Support Group for Adolescents Undergoing Bariatric Surgery: Preliminary Data and Suggestions for Providers
 by Melissa Santos, PhD, and Christine Finck, MD
by Melissa Santos, PhD, and Christine Finck, MD
Drs. Santos and Finck are with Connecticut Children’s in Hartford, Connecticut.
FUNDING: No funding was provided.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Objective. Adolescent bariatric surgery is becoming an increasingly used obesity management tool. Support groups are often recommended as part of care, but little research has examined the impact of a support group on outcomes or evidence-based best practices for conducting these groups.
Design. The charts of 10 adolescent patients who underwent the laparoscopic adjustable gastric banding procedure were examined to describe support group attendance and short-term weight outcomes. In addition, strategies for implementing support groups are offered.
Setting. The location of the study was a free-standing 187-bed children’s hospital in the Northeast United States.
Participants. Adolescents between the ages of 14 to 19 years undergoing bariatric surgery were included.
Measurements. Demographic information (gender, age, race/ethnicity), support group attendance (postbariatric surgery), weight loss (body mass index, weight).
Results. Adolescents who attended two or more support groups in the first six months after surgery lost more weight than those who did not attend a support group at all or only attended one. Baseline differences were seen with adolescents who were older and heavier being less likely to attend a support group. This could be that those adolescents who are older or heavier might feel uncomfortable attending a group session.
Conclusion. Preliminary data in this small subset of patients shows that a support group for adolescents undergoing bariatric surgery can be a helpful tool in achieving successful short-term (six-month) postsurgical weight loss. More research is needed on the process of running successful support groups, examining long-term outcomes (past six months) and identifying which adolescents most benefit from attendance at a support group.
KEYWORDS: support group, adolescent bariatric surgery, adjustable gastric banding, adherence
Bariatric Times. 2021;18(5):10–11.
Within the United States, approximately 17 percent of youth have obesity, while nearly 32 percent have either obesity or overweight.1 More specifically, 5.9 percent of youth meet criteria for Class 2 obesity (body mass index [BMI]≥120% of the 95th percentile for age and sex or BMI≥35kg/m2) and 2.1 percent for Class 3 obesity (BMI≥140% of the 95th percentile or BMI≥40kg/m2).2 Given the persistence of severe obesity, together with its associated medical and psychosocial comorbidities, bariatric surgery has become increasingly used as a method of intervention for youth with Class 2 and 3 obesity. Recent trends show a significant increase in the use of bariatric surgery in adolescents with lower risk of complications than adults.3 This is critical because research is also finding that youth are presenting to obesity clinics at increasingly higher weights and with more obesity-related comorbidities.4
Expert committee recommendations and guidelines for adolescent bariatric surgery programs exist.5–7 These guidelines, as well as the American Society for Metabolic and Bariatric Surgery’s (ASMBS) adult practice guidelines, recommend support groups as an important component of bariatric surgery programs.8 The importance of participation in a support group is highlighted in the adult literature, as attendance at support groups is related to greater weight loss, maintenance of weight loss, program adherence, and peer connections.9–12 Despite this, the most recent recommendations from ASMBS on adolescent bariatric surgery do not mention the utilization of support groups.13
In part, this might be because little research has examined the role of a support group in adolescents undergoing bariatric surgery. A search of the recent literature finds only one article that examines the outcomes from conducting an adolescent bariatric support group. Sawhney et al14 found that attendance at adolescent bariatric support groups was correlated with a greater likelihood of attendance for scheduled postoperative in person clinic visits. The authors were able to identify some characteristics of nonattendees—namely adolescents with higher preoperative BMIs and those with a parent or caregiver who had bariatric surgery were less likely to attend a support group. A recent survey of adolescent bariatric programs found support groups to be a competent component that works to retain patients and their families in treatment.15
Given the little research that has examined support group attendance in youth undergoing bariatric surgery, or its relationship to weight outcomes, the goal of this brief report is to add to the limited research by describing preliminary data from a small subset of youth who underwent the laparoscopic adjustable gastric banding procedure. Support group attendance and differences in short-term weight outcomes are described. Strategies for incorporating a support group into clinical practice are offered.
