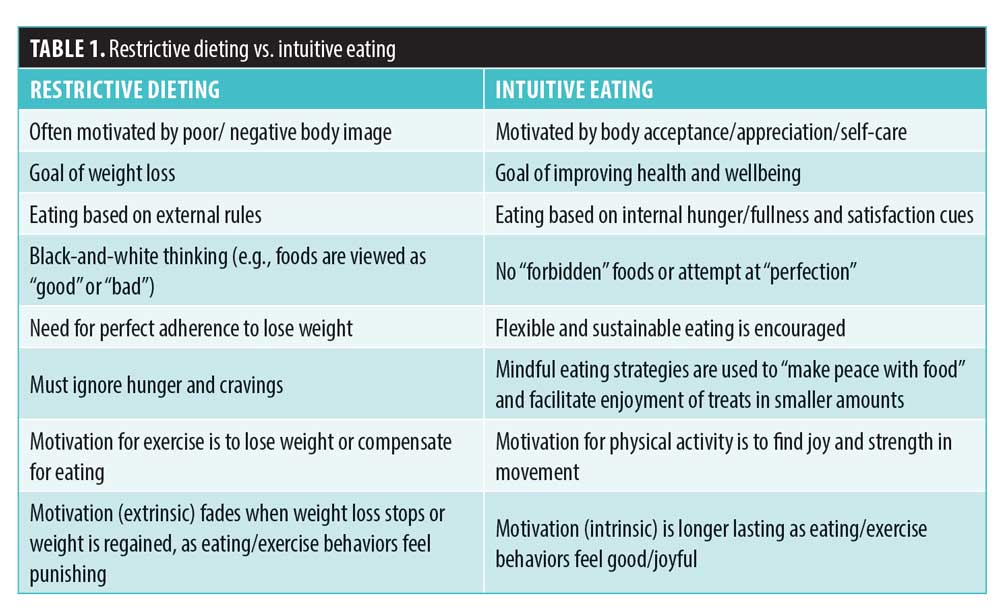
IE is a related eating philosophy that completely shuns any type of restrictive diet. As explained by Tribole and Resch,44 IE involves eating based on internal cues of hunger, fullness, and satisfaction, as opposed to external rules. Using “gentle nutrition,” this approach focuses on the pursuit of health versus weight loss, although reduced weight is acknowledged to be a potential outcome of healthy behavior changes.44 In fact, higher IE is associated with lower BMI.45–47 The four major tenets of IE are unconditional permission to eat, eating for physical rather than emotional reasons, reliance on hunger and satiety cues, and body–food choice congruence.48 Table 1 summarizes the differences between restrictive dieting and IE.
Evidence for ME and IE has been mounting in nonsurgical and ED literature. In a systematic review of 24 studies examining psychosocial correlates of IE among adult women, IE was negatively associated with disordered eating (bulimia, food pre-occupation, binge eating) and emotional distress, and positively associated with body appreciation (e.g., a greater focus on gratitude for the body’s functions rather than appearance).49 Among university students and women, research consistently shows that IE is associated with a lower BMI.50 A systematic review of mindfulness-based interventions also yielded strong evidence for ME in reducing binge eating.51
IE and ME have shown promise in weight management contexts as well. In a systematic review of 20 IE intervention studies in nonsurgical patients without EDs, those who participated in IE interventions (vs. controls) had greater physical activity, less disordered eating, a more positive body image, and reduced psychological distress.52 Although IE is focused on health rather than weight, significant weight loss or weight maintenance was observed in all but one study reviewed. Even when participants in IE interventions maintained weight, maladaptive eating behaviors, psychological functioning, and some cardiometabolic parameters improved. These results align with other research suggesting a relationship between IE and physical health indicators (e.g., blood pressure, cholesterol).50 Taken together, research suggests there is “strong support for inclusion of ME as a component of weight management programs.”53
Although ME and IE have been examined in nonsurgical weight management and ED populations, they have received much less attention in MBS literature. It has been proposed that these approaches might be more beneficial than dieting specifically in the MBS population.54 On the other hand, it could be difficult for patients to be guided by internal hunger/fullness cues following MBS due to the physical alteration of these signals induced by the surgery. The present study sought to examine the relationship between IE and several domains thought to reflect a healthy relationship with food. It was hypothesized that participants exhibiting higher levels of IE would evidence less emotional eating, feel more in control of eating, have a greater tendency to use mindful eating strategies, feel more satisfied with meals, be more likely to choose foods and portions based on hunger/fullness cues rather than external rules, be more likely to practice regular self-care, and feel more confident in their ability to maintain their eating behaviors and weight long-term.
Methods
At the University of Massachusetts Memorial Bariatric Center, the nutrition counseling pre- and postsurgery integrates principles of IE and ME. At the time of data collection, 270 patients were members of a private Facebook support group, where they were invited to participate in an online survey consisting of the Intuitive Eating Scale-2 (IES-2), Emotional Overeating Questionnaire (EOQ), and a questionnaire designed for this study. This study was approved by the Institutional Review Board (IRB).
Measurements
Intuitive Eating Scale-2. The IES-2 is a 23-item scale designed to measure the tendency to eat based upon hunger/fullness cues.48 Items are rated from 1 (strongly disagree) through 5 (strongly agree), yielding a total average score as well as four subscales (Unconditional Permission to Eat, Eating for Physical Rather than Emotional Reasons, Reliance on Hunger and Satiety Cues, and Body-Food Choice Congruence). The IES-2 has demonstrated adequate validity and reliability (Cronbach’s alpha coefficients ranging from 0.81 to 0.89).48 The total score was used in this study.
Emotional Overeating Questionnaire. The EOQ is a 6-item questionnaire measuring the frequency one overeats in response to anxiety, sadness, loneliness, tiredness, anger, and happiness.55 Respondents estimate how many days out of the past 28 days overeating occurred in response to these six emotions, from 0 (no days) through 6 (every day), yielding a total average score. The EOQ has demonstrated adequate convergent validity and reliability (alpha=0.85).
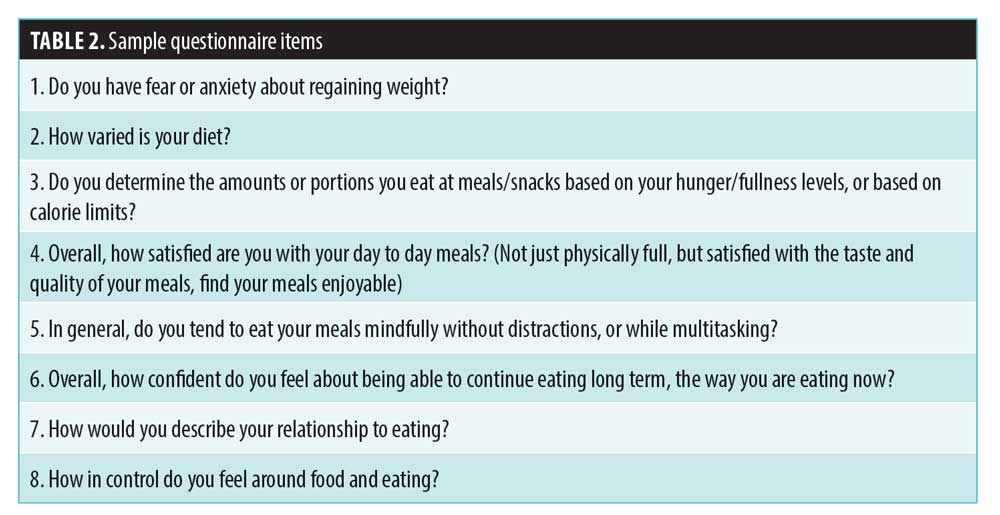
Study questionnaire. An additional questionnaire designed for this study included questions about demographics, various eating behaviors, self-efficacy, and self-care. Items were multiple choice (e.g., often, sometimes, rarely, never) or rated on Likert scales (e.g., not at all confident, somewhat confident, very confident). Table 2 lists questionnaire items relevant to the study’s hypotheses.
Data analysis. Dichotomous variables were analyzed using linear regression using a general linear model, with IES scores entered as the dependent variable. Variables were entered separately into their own models. Pearson correlation was used to explore the relationship between IE and EE.
Results
A total of 90 patients who underwent bariatric surgery responded to the online questionnaire. Response rate was 33 percent of online support group members. The final sample was 77.8 percent female, 92.0 percent Caucasian, 6.8 percent Latino/a, and 1.1 percent African American. The average age was 49.6 years (range=23–75 years, standard deviation [SD]=10.90 years). Mean BMI was 37.1kg/m2 (range=26–53kg/m2, SD=6.40). Time since surgery ranged from three months (20%) to more than five years (4.4%) with most participants in the 3-to-11-month range (40.7%). Men tended to have higher IE scores than women (p=0.02). There were no significant differences by age or racial/ethnic group. Although we did not collect data on the type of MBS procedures that the subjects in this study underwent, most patients at the UMass Memorial Bariatric Center (95%) undergo vertical sleeve gastrectomy (SG), with a small number of patients (5%) going through RYGB.