Methods
Institutional Review Board (IRB) approval from a free-standing children’s hospital in the Northeast was obtained, and patients were acquired from either a retrospective chart review or a prospective database. The minimum criteria for entering the bariatric surgery program is a BMI at, or greater than, 40kg/m2 or a BMI between 35 and 39kg/m2 with a medical comorbidity, such as Type 2 diabetes mellitus, hypertension, or obstructive sleep apnea. During the time this data was collected, patients had to be at least 14 years of age to enter the bariatric surgery program. To qualify for surgery, patients must show adherence to the treatment protocol, including attending a minimum of six consecutive nutrition appointments and attending at least one support group. Patients were included in this sample if they (a) underwent the laparoscopic adjustable gastric banding procedure and (b) attended a bariatric appointment six months after surgery.
Results
Demographic information. The sample consisted of eight female patients and two male patients. Their ethnicity/race was Brown/Hispanic (five); White/Caucasian (three) and Black/African American (two). Upon entry into the bariatric surgery program, the average starting weight was 131.43kg (302.29lbs) and the average starting age was 16.8 years. The average starting BMI was 47.9kg/m2.
Support group attendance. Bariatric support groups are held monthly and are led by a pediatric psychologist and/or registered dietitian. The support group is open to patients and their families. Prior to surgery, the average number of support groups attended across the sample was 3.2. In the first six months after surgery, the average number of support groups attended was 1.6.
Weight changes after surgery. At six months post surgery, the average weight was 115.11kg (253.24lbs). The average BMI at six months post surgery was 42.25kg/m2. When compared to their starting weight and BMI, this is a reduction of 16.32kg (49.05lbs) and 5.65 BMI points.
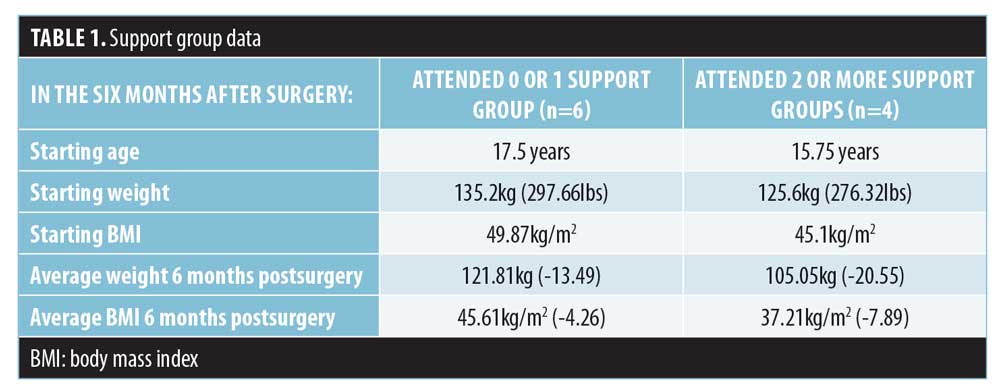
Comparing support group attenders to less frequent attenders after surgery. Table 1 summarizes the support group information. In the six months after surgery, six of the postsurgical patients attended one or no support group sessions while four attended two or more. Some differences were seen between these two groups.
Tips for Providers
A limited body of literature exists on how to successfully run a support group for adolescents undergoing or who have gone through bariatric surgery. The following describes some of our experiences in developing such a program.
First, the support group is staffed by a member of the bariatric team, generally the pediatric psychologist and/or registered dietitian. The groups are held in the evening at 5PM, so as to not conflict with work, school, or other commitments. For consistency, we run support group on the same day of the same week each month. When patients and families enter our bariatric program, they are provided the dates for support group for the upcoming year. In addition, rules for attending a support group include but are not limited to; being on time, no cell phone use, and no sharing of personal information outside the current support group.
The topics of support group change each month. Some of the support groups are patient and family focused, where emphasis is placed on the group asking questions, describing challenges, and getting support from one another by sharing stories and experiences. Occasionally, support groups have clear topics that focus on engaging in physical activity (e.g., Zumba, Wii video games like Just Dance, Scavenger Hunts, and Dodgeball). Groups have also focused on improving food choices (e.g., taste testing new vegetables, a jeopardy style Nutrition 101 game) and others have focused on improving overall well-being (e.g., learning new relaxation strategies, sleep hygiene).
We have held support groups for those who want surgery and those that have had surgery simultaneously. Although the needs of these patients might be different, it has provided a good learning experience for presurgical adolescents and their families to know what to expect. Also, it has provided an opportunity for postsurgical adolescents to mentor those on the path to surgery. Support groups are held with the adolescent and their parent/caregiver together. When two staff members are available, on occasion, adolescents and their parent/caregiver are separated to allow for more individualized attention.