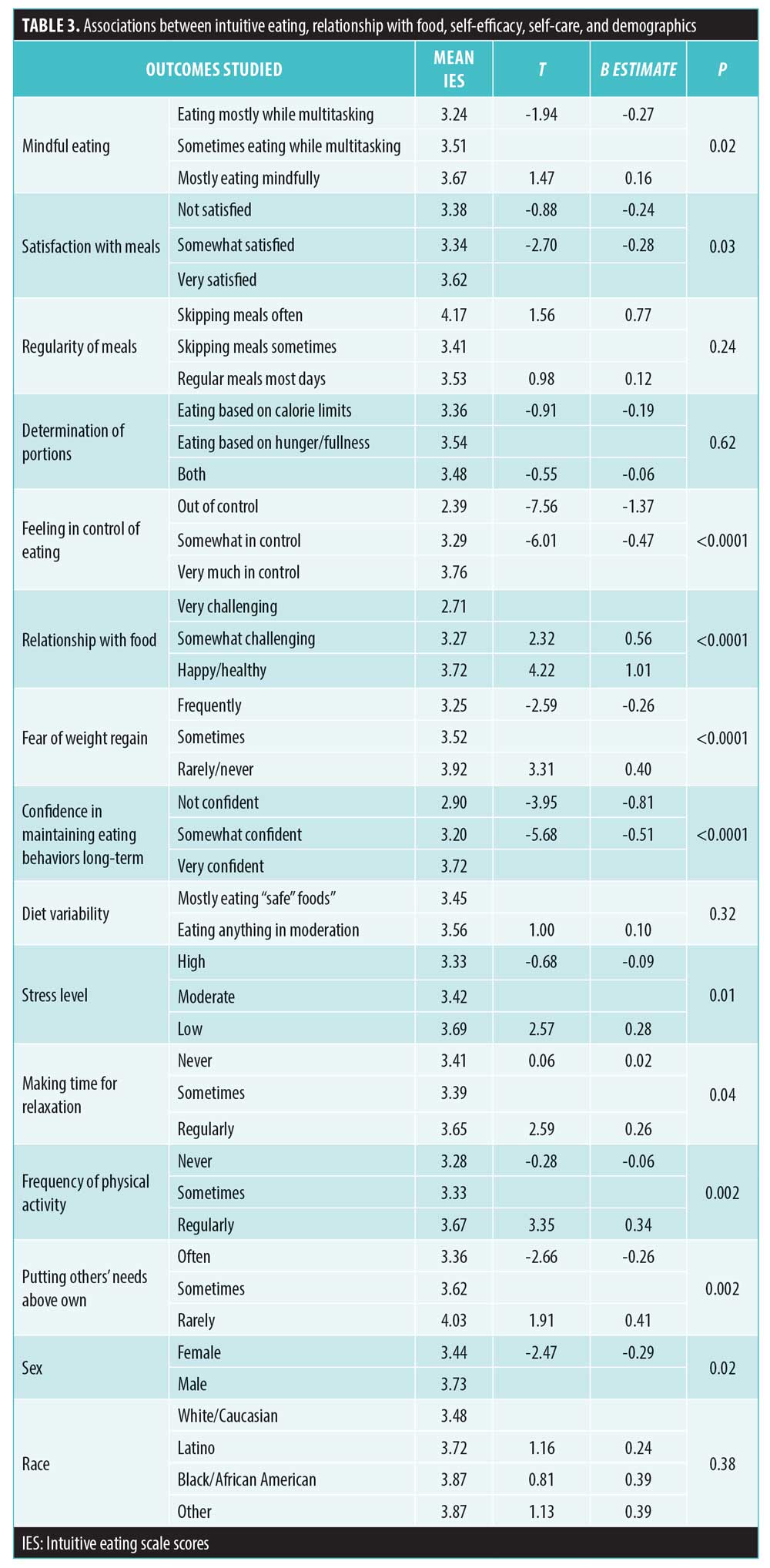
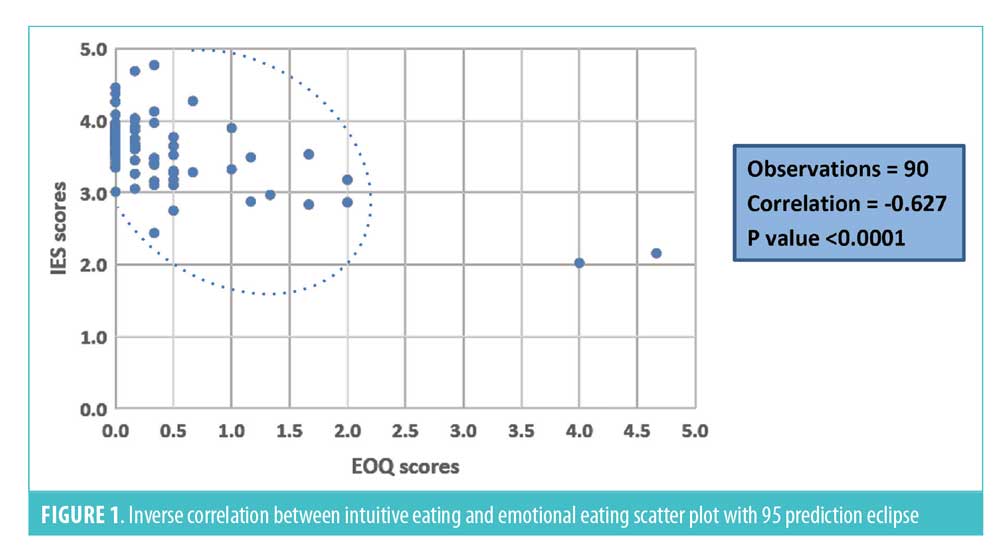
Mean IES score in the sample (N=90) was 3.51 (SD=0.48). Table 3 lists means, B estimates, and t-values for categorical independent variables related to relationship with food, self-efficacy, and self-care. Higher IE scores were significantly positively associated with satisfaction from meals (p=0.03), mindful eating (p=0.02), confidence in maintaining eating behaviors longterm (p<0.0001), feeling in control of eating (p<0.0001), having a positive relationship with eating (p<0.0001), making time for relaxation (p=0.04), and engaging in regular physical activity (p=0.002). IE was negatively associated with fear of weight regain (p<0.0001) and stress (p=0.01). IE was found to be inversely correlated to emotional eating, (r [88]= -0.63, p<0.0001, Figure 1). Unexpectedly, IE was not significantly associated with diet variety nor determining portions based on hunger/fullness levels.
Discussion
The weight loss journey of the average bariatric patient begins years before they begin an MBS program. Bariatric patients have tried an average of 15 diets, some with short-term success and ultimately weight regain.39 Over time, this “yo-yo dieting” causes adverse physiological and psychological consequences, including becoming disconnected with interoceptive hunger/fullness cues, guilt and anxiety around eating, and meal skipping. These results suggest that IE might be useful in mitigating these consequences and helping patients to develop a healthier relationship with food.
The intuitive and mindful eating experience. Results indicate that participants who embodied IE principles were more likely to report consuming meals mindfully, without distractions, rather than eating when multitasking or distracted. Participants who embodied IE principles also rated higher satisfaction from meals, as defined by feeling physically full, as well as deriving enjoyment from the taste and quality of meals. These results make sense given that ME is a key aspect of IE philosophy. Patients who undergo MBS who consume meals that are satisfying to them might be better able to savor food slowly without distraction, which is important in reducing portions and physical discomfort. Indeed, ME interventions have been shown to reduce “external eating,” or eating based on external cues such as the sight or smell of food.56 In addition, those with higher levels of IE have been found to experience greater pleasure in eating,57 perhaps because it is easier to appreciate the taste of food when one is making choices that are satisfying. Unconditional permission to eat, a tenet of IE, could be a prerequisite for facilitating ME, as it is difficult to eat a food mindfully while vowing to not eat it again.
Unexpectedly, IE was not significantly associated with eating based on hunger/fullness cues versus calorie limits. While research in non-MBS patients indicates that ME and IE are associated with making choices regarding portions and types of food based upon hunger, fullness, and satisfaction, there could be differences in the MBS experience.58 Those who have had MBS have altered hunger/fullness sensations, and, in fact, might need to eat when not physically hungry to meet nutritional needs, at least in the initial months or years following surgery. Likewise, IE was not significantly associated with diet variability versus consuming mostly “safe” foods. Again, patients who undergo MBS might be more limited in their food choices due to their MBS program’s recommendations regarding when to advance diet stages postsurgery, initial food intolerances, and prioritizing protein intake.
Emotional and loss-of-control eating. Results suggest that IE is associated with feeling more in control of eating and engaging in less emotional eating. These results are consistent with previous research indicating that higher IE is related to fewer BED symptoms, and that participants in IE interventions are less likely than wait list controls to have ED pathology.49,52,59–61 Likewise, ME training has been shown to be an effective intervention for BED.51,62 Thus, while some patients and providers might assume that rigid control of food intake is needed to prevent overeating, a gentler approach might actually reduce eating pathology, especially given that “food policing” seems to bring out the “inner rebel,” leading to sneaking and hiding food.44
The results of this study make sense when considering the psychological effects of chronic dieting and rigid control. Diets often place food into categories of “good” and “bad,” and while patients consume only the “good” or “safe” foods when motivated to lose weight, preoccupation with thoughts of “forbidden” foods might increase. Vowing to just eat these foods “one last time” when they become available leads to a perception of future deprivation, contributes to overeating in the present, and ultimately results in guilt and shame due to perceived “lack of control.” In other words, when restraint is broken during times of increased vulnerability, stress, or change, it might lead to counter-regulatory eating (also known as “what the hell effect” in popular culture), leading to “falling off the wagon” and a consequent vow to exert more control in the future. Trying to compensate overeating by undereating the next day might worsen subsequent overeating by leading to primal hunger.44
In contrast, those with an IE mindset know they can consume as much of any desired food as satisfies them at any time, which could be smaller portions on some days, larger portions on other days, and none on others. The consequences of overindulgence (e.g., physical discomfort) can create a natural aversion to overeating those foods in the future over time. This process, called “habituation,” a form of learning in which repeated exposure to a stimulus leads to decreased response, occurs repeatedly in those following an IE approach and slowly tempers the allure of highly palatable foods with time.44,63 Strict dieters, on the other hand, who do not have the opportunity to become habituated, continue to feel food insecurity and intense cravings. Thus, whereas the desire for rigid control on diets can have the opposite of the intended effect, results of the present study suggest that IE is associated with greater perceived ability to control food intake, and might especially be helpful in patients who undergo MBS due to the possible reoccurrence of loss of control eating postsurgery.5 For individuals who have a deep-rooted pattern of emotional eating, restrictive eating recommendations might only worsen this tendency as food feels more rewarding, not less, in a state of hunger and deprivation.
Self-efficacy. Results suggest that participants who embody IE principles feel more confident in their ability to maintain current eating behaviors long-term and have less fear of weight regain. In other words, those with greater IE appear to have greater self-efficacy around their ability to maintain eating behaviors and weight over time. Other research highlights the importance of self-efficacy in weight management, suggesting that greater self-efficacy is associated with greater weight loss and better weight-loss maintenance in non-surgical samples.64 Not surprisingly, chronic dieting is associated with lower self-efficacy, which underscores the need to help patients who undergo MBS, who have tried many previous diets, to boost confidence in their ability to maintain lifestyle changes.64,39
The nonsurgical literature suggests that IE and ME could help increase self-efficacy. For example, Timmerman and Brown65 found that non-surgical patients who participated in an ME intervention had increased self-efficacy (e.g., confidence they could maintain eating behaviors consistently for at least six months) and decreased perceived barriers to weight management. Based upon the results of the present study, patients who undergo MBS with greater levels of IE perceive their eating behaviors as more feasible to maintain longterm as well.