Finally, our six keys to running an effective support group are: 1) be consistent—have a set day and time; 2) be flexible on what is discussed in group but have a topic planned for times when no one will participate; 3) keep good records of who attended; 4) streamline topics but know that participants might change the topic; 5) invite the whole family to participate; and 6) have fun. Support groups are generally nonbillable activities that allow one to engage with families in activities that you might not be able to in your general provider role with families. To aid with attendance, particularly for patients and families who live far from our program or have limited transportation, we will schedule multiple appointments around a support group so they can limit their travel to our institution.
Discussion
Preliminary data in this small subset of patients shows that a support group for adolescents having undergone bariatric surgery can be a helpful tool in achieving successful short-term postsurgical weight loss. Adolescents who attended two or more support groups in the first six months after surgery lost more weight than those who only attended one or no support group sessions.
This is a similar finding to that seen in adults who have undergone bariatric surgery, where attendance at support group was related to increased weight loss. Additionally, less frequent attendees of support group tended to be older and have higher BMIs at baseline than those who attended two or more support groups. Sawhney et al14 found similar findings. Adolescents with higher preoperative BMIs were less likely to attend support group. This might highlight a subset of youths that warrant further clinical attention and services specifically, mental health services.
Limitations. This study examined a small population and future studies should examine these findings in a larger sample using varying bariatric procedures. More research is needed on the process of running successful support groups, identifying key components and examining which adolescents benefit the most from attendance and which may require other services. Finally, more research is needed in examining long term outcomes of support group attendance on variables beyond weight such as mood and improvements to eating behaviors.
Conclusion
In summary, this study provides preliminary evidence on a small subset of youth who underwent laparoscopic adjustable gastric banding surgery and found that attendance at a support group might have beneficial effects, including greater weight loss six months after surgery. Although this study examined a small subset of patients, it is critical that we examine the impact of additional support on the outcomes of youth following bariatric surgery. Even with a small sample size, changes in short-term (six-month) outcomes were seen. As providers, support group has given us a way to know patients in a less formal setting and be able to identify challenges with complying to postoperative behaviors and lifestyle changes.
References
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814.
- Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr. 2014;168:561–566.
- Humayon S, Altieri MS, Yang J, et al. Recent trends of bariatric surgery in adolescent population in the state of New York. Surg Obes Relat Dis. 2019;15(8):1388–1393.
- Avnieli Velfer Y, Phillip M, Shalitin S. Increased prevalence of severe obesity and related comorbidities among patients referred to a pediatric obesity clinic during the last decade. Horm Res Paediatr. 2019;92(3):169–178.
- Michalsky M, Kramer R, Fullmer M, et al. Developing criteria for pediatric/adolescent bariatric surgery programs. Pediatrics. 2011;128:S65–S70.
- Pratt JS, Lenders CM, Dionne EA, et al. Best practice updates for pediatric/adolescent weight loss surgery. Obesity. 2009;17:901–910.
- Austin H, Smith K, Ward WL. Psychological assessment of the adolescent bariatric surgery candidate. Surg Obes Relat Dis. 2003;9:474–480.
- Mechanick J, Youdim A, Jones D, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient – 2013 update. Surg Obes Relat Dis. 2013;9:159–191.
- Shen R, Dugay G, Rajarm K, et al. Impact of patient follow-up on weight loss after bariatric surgery. Obes Surg. 2004;14:514–519.
- Kaiser K, Franks S, Smith A. Positive relationship between support group attendance and one-year postoperative weight loss in gastric banding patients. Surg Obes Relat Dis. 2011;7:89–93.
- Orth W, Madan A, Taddeucci R, et al. Support group meeting attendance is associated with better weight loss. Obes Surg. 2008;18:391–394.
- Glinksi J, Wetzler S, Goodman E. The psychology of gastric bypass surgery. Obes Surg. 2001;11:581–588 .
- Pratt JSA, Browne A, Browne NT, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14(7):882–901.
- Sawhney P, Modi A, Jenkins TM, et al. Predictors and outcomes of adolescent bariatric support group attendance. Surg Obes Relat Dis. 2013;9:773–779.
- Santos M, Gaffka B, Mackey E. Patient retention and engagement in adolescent bariatric surgery programs: a review of the literature and survey of programs. Clin Pract Pediatr Psychol. 2017;5:52–61.
Category: Brief Report, Past Articles