Self-care. Results indicated that participants who embody IE principles have lower perceived stress, engage in physical activity more regularly, make more time for rest/relaxation, and are less likely to prioritize others’ needs before their own. These results are consistent with previous research suggesting a relationship between IE and greater proactive coping, lower depression and negative affect, and better stress management behaviors.45,59,60,66,67 In fact, Van Dyke and Drinkwater’s50 systematic review of IE and health indicators concluded, “the clearest positive association between IE and health outcomes is with psychological health.” Present results also add to the body of literature regarding the relationship between IE and physical activity, which to this point has been mixed. Whereas some studies have found a significant positive correlation between physical activity and IE, several others have not.50,58 It is unclear whether IE principles are easier to follow when practicing better self-care, whether IE itself motivates one to practice better self-care or whether some other factor contributes to this relationship. However, it is possible that whereas more restrictive eating and externally motivated exercise contributes to greater pressure and stress, IE provides a more positive experience. Indeed, rather than focusing on exercise to burn calories, IE encourages finding joy and pleasure in movement.44
Implications and Recommendations
Overall, patients who undergo MBS and embody IE principles feel more in control of their eating and confident about maintaining behaviors long-term. IE principles can be adapted for MBS populations and integrated into pre- and postsurgical nutritional and behavioral counseling.
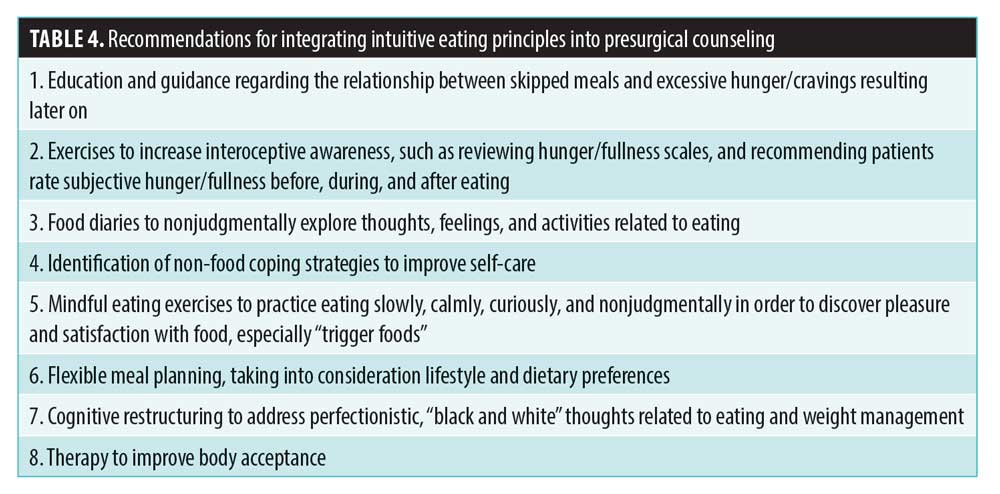
Presurgical counseling. Presurgical counseling involves shifting the focus from dieting or strict weight loss requirements to developing a healthy, sustainable lifestyle that prepares patients for a healthy adjustment to surgery. For many patients, this counseling involves helping them to reduce meal skipping and the primal hunger resulting from it. Patients are asked to experiment with eating regular meals slowly and mindfully, and then observe changes in their hunger, cravings, portions, energy levels, and vulnerability to emotional eating. Table 4 includes topics that may be integrated into presurgical counseling to develop skills for maintaining long-term healthy eating behaviors.
Clinical observation suggests that when patients are given the freedom to decide portions/choices based on comfort and satisfaction, and asked to eat regular meals mindfully, without excessive focus on calories or weight loss, they tend to gravitate toward nutritious choices, habituate with highly palatable foods, and feel more confident and in control of eating. Modest presurgical weight loss, which might not be the primary goal, is often the natural side effect of developing a healthier relationship with food.
Postsurgical counseling. After surgery, education and intervention are similar, with individualized nutrition counseling to ensure that each patient is meeting their nutritional needs to prevent malnutrition. During the first few weeks and months following surgery when patients are adjusting to increased restriction and reduced hunger hormones, IE approaches need to be adapted to assist patients in relearning hunger/fullness cues. Early introduction of IE principles can facilitate a return to this approach long-term once hunger and fullness cues have been re-established.
Traditionally, there has been a tendency among well-intentioned MBS clinicians to give postsurgical diet recommendations that restrict calories and food groups (mostly carbohydrates), in addition to the restriction created by the surgical procedure. The intense fear of weight gain among patients who see surgery as their “last resort” (likely driven by years of being subjected to weight bias) seems to drive them to try to strictly adhere to these recommendations but ultimately feel they have “failed” to live up to what may be unrealistic expectations. For some patients, this might lead to re-entering the same restrict-binge cycle that contributed to weight gain before surgery.
Instead of calorie-counting, patients are encouraged to decide meal amounts and choices while balancing nutrition with their personal comfort and satisfaction levels, without forbidding what they might have previously perceived as “bad” foods, for these reasons:
Calorie needs tend to differ person to person based on age, gender, weight, physical activity, and time elapsed since surgery
There is no scientific consensus on calorie recommendations post-surgery41–43
The restrictive effects of the MBS procedure might vary from person to person
Specific nutrition guidelines are individualized, with the following general recommendations:
Avoid skipping meals. Eat regular meals (4–5 small meals a day in the first few months postsurgery, 3–4 meals per day as time since surgery and appetite increase), making choices that are comfortable, satisfying, and as nutritious as possible. Allow time gaps of a few hours between meals to establish clear hunger and fullness signals with time.
Eat when comfortably hungry, don’t wait till famished, and stop when feeling comfortably full. If one does not feel hungry initially, eat an amount of food that feels comfortable, approximately every three hours, until hunger signals return.
Eat slowly, without distractions, while chewing well.
Eat balanced meals and snacks that contain all major nutrients: protein, carbohydrates, and dietary fat, with a special emphasis on protein, and mostly preferring whole grains and complex carbohydrates to refined ones as much as possible.
Consume adequate water and other unsweetened, noncarbonated beverages.
Realistic goal setting focused on these healthy behaviors rather than weight loss itself could assist in broadening patients’ definition of “success” following MBS. Weight loss treatments should target all aspects of lifestyle, given that the etiology of weight gain and its associated morbidities is multifactorial and biopsychosocial and includes social determinants of health with the understanding that some factors might be out of one’s control.68 If too much importance is placed on weight loss expectations and “adherence” on the part of the patient, it could lead to discouragement and self-blame. In contrast, a compassionate approach might promote resilience in the pursuit of health even if weight loss results are suboptimal. Moreover, integrating IE postoperatively might not lead to the same degree of rapid weight loss as restrictive eating, but it might be conducive to modest yet sustainable weight loss, physical and mental health benefits, and a healthy relationship with eating.
Limitations
Results of the present study must be considered in light of the study’s limitations. First, research was correlational in nature, and thus, conclusions about causality cannot be drawn. Intervention studies are needed to further clarify the relationship between IE and other variables (e.g., self-care, ED pathology) at various points pre- and post-MBS, and to explore the relationship between IE and long-term weight loss outcomes. Second, the sample was drawn from an online support group for an MBS program in which IE principles are integrated into pre- and postoperative nutrition counseling. Thus, while there was variability in this sample’s IE scores, results might not generalize to patients who undergo MBS in other programs that do not emphasize an IE approach. It would be helpful to replicate this study in another MBS setting with a larger sample size and with greater variability in time since surgery. Finally, the study questionnaires relied only on self-reporting, and several questionnaire items were designed specifically for this study rather than drawn from previously validated instruments. Future research using more precise measures is needed to examine food intake/nutritional status as it relates to IE in patients who undergo MBS.
Conclusion
In conclusion, integrating IE with MBS might seem contradictory on the surface, especially given that the surgical procedure could alter hunger and fullness sensations initially. However, results of the present study suggest that IE can assist patients in developing a healthier relationship with eating. Postsurgical patients who have higher levels of IE tendencies report feeling more in control of their eating, feel more mindful and satisfied with meals, engage in less emotional eating, feel more confident in their ability to maintain eating behaviors long-term, and engage in better selfcare overall. While some people might believe that IE means “eating whatever you want, whenever you want,” it is more accurate to describe it as a means of curiously and mindfully respecting internal cues, fostering body trust, focusing on health rather than weight, and finding a manner of eating that feels more sustainable than rigid diets. Food is not just a source of fuel and nutrition for humans, but also comfort, celebration, and a link to our childhood, culture, and roots. Therefore, a flexible eating approach that honors these needs might be more sustainable than a rigid, depriving one that focuses solely on nutrition. Restriction might lead to compulsion and rebellion, while permission might lead to choice. It might seem counterintuitive, but IE promotes food choices that are more nutritious and higher quality.69
Research regarding IE in nonsurgical populations is burgeoning, but it is essentially unexamined in the bariatric population. Intervention studies are needed to further examine the efficacy and utility of IE approaches before and after MBS, as well as the relationship between IE and long-term outcomes.
The authors would like to end this paper by asking the reader to think critically about this scenario: X and Y were two friends working in an office. X was trying to lose weight, while Y was not. At lunch time one day, both were craving a sandwich. Y had a sandwich and enjoyed every bite of it, slowly and mindfully. X decided a salad was a “better choice,” but was not in the mood for it that day, so he ate it while checking his email, just to “get it over with.” Half an hour later, a coworker brought a platter of donuts to celebrate someone’s birthday. Between X and Y, who was more likely to give in and eat the donut?
References
- Hales C, Carroll M, Fryar CD, et al. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief. 2017;288:1–8.
- Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guidelines for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 PtB B):2985–3023.
- Arterburn DE, Olsen MK, Smith VA, et al. Association between bariatric surgery and long-term survival. JAMA. 2015;313(1):62–70.
- Maciejewski ML, Arterburn DE, Van Scoyoc L, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016;151(11):1046–1055.
- Mitchell JE, Lancaster KL, Burgard MA, et al. Long-term follow-up of patients’ status after gastric bypass. Obes Surg. 2001;11(4):464–468.
- Chao AM, Wadden TA, Faulconbridge LF, et al. Binge-eating disorder and the outcome of bariatric surgery in a prospective, observational study: two-year results. Obesity. 2016;24(11): 2327–2333.
- Mann T, Tomiyama AJ, Westling E., et al. Medicare’s search for effective obesity treatments: diets are not the answer. Am Psychol. 2007;62(3):220–233.
- Katan M. Weight-loss diets for the prevention and treatment of obesity. N Engl J Med. 2009;360:923–925
- Willett WC, Leibel RL. Dietary fat is not a major determinant of body fat. Am J Med. 2002;113 Suppl 9B:47S–59S.
- Howard BV, Manson JE, Stefanick ML, et al. Low-fat dietary pattern and weight change over 7 years: The Women’s Health Initiative Dietary Modification Trial. JAMA. 2006;295(1):39–49.
- Tobias DK, Chen M, Manson JE, et al. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3(12):968–979.
- Fields H, Ruddy B, Wallace MR, et al. Are low-carbohydrate diets safe and effective? J Am Osteopath Assoc. 2016;116(12):788–793.
- Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med. 2003;348(21):2082–2090.
- Nordmann AJ, Nordmann A, Briel M, et al. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med. 2006;166(3):285–293.
- Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360(9):859–887.
- Siedelmann SB, Claggett B, Chen S. et al. Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. Lancet. 2018;3(9):419–428.
- Kirkpatrick CF, Bolick JP, Kris-Etherton PM, et al. Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: a scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J Clin Lipidol. 2019;13(5):689–711.
- Reynolds A, Mann J, Cummings J, et al. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet. 2019;393(10170):434–445.
- Keys A, Brozek J, Henschel A. The Biology of Human Starvation I–II. Minneapolis, MN: University of Minnesota Press; 1950.
- Field AE, Austin SB, Taylor CB, et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003;112(4):900–906.
- Pietiläinen KH, Saarni SE, Kaprio J, Rissanen A. Does dieting make you fat? A twin study. Int J Obes. 2012;36(3):456–464.
- Ackard DM, Croll JK, Kearney-Cooke A. Dieting frequency among college females: association with disordered eating, body image, and related psychological problems. J Psychosom Res. 2002;52(3):129–136.
- Cachelin FM, Regan PC. Prevalence and correlates of chronic dieting in a multi-ethnic U.S. community sample. Eat Weight Disord. 2006;11(2):91–99.
- Neumark-Sztainer D, Wall M, Guo J. et al. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? J Am Diet Assoc. 2006;106(4):559–568.
- Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychol. 2002;21(2):131–138.
- Neumark-Sztainer N, Paxton S, Hannan PJ, et al. Does body satisfaction matter? Five-year longitudinal associations between body satisfaction and health behaviors in adolescent females and males. J Adolescent Health. 2006;39(2):244–251.
- Bouzas C, Bibiloni MDM, Tur JA. Relationship between body image and body weight control in overweight ≥55-year-old adults: a systematic review. Int J Environ Res Public Health. 2019;6(9):1622.
- Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull. 2002;128(5):825–848.
- Stice E, Gau JM, Rohde P, et al. Risk factors that predict future onset of each DSM-5 eating disorder: predictive specificity in high-risk adolescent females. J Abnorm Psychol. 2017;126(1):38–51.
- Stice E, Van Ryzin MJ. A prospective test of the temporal sequencing of risk factor emergence in the dual pathway model of eating disorders. J Abnorm Psychol. 2019;128(2):119–128.
- Ivezaj V, Wiedemann A, Grilo CM. Overvaluation of weight or shape and loss‐of‐control eating following bariatric surgery. Obesity. 2019;27(8):1239–1243.
- Saarni SE, Rissanen A, Sarna S, et al. Weight cycling of athletes and subsequent weight gain in middle-age. Int J Obes. 2006;30(11):1639–1644.
- Montani JP, Schutz Y, Dulloo AG. Dieting and weight cycling as risk factors for cardiometabolic diseases: who is really at risk? Obes Rev. 2015;16(1):7–18.
- Field AE, Manson JE, Taylor CB, et al. Association of weight change, weight control practices, and weight cycling among women in the Nurses’ Health Study II. Int J Obes Relat Metab Disord. 2004;28(9):1134–1142.
- Oh TJ, Moon JH, Choi SH, et al. Body-weight fluctuation and incident diabetes mellitus, cardiovascular disease, and mortality: a 16-year prospective cohort study. J Clin Endocrinol Metab. 2019;104(3):639–646.
- Kim MK, Han K, Park YM, et al. Associations of variability in blood pressure, glucose and cholesterol concentrations, and body mass index with mortality and cardiovascular outcomes in the general population. Circulation. 2018;138(23):2627–2637.
- Byun S, Bello NA, Liao M, et al. Associations of weight cycling with cardiovascular health using American Heart Association’s Life’s Simple 7 in a diverse sample of women. Prev Med Rep. 2019;116:1–7.
- Bertoletti J, Aparicio MJG, Bordignon S, et al. Body image and bariatric surgery: A systematic review of literature. Bariatr Surg Pract Patient Care. 2019;14(2):81–92.
- Gibbons LM, Sarwer DB, Crerand CE, et al. Previous weight loss experiences of bariatric surgery candidates: how much have patients dieted prior to surgery? Obesity. 2006;14(2):70–76.
- Niego SH, Kofman MD, Weiss JJ, et al. Binge eating in the bariatric surgery population: a review of the literature. Int J Eat Disord. 2007;40(4):349–359.
- Aills L, Blankenship J, Buffington C, et al. ASMBS allied health nutritional guidelines for the surgical weight loss patient: allied health sciences section ad hoc nutrition committee. Surg Obes Relat Dis. 2008;4: S73-S108.
- Andromalos L, Crowley N, Brown J, et al. Nutrition care in bariatric surgery: an Academy Evidence Analysis Center systematic review. J Acad Nutr Diet. 2019;119(4):678–686.
- Cummings S, Isom K. Nutrition care during weight stabilization. In: Cummings S, Isom K (eds). Academy of Nutrition and Dietetics Pocket Guide to Bariatric Surgery, Second Edition. US. 2016:86–102.
- Tribole E, Resch E. Intuitive eating: a revolutionary program that works. New York, NY: St Martin’s Griffin;2012.
- Tylka TL, Wilcox JA. Are intuitive eating and eating disorder symptomatology opposite poles of the same construct? J Couns Psychol. 2006;53(4):474–485.
- Hawks S, Madanat H, Hawks J, et al. The relationship between intuitive eating and health indicators among college women. Am J Health Educ. 2005;36(6):331–336.
- Denny KN, Loth K, Eisenberg ME, et al. Intuitive eating in young adults. Who is doing it, and how is it related to disordered eating behaviors? Appetite. 2013;(60)1:13–19.
- Tylka TL, Kroon Van Diest AM. The Intuitive Eating Scale-2: item refinement and psychometric evaluation with college women and men. J Couns Psychol. 2013;60(1):137–153.
- Bruce LJ, Ricciardelli LA. A systematic review of the psychosocial correlates of intuitive eating among adult women. Appetite. 2016;96:454–472.
- Van Dyke N, Drinkwater E. Relationships between intuitive eating and health indicators: a literature review. Public Health Nutr. 2014;17(8):1757–1766.
- Warren J, Smith N, Ashwell M. Structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviors: effectiveness and associated potential mechanisms. Nutr Res Rev. 2017;30(2):272–283.
- Schaefer JT, Magnuson AB. A review of interventions that promote eating by internal cues. J Acad Nutr Diet. 2014;114(5):734–760.
- Dunn C, Haubenreiser M, Johnson M, et al. Mindfulness approaches and weight loss, weight maintenance, and weight regain. Curr Obes Rep. 2018;7(1):37–49.
- May M, Furtado M, Ornstein LB. The mindful eating cycle: preventing and resolving maladaptive eating after bariatric surgery. Bariatric Times. 2014;11(2):8–12.
- Masheb R, Grilo C. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. Int J Eat Disord. 2006;39:141–146.
- O’Reilly G, Cook L, Spruijt-Metz D, et al. Mindfulness-based interventions for obesity-related eating behaviors: a literature review. Obes Rev. 2014;15(6):453–461.
- Smith TS, Hawks SR. Intuitive eating, diet composition, and the meaning of food in healthy weight promotion. Am J Health Educ. 2006;37(3):130–136.
- Bacon L, Stern JS, Van Loan MD, et al. Size acceptance and intuitive eating improve health for obese, female chronic dieters. J Am Diet Assoc. 2005;105(6):929–936.
- Hazzard V, Telke SE, Simone M, et al. Intuitive eating longitudinally predicts better psychological health and lower use of disordered eating behaviors: findings from EAT 2010–2018. Eat Weight Disord. 2020 Jan 21. Online ahead of print.
- Tylka TL, Calogero RM, Daníelsdóttir S. Is intuitive eating the same as flexible dietary control? Their links to each other and well-being could provide an answer. Appetite. 2015;95:166–175.
- Bush H, Rossy L, Mintz LB, et al. Eat for life: a work site feasibility study of a novel mindfulness-based intuitive eating intervention. Am J Health Promot. 2014;28(6):380–388.
- Kristeller J, Wolever R, Sheets V. Mindfulness-based eating awareness training (MB-EAT) for binge eating: a randomized clinical trial. Mindfulness. 2013;5(3):282–297.
- Epstein L, Carr, K, Cavanaugh MD. Long-term habituation to food in obese and nonobese women. Am J Clin Nutr. 2011;94(2):371–376.
- Bas M, Donmez S. Self-efficacy and restrained eating in relation to weight loss among overweight men and women in Turkey. Appetite. 2009;52:209–216.
- Timmerman GM, Brown A. The effect of a mindful restaurant eating intervention on weight management in women. J Nutr Educ Behav. 2012;44:22–28.
- Iannantuono AC, Tylka TL. Interpersonal and intrapersonal links to body appreciation in college women: an exploratory model. Body Image. 2012;9(2):227–235.
- Hawley G, Horwath C, Gray A, et al. Sustainability of health and lifestyle improvements following a non-dieting randomized trial in overweight women. Preventative Medicine. 2008;47:593–599.
- CDC Health Disparities and Inequalities Report-United States, 2011. MMWR 2011;60[Suppl; January 14, 2011].
- Carbonneau E, Begin C, Lemieux S, et al. A Health at Every Size intervention improves intuitive eating and diet quality in Canadian women. Clinical Nutrition. 2017;36(3):747–754.
Category: Original Research, Past Articles




